Abstract
Two and a half years into the COVID-19 pandemic, we have gained many insights into the human antibody response to the causative SARS-CoV-2 virus. In this Review, we summarize key observations of humoral immune responses in people with COVID-19, discuss key features of infection- and vaccine-induced neutralizing antibodies, and consider vaccine designs for inducing antibodies that are broadly protective against different variants of the SARS-CoV-2 virus.
Similar content being viewed by others
Main
Since its initial outbreak at the end of 2019, COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread across every continent. By the end of February 2022, there were more than 400 million confirmed cases and the disease had claimed more than 5.9 million lives worldwide (World Health Organization COVID-19 dashboard; https://covid19.who.int). The world has seen development of highly efficacious COVID-19 vaccines and promising antiviral small-molecule and antibody drugs with an unprecedented speed1. From a clinical perspective, while completely asymptomatic SARS-CoV-2 infection is not uncommon, 30–50% of infected individuals show progressive respiratory involvement, including interstitial pneumonia2,3. In a subset of infected individuals, acute respiratory distress syndrome (ARDS) and severe inflammatory response syndrome (SIRS) develop, potentially accompanied by microvascular and macrovascular thrombosis that may eventually lead to death4,5,6. While pneumonia is largely a consequence of cytopathic injury by the virus7, inappropriate and exaggerated host responses to the virus contribute to ARDS and SIRS5,8. As COVID-19 has become the single most studied human disease in history, unprecedented global efforts are being devoted to understanding how the host develops innate and adaptive immune responses to the SARS-CoV-2 virus and how the immune system helps control infection and transmission or, in certain cases, becomes dysregulated, causing tissue damage, organ failure, or death of the host. These efforts not only help to identify immunological correlates of infection- and vaccine-induced protection, but also facilitate development of treatment strategies for severe COVID-19 immunopathology.
The antibody response is an important arm of adaptive immunity against viral infection. On the basis of predominant isotypes and the profiles of somatic hypermutations of the resulting antibodies, the humoral immune response to viral infection or vaccines can be broadly divided into two phases. In the extrafollicular (EF) phase, B cells are activated to rapidly differentiate into plasma cells in foci outside of the follicle within a few days after infection9, producing antibodies that contain few somatic hypermutations but that can nonetheless be of reasonably high affinities and able to neutralize the virus10. These EF plasma cells are predominantly of the IgM isotype following protein-antigen immunization, but they can be IgG- or IgA-switched, particularly in response to viral infections. In either case, EF plasma cells are thought to be relatively short-lived. In the germinal center (GC) phase, which takes several days to a week to begin but can last for months, antigen-specific B cells undergo somatic hypermutation and affinity-based selection to give rise to predominantly isotype-switched and high-affinity plasma cells that establish a long-lived compartment localized in the bone marrow. Both EF and GC responses produce antigen-specific memory B cells that may persist long after primary infection is cleared11.
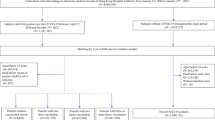
Almost everyone with SARS-CoV-2 infection seroconverts within 2 weeks post-symptom onset (PSO), producing IgM and IgG antibodies that predominantly recognize the viral spike and nucleocapsid proteins12,13,14,15. However, high serum titers of total or neutralizing antibodies against SARS-CoV-2 are more frequently found in severe cases of COVID-19 and do not necessarily correlate with better disease outcomes of the primary infection16,17,18. Transfusion of convalescent plasma was initially reported to be able to reduce the mortality rate of people hospitalized with COVID-19 (refs. 19,20), although increased survival was not replicated in a subsequent large controlled trial21. Neutralizing antibodies that block angiotensin-converting enzyme 2 (ACE2)-dependent viral entry into host cells correlate well with efficacy of prophylactic vaccines22. Serum levels of neutralizing antibodies to SARS-CoV-2 peak within the first few weeks after infection or vaccination and decline subsequently23,24,25,26,27,28, leading to reduced protection and an increased risk of re-infection by the original strain or newly emerging variants of concern or interest (VOCs or VOIs). Vaccine booster shots can induce broader and more potent neutralizing antibodies in patients convalescing from COVID-19 compared with previously uninfected individuals29. Antibodies that are cross-reactive because of previous exposure to other pathogenic and seasonal coronaviruses may affect the development of SARS-CoV-2-specific neutralizing antibodies as well30,31,32. What emerges from these and other studies of humoral immunity to SARS-CoV-2 is the importance of the timing and context in which B cell activation and antibody responses are initiated and maintained (Fig. 1).
