“A New Day”: DCH CEO Katrina Keefer Answers 20 Questions About Tuscaloosa Hospital System
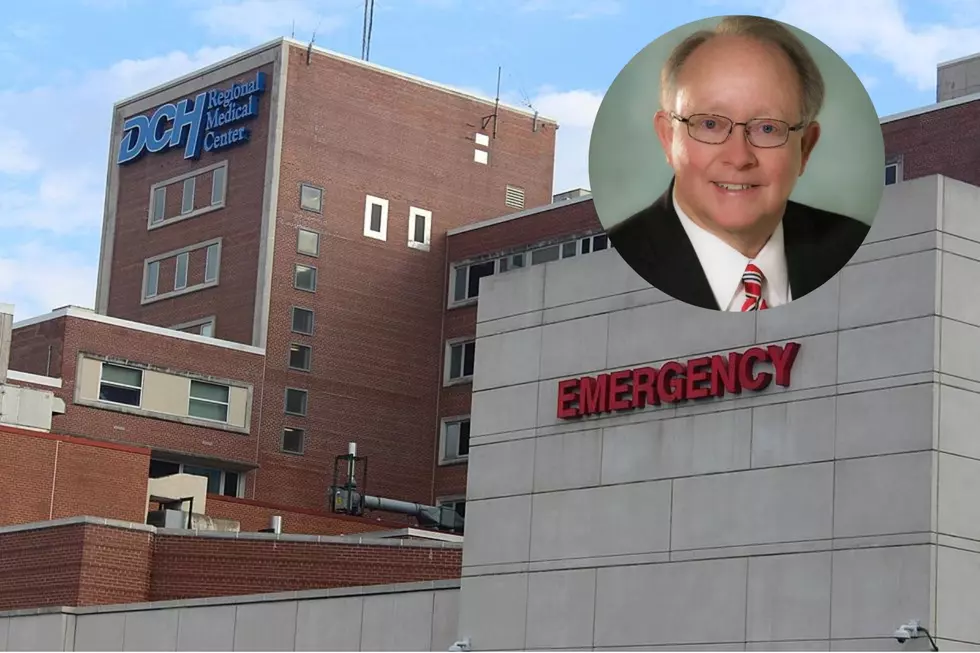
Katrina Keefer, the new CEO of the DCH Health System, said Friday morning that she knows the patient experience in their three hospitals needs to improve but is optimistic that better days are ahead.
Keefer, who started in this role at the beginning of August, and DCH's Vice President of Communications sat down with the Tuscaloosa Thread Friday morning for an hour-long interview. Keefer answered 20 questions, the vast majority of which have been transcribed below.
The questions and parts of her responses have been lightly edited for clarity and consistency, and the omissions denoted by ellipses in brackets reflect only irrelevant banter cut for the sake of the reader.
For answers about ER wait times, the possibility of partnership with UAB or the University of Alabama, employee morale within the hospital and much more, read through the Q&A below.

Q: Tell me about taking this job. What made DCH attractive to you, what made you decide you wanted to leave Augusta and set up shop in Tuscaloosa to lead this system?
KEEFER: Coming to DCH is really coming home to Alabama, and it's coming to a health system with great potential and I really am looking forward to the challenge of rebuilding its reputation and loving its caregivers and building bridges back into the community.
I've never lived in Tuscaloosa but it's been fun to watch from afar, both from Montgomery and from Birmingham. I'm a big Alabama fan, so I've been here for many Gamedays, but as the University has continued to develop and with all that Tuscaloosa is becoming -- I'm excited about being a part of that.
Q: One of the first major stories we wrote about DCH this year was about a leaked internal email about projections of major financial loss for this system, up to $60 million in losses this fiscal year, which meant no merit raises for System employees. Where does the System stand now? Did the situation improve or get worse?
KEEFER: The financial situation has improved from that time. The caregivers really stepped up and worked hard to manage expenses and did so successfully. [Patient] volume has continued to return, which has driven some of the revenue but really the expense management by the leadership here has materialized into less of a loss projected for the end of the year. The numbers bounce around with the close of each month, but July was a good month. We're on track to cut that [projected loss] by probably a third at the year-end. But until we get to an audited financial statement, it doesn't really matter.
