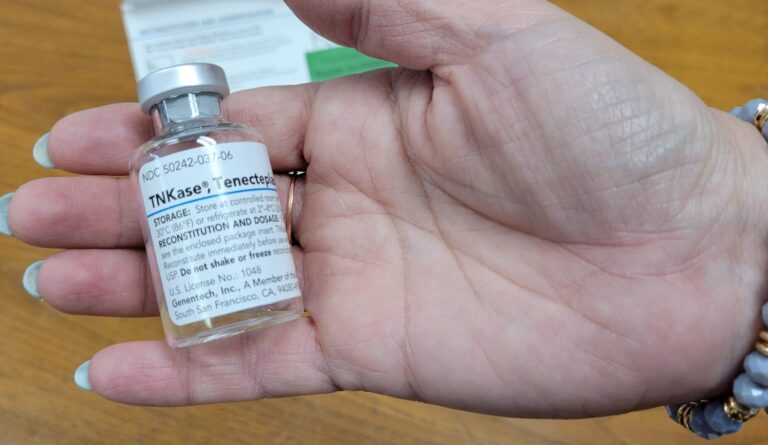
More hospitals are turning to a drug called TNKase — a brand name for tenecteplase — to break up the blood clots that threaten stroke victims. It ’s a less expensive and much faster acting drug than previous treatments. While it isn’t suitable for all patients (such as those suffering from bleeding in the brain) it can help avoid the brain damage of a stroke. But patients get the benefit only if they seek treatment quickly, within the first hours after a stroke occurs.
Nurse Leslie Ingold is the regional stroke coordinator for the OSF Healthcare hospitals in Urbana and Danville. She spoke to Illinois Newsroom’s Jim Meadows:
Leslie Ingold: We started on January 30, using a new to us, not a new drug, but tenecteplase. TNK or TNKase has been around for a long, long time. It treated patients for acute MI (myocardial infarction) . There’s lots of studies that had gone on over the years that showed that there could be a possibility that it would be a benefit to our stroke patients over the current gold standard medication that was being used, alteplase
Jim Meadows: And acute MI, I should say that’s heart attacks?
Leslie Ingold: That’s right, that’s a heart attack. So Danville (OSF Sacred Heart Medical Center) was using it for heart attack patients, to get them to Heart of Mary (the OSF hospital in Urbana).
Jim Meadows: What does this drug do?
Leslie Ingold: So this drug has a quicker injection time. The other drug, it took a while to mix … Then it was a drip that we hung up for an hour. This new drug is really just mix it and give it IV push over five to 10 seconds. So that makes the patient getting the medication quicker. The medication has a longer half life. For this drug, it has a half life of 20 to 24 minutes. So it’s going to work in your body longer. It has a better fibrin-specificity. So that means the drug seeks out those clots better, finds them and works on breaking them up quicker.
Jim Meadows: And it does it a lot faster than the previous drug being used.
Leslie Ingold: Right. Just by the nature of how fast we can give it and how quickly we can give it. It works, has better specificity, attacks them quicker, it can stay in there longer, and it has a reduced risk of bleeding for the patient because it is a blood thinner.
Jim Meadows: Is this something which has an improved impact on patient outcomes? Is this a game changer in any way?
Leslie Ingold: It really is a game changer. First we need the patients to come to the hospital quicker. This medicine can only be given if you come to the hospital within four and a half hours of your symptoms starting. Yes, it will be a game changer. But I need help from the public to come to the hospital quicker, so it can be a game changer for you.
Jim Meadows: It sounds like that’s a that’s a constant message that you’re trying to get out to the population of people who are at highest risk of strokes,
Leslie Ingold: Right. We’ve probably given it about ten times in both hospitals since January 30th. And a lot of people would think gosh, Leslie, that’s a pretty low number. The problem is, is we have a low number of patients to work with because they don’t come in that timeframe. And so it’s a sad opportunity that we could give them if they would have just — a lot of patients (think) I’m going to take a nap, it’ll get better, or I’m going to call my primary (care physician) and wait on them to call me back or it’ll go away soon, it’ll be fine. And so we really could have a better opportunity if patients came into the hospital quicker, we always want them to call 911. The ambulance can start treatment quicker than somebody driving them in a private vehicle.
Jim Meadows: Well, a patient may feel well something feels wrong, but I’m not sure what it is yet. I’m gonna see if it keeps on feeling wrong. How do you get from that to I need to take action now? And how do you know when to take action now?
Leslie Ingold: we use the mnemonic BE FAST. And if you can identify with any of those letters in the alphabet, you need to come to the hospital right away. So B is for balance. If you have a sudden acute onset of dizziness or you’re falling to one side or the other, I need you to call 911. E is eyes — double vision, loss of vision, unable to see on one side or the other. F — face. Somebody tells you you have a droopy mouth or a droopy eye, your speech is slurred. A — arms, stick your arms out like you’re holding a pan with the palms up. Close your eyes. And if one arm deviates and they don’t stay level and somebody sees that th,at’s a concern, too. S — I talked about speech when we talked about face. And T is time the four and a half hour window we need you to get to the hospital.