Overview of the B cell and antibody response to SAR2-CoV-2 infection in the human system. a, Once activated, the extrafollicular (EF) response is rapidly launched. Some B cells differentiate into either short-lived plasma cells to serve as pioneers fighting against SARS-CoV-2 infection or memory B cells with few mutations, or they participate in the germinal center (GC) reaction. b, Through the GC response, B cells gain affinity-increasing immunoglobulin (Ig) gene mutations and potentially differentiate into either long-lived plasma cells to secrete high-affinity neutralizing antibodies and help maintain anti-SARS-CoV-2 antibody levels in serum or memory B cells with higher mutation frequencies and increased longevity. These differentiated B cells and plasmablasts migrate to different inflammatory sites to function (c–e). c, In blood vessels, memory B cells join the circulation system in surveillance, and plasma cells migrate to inflammatory sites to fight against infection. Other antibodies, like cross-reactive antibodies secreted by other viral-infection-induced plasma cells, contribute to the clearance of SARS-CoV-2. Auto-reactive antibodies may increase following SARS-CoV-2 infection in blood and potentially harm other healthy tissues by inducing autoimmune diseases. d, In mucosal sites, especially in nasal tissues, dimeric IgA protects from SARS-CoV-2 invasion and re-infection. e, In the bone marrow, long-lived plasma cells reside and help maintain anti-SARS-CoV-2 antibody levels in the host.
The serum antibody response in SARS-CoV-2 infection
Similar to other respiratory infections, SARS-CoV-2 infection stimulates rapid production of IgM, IgG and IgA antibodies, which are measurable in the sera as early as a week PSO, including those that bind to nucleocapsid and the spike protein12,13,14,15,24,25. The rapidity of such responses suggests that the antibodies have an EF origin33. Neutralizing activities toward pseudotyped or live SARS-CoV-2 also appear rapidly in these antibodies; this activity is readily detected in convalescent sera, although levels of neutralization achievable vary greatly among individuals16,23,27,34. This variability may partly explain why plasma therapy attempted early in the pandemic produces mixed results1.
Cross-section and longitudinal studies indicate that ELISA titers and neutralizing antibodies against SARS-CoV-2 peak in 3 to 4 weeks PSO23,24. While levels of these serum antibodies do decay25,26,27,28, they can be relatively stable for months, with IgG being more stable than IgM and IgA antibodies18,23,24. These kinetic features are consistent with a gradually increasing contribution by a more long-lasting plasma-cell compartment beyond continuous recruitment of EF plasma cells.
While COVID-19 severity varies greatly among individuals following SARS-CoV-2 infection, higher titers of ELISA and neutralizing antibodies are found in individuals with severe COVID-19 than in those with mild disease18,28,35 or those without symptoms36. Because severe disease is more likely to start with a high viral load, as suggested by a survey of studies involving more than 10,000 participants in total37, the elevated level of antibodies in severe cases probably results from much stronger antigen-driven EF response33.