As it relates to raises, we did raise our entry-level wages from $10 to $14 dollars at the first of this month to stabilize many of our support services. We likely will not be giving merit raises for [this] year, but we're continuing to evaluate all of the pockets of our workforce to ensure that we're stabilizing our workforce, which will lead to better care for our patients.
Q: Both at the Chamber of Commerce of West Alabama's Next Level Summit in April and at their State of the Community event earlier this week, Tuscaloosa Mayor Maddox has raised concerns about the long-term financial viability of the DCH System. Maddox talks a lot about other health care entities that have closed down in West Alabama, and how that leads to DCH becoming a "drainage basin" for more indigent people coming from a much wider area, but the System doesn't ever really see revenue from those patients and you don't turn any patients away. Has he got a good grasp on that issue and how it affects the system?
KEEFER: Well, I really don't like the term 'basin,' but that is a catch-all and that's what Safety-net hospitals are. We're a Safety-net hospital and I think many of our caregivers are proud of that, and I think our community is proud of the fact that we don't turn others away. I think that we need to partner with other resources in the community to think about how we help patients stay closer to home. What are the resources in those regions?
It's hard to make a living in a hospital and the smaller hospitals and smaller facilities are going to have trouble making it if we can't figure out ways to work together for different care models to get patients in the right setting in the right situation. I've had success in other markets with chronic disease management, managing people outside of the four walls of the hospital to keep them out of the emergency room, to keep them healthy and learn how to manage their chronic disease, which is really a lot of what we see from outlying areas that land in our emergency department. So I think we really need to get away from the 'basin' discussion and really talk about the Safety-net nature of who we are and own that, but really let that be a positive anchor for West Alabama instead of the negative connotation that seems to come with that rhetoric.
Q: Even as some leaders say DCH is in bad shape because other health care facilities have closed in the region, some of those same parties are saying DCH is in bad shape because UAB is going to open the Medical West Hospital Authority in McCalla in 2024. You spent 17 years in the UAB System -- what are your thoughts on the new facility coming to McCalla? Is it a threat to DCH, or will it be an asset to have another hospital in West Alabama?
KEEFER: I think we've got a couple years where we really need to ensure that we're stabilizing our workforce. [The new hospital] is going to be the new shiny object down the road, but we need to ensure that we are providing high-quality care and that we have a culture here where our caregivers want to stay home, where they want to care for their friends and neighbors here. It will be interesting to see how it changes the dynamics in the market, but I really see Medical West more as a Birmingham facility than a Tuscaloosa facility. I think of it in terms of volume that is leaving to go to Birmingham more so than it really being 'next door' to us.
Q: When Maddox talks about the problem of financial viability, the proposal he has put forward time and time again is a partnership with or acquisition by the University of Alabama System or the UAB Health System. With your background at UAB, some people have assumed you were brought on to oversee that kind of partnership or acquisition. Can you talk a bit about what that might look like?
KEEFER: It's interesting because you preface the question by saying the mayor has always put a proposal on the table with either the UA System or UAB -- those two things would look very different. There hasn't been a true proposal, there have just been discussions and I do think those are premature.
I stay close to all of those people and understand where their Systems are heading -- UAB Health System is going through a leadership transition right now as well, so their new leader may or may not feel the same way as prior leaders have about partnerships -- but we're always looking for partnerships. I think we have a world of opportunity on the research side to think about how we apply new models of care to rural areas. That is a national topic of discussion and I think a place that we could truly use this as an incubator to talk about how we keep health care local, how we put together all of those partnerships.
[...]
I'm certainly open to all of those things but to rush to give somebody the keys, I think, is very premature and I think it really will hinder our ability to get a strong footing with the rhetoric that's out there.
I'm going to meet with [Tuscaloosa Mayor Walt Maddox, Probate Judge Rob Robertson and Northport City Administrator Glenda Webb] this afternoon. I'm really looking forward to that, continuing to get to know them and developing our personal relationships and talking through what it is it that we're really trying to accomplish together.
[...]
Let's say there's a physician coming to town -- they either want to practice in a community setting or an academic setting and they aren't going to come to a community setting if they think it's going to turn into an academic setting in two years. That'll be about the time their practice gets established and then it would get turned upside down.
