Health officials are warning parents and school staff to look out for its signs and symptoms of strep A infections after several deaths among children.
While most people who get it will not become extremely sick, the highly contagious bacteria that cause the infection can, in some cases, cause serious illnesses, health complications and death.
What is strep A?
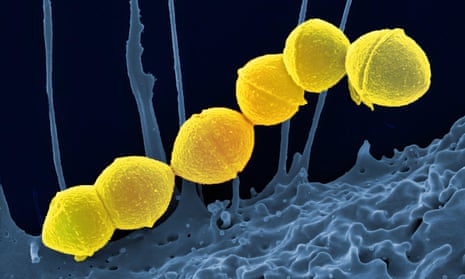
Strep A bacteria can cause many different infections. The bacterium is commonly found in the throat and on the skin, and lots of people have it without even knowing and do not come to any harm.
However, they can spread it to others who might become ill. People can catch it through close contact and from coughs and sneezes. Outbreaks can sometimes happen in places such as schools.
Most health issues caused by strep A are mild, but can range from minor illnesses to serious and deadly diseases. They include the skin infection impetigo, scarlet fever and strep throat.
What are the symptoms?
Strep throat is different from a regular sore throat and the pain can come on very quickly. Symptoms include pain when swallowing, fever and red and swollen tonsils – sometimes with white patches or streaks of pus.
The first signs of scarlet fever can be flu-like symptoms, including a high temperature, a sore throat and swollen neck glands.
A rash appears 12 to 48 hours later that starts on the chest and stomach, then spreads. A white coating also appears on the tongue that peels, leaving the tongue red, swollen and covered in little bumps, which is often called “strawberry tongue”.
Impetigo is a skin infection which starts with red sores or blisters that then burst, leaving crusty, golden patches.
Very rarely, strep A can cause severe illness when the bacteria get into parts of the body that are usually free from bacteria. This is called invasive group A streptococcal disease.
What is invasive group A streptococcal disease?
Invasive group A strep disease can become a life-threatening infection in which the bacteria have invaded parts of the body such as the lungs, blood or muscles.
Two of the most severe but rare forms of invasive disease are necrotising fasciitis and streptococcal toxic shock syndrome.
Necrotising fasciitis is also known as the “flesh-eating disease” and can occur if a wound gets infected. Signs of necrotising fasciitis include fever – a high temperature above 38C – severe pain and swelling, and redness at the wound site.
Streptococcal toxic shock syndrome is a rapidly progressing infection causing low blood pressure or shock, and damage to organs such as the kidneys, liver and lungs. Early signs and symptoms of toxic shock may include fever, dizziness, confusion, rash and abdominal pain.
after newsletter promotion
How can strep A be treated?
Strep A infections such as scarlet fever and impetigo are treated with antibiotics. After a full 24 hours of treatment, people are generally thought to no longer be contagious.
Anyone thought to have invasive group A streptococcal disease should seek medical help immediately. Antibiotics, other drugs and intensive medical attention are likely to be needed.
Why is strep A an issue now?
Public health officials said there was currently no evidence of a new strain circulating. The rise in cases and deaths was most likely to be related to high amounts of circulating bacteria and increased social mixing, they said.
“We are seeing a higher number of cases of group A strep this year than usual,” Dr Colin Brown, the deputy director of the UK Health Security Agency (UKHSA), said in a statement released on Friday evening.
“The bacteria usually causes a mild infection producing sore throats or scarlet fever that can be easily treated with antibiotics. In very rare circumstances, this bacteria can get into the bloodstream and cause serious illness – called invasive group A strep (iGAS).
“This is still uncommon, however it is important that parents are on the lookout for symptoms and see a doctor as quickly as possible so that their child can be treated and we can stop the infection becoming serious. Make sure you talk to a health professional if your child is showing signs of deteriorating after a bout of scarlet fever, a sore throat, or a respiratory infection.”
Microbiologists believe that reduced mixing among children over the last two years may have caused a drop in population-wide immunity that may result in the UK experiencing an increase in transmission, particularly among school-age children.