Mucosal antibodies in SARS-CoV-2 infection
Plasma neutralizing antibodies are the best predictor of vaccine-induced protection from infection22. However, although antibodies in circulation or tissues help control viral spread within the body, mucosal antibodies, and particularly secretory IgA, in the respiratory tract may play a more prominent role in preventing transmission of SARS-CoV-2 through the airway38. This protection is based on strategic tissue distribution and the more potent neutralizing activity of dimeric secretory IgA than monomeric serum IgA and antibodies of other isotypes39. Indeed, virus-specific IgA is detected in saliva from infected individuals24. Neutralizing IgA antibodies in nasal fluids have been found in seronegative healthcare workers, suggesting a strictly local response in the nasopharynx-associated lymphoid tissue40. Significant levels of SARS-CoV-2 antibodies, including neutralizing IgA, remain in nasal fluids for months PSO41,42. Presumably, these antibodies contribute to reduction or resistance to re-infection.
Cross-reactive antibodies
SARS-CoV-2 shares 79% and 50% genome sequence identity with SARS-CoV and MERS-CoV, respectively, including the coding sequence for the receptor-binding domain (RBD), the main target of neutralizing antibodies43,44. Sequence homology between SARS-CoV-2 and other human coronavirus is lower, but remains immunologically relevant. In principle, recall of cross-reactive memory B cells that are produced during prior coronavirus infections may contribute to the rapid EF antibody response (IgG and IgA in particular) following primary SARS-CoV-2 infection45. Previously, SARS-CoV-specific antibodies isolated from people with SARS have been found to cross-react with human coronaviruses 229E and OC43 (ref. 46). Antibodies that can cross-react or cross-neutralize SARS-CoV and SARS-CoV-2 have been observed47,48,49. IgG antibodies that bind to SARS-CoV-2 spike proteins have been detected in blood drawn from healthy donors before the COVID-19 pandemic50,51, probably due to cross-reactivity to the human coronavirus (hCoV) that causes common cold52. Indeed, studies of uninfected cohorts in Canada have uncovered antibodies that are cross-reactive to SARS-CoV-2 spike and spike proteins from hCoV HKU1, NL63 and 229E, but not OC43 (ref. 53). In sub-Saharan Africa, pre-existing serological cross-reactivity to SARS-CoV-2 spike and nucleocapsid has likely resulted from exposure to hCoV NL63 and 229E54. These cross-reactivities are likely due to antibodies targeting to the highly conserved S2 domain of the spike protein, as the S1 domain is much less conserved in comparison, likely owing to strong selective pressure exerted by the immune system30,31,32. High levels of pre-existing cross-reactive antibodies tend to correlate with milder clinical manifestations after SARS-CoV-2 infection in some studies50,51,55, but not others52. Interestingly, people who show seroreactivity to hCoV OC43 spike protein do not have detectable cross-neutralizing antibodies against SARS-CoV-2 (ref. 56). Given the fact that pre-existing cross-reactive T cells are prevalent among people who have not been exposed to SARS-CoV-2 (refs. 57,58), the impact of cross-reactive cells is likely a significant variable in shaping the clinical outcome of SARS-CoV-2 infection59.
Auto-reactive antibodies in SARS-CoV-2 infection
It is not uncommon for viral infections to lead to increased generation of autoantibodies, in part because of inflammation, cell-death-related autoantigen release, and molecular mimicry60,61, although overt autoimmune disease does not necessarily ensue. SARS-CoV-2 infection leads to a marked increase in circulating autoantibodies targeting a wide range of autoantigens, including complement proteins, cytokines, chemokines and surface proteins62. Autoantibodies that recognize, and even neutralize, type I interferons, the very cytokines critical for orchestrating antiviral defense, have been identified in some people with COVID-19 and are strongly implicated in promoting life-threatening disease63,64, because severe COVID-19 is often characterized by diminished interferon production65,66,67.
Independent studies have also revealed a spectrum of antibody-driven autoimmune conditions following SARS-CoV-2 infection, including systemic lupus erythematosus68, Guillain–Barre syndrome69,70, and cold agglutinin syndrome71,72, pointing to a likely scenario that de novo autoimmunity is a significant contributor to severe COVID-19 (ref. 73).