If we can just tamp down and be a strong community health system for West Alabama, we can continue to think about those other things but not let that be what drives the discussion -- what really needs to drive the discussion is the high-quality health care provided by our caregivers here in West Alabama.
Q: Where Maddox has talked a lot about the financial viability problems, Judge Robertson has talked a lot about emergency room wait times and how an ambulance waiting to get someone admitted into the ER is not in service, about how that wait can be hours long. Can you talk about the root cause of the ER wait times and how you address them?
KEEFER: They call it 'wall time,' when the ambulance service is waiting to hand off [a patient.] I think the team here has taken an approach to try to get that handoff done more quickly and I think those times have likely already improved but that has been at the expense of pulling people from the waiting room back into a room. I've challenged the team in my first couple of weeks here -- we're really studying our geography and how we utilize the space that we have in the emergency room. There are too many people in the halls. There are too many people in the corridors. It is not acceptable and we are really owning that, taking incremental, sustainable steps to improve wait times, but particularly [improving] our patients' experiences in the emergency room as well as the length of stay upstairs and getting patients discharged. There may be a better discharge lounge concept that we might be able to use. The System did a great job of making space when needed for COVID and many of those patient areas are still available. We really need to think about how we utilize that space, how we staff that appropriately with the right caregivers. That's the first puzzle that the board and the public expect me to solve.
Q: When you look at the problem, at long ER wait times and the patient experience, is the core of the problem the number of available staff? Quality of staff? Is it the length of the shift those caregivers are working? Have you identified the root cause that creates this patient experience that you said you don't find acceptable?
KEEFER: It's all of those things, other than quality of staff. I would not let that one fall in there. It's the mix of staff [shortages], the geography that they have been given, the patient flow and the way patients are called back and seen and triaged -- our patients that come into the emergency department are triaged and seen quickly, but it's getting them that follow-up care when they have to sit in the waiting room. And really, if they have to sit back in the waiting room for a very long time, did they need to be in the emergency room? We really need to study how we keep those folks out of the emergency room. How do we get them followup appointments with perhaps a primary care physician or a specialist in the office on a following day?
There's no one single root cause and really studying who the patients are, where they're coming from and how we partner with community resources to try to address that outside of these walls while improving patient flow and working with the nurses as we're also working with our physician partners in the way that they are seeing patients -- it's a big Lego set to put together and it's got to be put together in the right way so that it's not knee-jerking.
I think before the answer has been 'Oh, it's hard,' or 'Oh, it's staffing' or 'Oh, it's length-of-stay upstairs," and none of those answers are acceptable. We have to start making incremental, sustainable steps and I will own that.
Q: You've got three hospitals in the DCH Health System in Tuscaloosa, Northport and Fayette. Do they present unique challenges? Would a step taken or policy implemented at one also be applied at the other two?
KEEFER: They are all unique. They all have their own personality. There's a sense of pride within each of them. [...] I think that we can learn a lot from Fayette, they do very well in their patient experience scores. They do very well in many of their quality metrics. They are a smaller facility and they offer different services than Regional or Northport might but each of them have their own personality and it's good to honor that but when you're trying to be efficient in the back office and apply Systems thinking, it's a delicate balance to ensure that we're honoring the sort of local flair and identity while ensuring that the processes are consistent across the board.
Q: We've heard a lot from Northport City Administrator Glenda Webb regarding concerns with the DCH System's board of directors and transparency from that board, but also heard this summer that steps had been taken to improve that transparency. Those conversations may have taken place before you took over as CEO, but can you comment on those developments at all?
KEEFER: Yes, before I occupied the office, the board relaxed some of the [confidentiality] requirements, but my approach has been a transparency pledge. I have spent time with Glenda and she is arranging for me to meet with several City Council members next week, so I'm really looking forward to having that direct interaction with them.
Their appointee to our board [David Albright] should not have to carry DCH's detailed message and it's important to me to understand what is it that they really want to know for their constituents instead of getting wrapped up in who signed an NDA and who didn't.
[...]
Boards talk about confidential things and I trust that Dr. Albright can judge that appropriately but I really want to work with Glenda and the folks in Northport to ensure that we are being responsive to them and understanding what their real concerns are because it probably has a lot more to do with health care for citizens than it does non-disclosures and boards and we just really need to talk about what is it that we're doing that is helpful to them and for them and what we need to do to improve the experience for them.
