PORTLAND, Ore. — “Being a pathologist, but also a Black pathologist…it’s momentous to see this actually happening and at such a large scale,” Dr. La’Tonzia Adams said.
Adams is talking about the end of a long-running practice of using race-based testing for chronic kidney disease.
In the past, African Americans and other people of color were tested differently than their white counterparts, leading to poor healthcare treatment and increasing disparities in Black and Brown communities.
“Patients were appearing sick, very sick and they didn’t have the right eGFR. It was too high. So, they couldn’t get a transplant. Even though clinically, they met every other criteria, it’s just this particular one that they didn’t meet. So, they were denied that opportunity," she said.
Adams is a member of the College of American Pathologists and a pathologist at the Portland VA Medical Center, and she said she's seen firsthand how putting race into the equation has led to disparities in kidney treatment for Black people.
“It was one of those things that, unfortunately, when it gets into the health system, it’s hard to pull out. So, it was just never really addressed and corrected, and it just became mainstream thought,” Adams said.
eGFR (estimated glomerular filtration testing) is a blood test commonly used to assess kidney function. For years, Adams said, the equation for the test used race, sex, weight, and creatinine, a breakdown product from muscle and protein metabolism.
Here’s the problem: the inclusion of creatinine added racial bias to the formula. The myth that African Americans have more muscle mass, thus making more creatinine, added a multiplier for Black people.
“The problem with that is it made those that were Black seem that they had a higher kidney function or a higher glomerular filtration rate than their non-black counterparts,” Adams said.
That miscalculation has furthered disparities for Black folks in healthcare, preventing them from early interventions, treatments, and transplants, according to the College of American Pathologists.
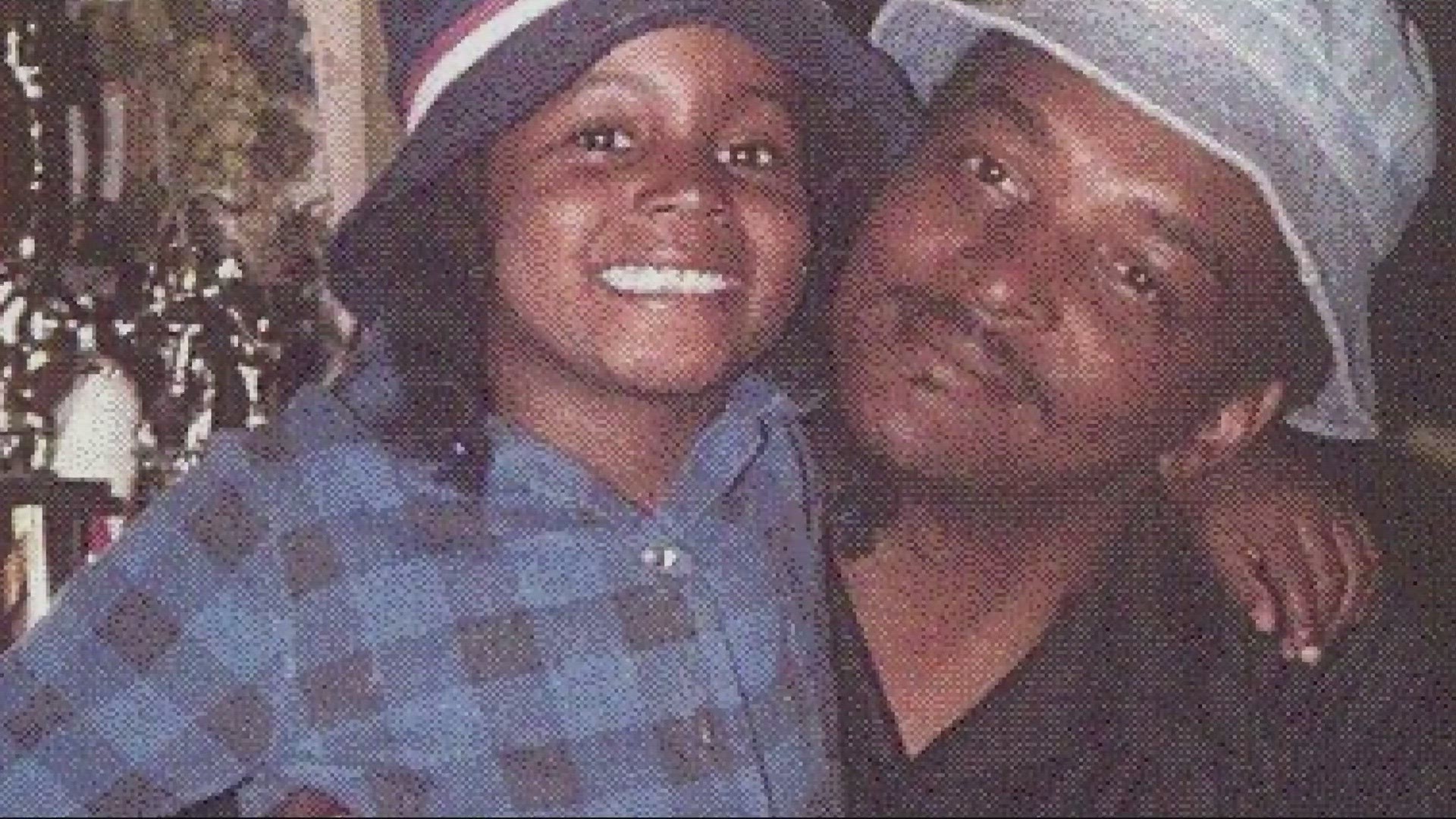
Adams has seen the negative impact of this race-based testing in her patients and even her own father. She lost him to kidney disease after it was diagnosed too late.
“He was very proud, very strong. Would do anything for you,” Adams said. “He was a Vietnam vet and a fireman when he came back from Vietnam.”
Her dad had the two most common risk factors for kidney disease: diabetes and high blood pressure. He also had a stroke.
He would go to the doctor regularly, Adams said, doing everything you’re supposed to do. They tried to get him seen by a specialist, but he couldn’t get a referral. Eventually, he got so sick, he needed to go to the emergency room. That's when they found out that his kidneys were failing.
“After doing those simple blood tests, one of them being eGFR, we were told that he was in end-stage renal failure and he needed emergency dialysis,” she said.
Their family immediately started looking into treatments. Adams was ready to donate her kidney to save her dad, but they never had the chance to get to that point.
“One of the things that they said was, he doesn’t qualify right now because he wouldn’t even survive the surgery. He doesn’t have enough reserve,” she said.
The College of American Pathologists says that’s an outcome for many Black Americans because of race-based testing for kidney function.
It is part of Adams’ job, and the work of other pathologists, to ensure providers are up to date on the change. She hopes this will prompt the medical community to address other ways racial bias has become common practice in healthcare.