Q: We've talked a lot about external perception of the DCH System, but there are also a lot of conversations about issues internally and morale within the hospital staff. How do you turn that around for the people who work in this building, in Northport and in Fayette and assure them it really is a new day and it's worth sticking around?
KEEFER: I think that we kicked that off in a major way earlier this week at our Health System management team meeting. It's culture, culture, culture and it's appreciating people for the work that they do. It's encouraging them to work in teams. It's encouraging them to communicate with each other. It's requiring a culture of safety, requiring a culture of compliance, requiring a culture of accountability. Many of the caregivers that are here have been yearning for that. I think there's a new energy in our folks because they feel like we can do this together. I gave them permission to go back to taking care of patients and said I would take care of the noise. The noise has been disruptive to them and their families. You know, these are people who come to work every day and hear their workplace trashed in the news and that's not helpful. That doesn't help us with recruiting and retaining the best and brightest. So I really want to ensure that we've got the right leaders in place to really promote the culture change that has to occur here so that we can stabilize the workforce.
Q: Have you identified those places where a change in leadership is needed?
KEEFER: I'm putting together the skill sets that I think are lacking from the existing leaders and also trying to get to know the next level of leaders. I love to grow from within but sometimes you need a shot in the arm from outside, so I'll be putting that together hopefully over the next 30 days so we have ourselves organized for the work that we need to do.
Q: Your predecessor as CEO, Bryan Kindred, has stayed on with the DCH System as an advisor and that's drawn a lot of attention. Can you talk about what you expect to rely on Kindred for? What will that role look like and what advice do you expect to seek from him?
KEEFER: Bryan and I met one day during my second week as CEO and we'll meet one day next week. He has not been on campus but does come to my office and share with me things that may still be coming to him -- I've known Bryan a long time and he's been a friend.
ANDY NORTH: From my perspective on that one, Bryan has really -- as he was leaving, he said 'I plan on staying out of the way and if Katrina needs me, if she has any questions, I'm happy to help but she's got the plan and I fully support her doing whatever she needs to do.'
Q: I want to give you time to talk about your own vision and optimism. There have been a lot of negative stories out of and about the System recently and I suspect you wouldn't have taken this job if you didn't believe you could turn things around. Talk about what excites you, what's working well. Where are the bright spots you can point to?
KEEFER: I'm excited about changing the narrative about DCH and working with our caregivers here to tell the good stories.
Everybody talks about a D in LeapFrog, but they're not talking about the US News & World Report's List of Top Hospitals. There were only four in Alabama and DCH was among them, behind UAB, Huntsville and St. Vincent's.
There are good things going on, but we don't want to get hung up on any one metric, any single recognition, but instead focus on telling those good stories and building bridges to the community, to the business community, to the elected officials, to our medical staff. We want to take all of the good that Tuscaloosa has to offer and really let that be an opportunity to recruit and retain the best and brightest.
I know that with a culture change within the walls and with our caregivers feeling good about the care that they are providing, this will be a place that people want to work. I am confident that local folks who have gone -- perhaps a traveling nurse might have gone to take a 13-week assignment in Montgomery -- when she gets done with that assignment, I want her to want to practice here. I think that we can create an environment over time to do that. I think we can take immediate steps to
work through wait times in the emergency department.
We realize there are things that we do here that we don't promote well. We need to be in our referring physicians' offices ensuring that they know the kinds of care that we can provide. We're also studying the kind of information that we can give back to referring physicians so when they send their patients to us, they get the best information back.
There's a world of opportunity. There's so much good that is here that could be built on and I'm just proud of the team that has held it together and I'm really looking forward to the future.
Q: As you talk about the future, is there any specific measure or step coming soon, with a concrete ETA, that you want to point to? Or is that too deep to drill down so early in your tenure?
KEEFER: I would like to be able to present some of those goals to the board at our next meeting and really work with them on tangible, incremental goals and then be able to share those with the public. Then we hold ourselves accountable to meeting those. The board has been very clear that they want me to work on establishing a leadership team that is ready to lead the culture change. They've been clear that assessing patient care and the quality of care needs to be addressed immediately. Many of those charges that I have from them, I'm beginning to outline in a way that I'm hopeful is appropriate for them and that they will endorse so we can share plans with the public and be able to celebrate victories along the way.
Q: The board has not been left out of conversations about conditions at DCH, especially those with long tenures of service. Are the current board members the appropriate leaders to get things moving in the right direction and achieve better results for the community? Are you confident in those nine board members?
KEEFER: I am confident in them. I think we've got the right board at the right time. Chairman [Jim] Harrison is the new leader after the Judge [Joseph Colquitt] had been chair for a long time. With [Colquitt] having served a long time and [former CEO] Bryan Kindred having served a long time, we really have turned a corner on a new day. I really think that the board has individual competencies that can contribute to this next chapter and to guide the way. Individually, I really like them and collectively I think they're a great board.
Q: We've talked a lot about the promise of this next chapter. What are some of the challenges or obstacles you anticipate? Finances? COVID and its variants? Monkeypox?
KEEFER: Workforce Development. My answer to that question, on a lot of levels, is probably the same as any large employer in the region. I just hire one of every kind of person, whereas a manufacturer may just hire line workers and engineers. Stabilizing the workforce is going to be critical to our success.
We also need to shift from pandemic thinking to endemic thinking as it relates to COVID -- COVID is not going to go away. We need to just learn to live with it and how that flows through the way that we welcome our patients and their families and make that part of everyday life here.
There are always going to be unexpected circumstances, so for those things that can't be anticipated, we've got to have a leadership team together that understands how to pivot quickly. With lots of unknowns in the world we live in, we'll we'll take them as they come.
Q: Is there anything you want to make sure we talk about? Anything on your mind or a message for our readers, if you could talk to them directly?
KEEFER: I would say give us a chance. Give our caregivers a chance to prove that the negative perceptions that are out there are not going to be our reality. I'm going to wake up every day, and our teams are going to wake up every day, and work really hard to earn that trust.
[...]
I look forward to building bridges within the community, with the elected officials, with our caregivers direct and indirect and making DCH the best it can be.
Q: Your first day was August 1st -- has anything really surprised you since then? Is anything much better or worse than you expected?
KEEFER: I think the welcome that I've received -- I knew that people would be nice, but people seem genuinely over the top excited about the next chapter.
[...]
I don't know that I've been especially surprised in a negative way. Nothing surprises me because in a hospital, you can't make up the things you see. When you've been working in leadership in hospitals for 20 years, not much surprises you.
Q: Speaking of that level of experience, you spent 17 years in the UAB Health System. What lessons learned there, if any, will apply here at DCH?
KEEFER: Much of what I learned from the UAB Health System that will be applicable here was when I was spending time serving in the Chief Financial Officer role for the Healthcare Authority for Baptist Health -- an affiliate of UAB Health System in Montgomery. Baptist Health is very similar to DCH in that they have three hospitals that are all different with their own unique personalities. Ensuring that we segregate services and align them in the background while letting each of the facilities really own their own identity -- that probably will be very helpful.
Much of the chronic disease management work that we did and thinking about care transitions and the full-care continuum will be very helpful.
We also did a lot of work with simulation and teaching people to work in teams, in high-reliability organizations. We really focused on zero patient harm and being a high-reliability organization, taking lessons learned from the airline industry, from the nuclear industry about getting to zero harm and having redundant systems.
The other piece from the UAB Health System -- when I was serving as treasurer, I was really their voice to the market. I did the transaction work, the bond work, whether it was new bond issues or restructuring -- when we went into Montgomery, they were technically in default on all their debt, so that was interesting. I was the voice to the market and to the banks for Medical West who, at the time, was not very strong and for Baptist as it went from being in default to being very financially successful and growing as a University of Alabama hospital, which of course UAB medicine is very strong in the market.
Also learning to talk to different constituencies and the different strengths of different kinds of health systems really helped me quite a bit and also informed much of the work that I did at Augusta University Health System, which is of course the teaching health system associated with the Medical College of Georgia.
For more coverage of the DCH Health System, Keefer's time at the helm and more, stay connected to the Tuscaloosa Thread.
Top Stories from the Tuscaloosa Thread (8/8 - 8/15)
More From 105.1 The Block