The GC response in SARS-CoV-2 infection
Whereas the EF response gives rise to neutralizing antibodies, it is probably not sufficient for controlling SARS-CoV-2 infection33. Furthermore, prevention of re-infection depends on persistent neutralizing antibodies with increased affinity and long-lasting humoral memory in the form of memory B cells and long-lived plasma cells, which all require robust primary GC responses. However, the virus-specific GC response is difficult to assess directly in people, except for during autopsies of the deceased. Initial observations from autopsies of deceased people with COVID-19 show a surprising lack of anatomically identifiable GCs in lymph nodes or spleen74,75. Severe COVID-19 can be accompanied by severe lymphopenia76,77,78. It is likely that severe disruption of immune functions abrogates the GC response in those cases.
In people with non-severe COVID-19, analyses of antibodies, memory B cells and plasma cells over a period of months after infection revealed classical GC-dependent features. Although antibodies expressed by memory B cells isolated early after infection may carry relatively few mutations79,80,81, the spike- or RBD-specific memory compartment continues to evolve and turn over in the subsequent months, after which antibodies are expressed that show greater somatic hypermutation82,83 and increased neutralizing potency and breadth84,85,86. Spike-specific plasma cells have been found in bone marrow aspirates a year after SARS-CoV-2 infection, and their abundance correlates with serum spike-specific antibody titers87, indicating formation of a long-lived plasma-cell compartment. SARS-CoV-2 infection induces robust T cell responses, including spike-specific CD4+ T cells of the follicular helper phenotype that is capable of promoting antibody response57,88,89,90. In a rhesus macaque (Macaca mulatta) model of SARS-CoV-2 infection that recapitulates moderate disease in humans, primary infection clearly triggers GC formation, leading to protection from re-infection91,92. Finally, in a rare analysis of SARS-CoV-2-seropositive organ donors, virus-specific GCs have actually been found in the lung-associated lymph nodes 6 months after infection93. In combination, these studies indicate that SARS-CoV-2 infection induces functionally robust GC responses that may last for months, potentially owing to antigen persistence82. In addition to de novo GC responses from naive B cells, it is likely that cross-reactive memory B cells generated during previous exposure to seasonal coronaviruses are recruited to participate in the GC response to SARS-CoV-2. This possibility is supported by the fact that antibodies against S2, highly conserved among human coronaviruses, tend to have higher levels of somatic hypermutation than contemporary RBD-specific antibodies following SARS-CoV-2 infection31.
Although a persistent GC response may not be essential for controlling primary infection, with its continuous output of memory and plasma cells of increasing affinity and neutralization breadth and potency against SARS-CoV-2, it is a required component of, and arguably the best correlate for, a good prophylactic vaccine strategy.
Features of S glycoprotein and antibody neutralization
Spike proteins on the surface of SARS-CoV-2 viral particles and infected cells are the major target of neutralizing antibodies. Each matured SARS-CoV-2 virion contains, on average, 26 ± 15 (mean ± s.d.) spike trimers, covered extensively by glycans and randomly distributed on the surface94. For each monomeric S glycoprotein, there are two functional subunits: the S1 subunit, for binding to the receptor ACE2, and the S2 subunit, for mediating fusion of viral and cellular membranes (Fig. 2a). The S1 subunit folds into four major structural domains, the amino-terminal domain (NTD), the RBD, and two carboxy-terminal domains (CTDs), which wrap around and protect the inner S2 subunit. Antibodies predominantly neutralize the virus by blocking S protein from binding to its receptor ACE2 and interfering with the subsequent steps that are required for membrane fusion. Many RBD-binding antibodies can trigger S1 shedding, suggesting that they also neutralize the virus by mimicking ACE2 to induce premature conversion to the post-fusion conformation95. Cryo-electron microscopy and crystal-structure analyses have revealed that the RBD undergoes spontaneous structural fluctuation between an ‘up’ and a ‘down’ conformation. Only the up conformation enables the exposure of the receptor-binding motif (RBM) of the RBD, which can then become accessible and bind the host receptor ACE2. The up conformation is believed to be less stable, potentially explaining why the dominant trimer state has only one of the three RBDs standing up96,97. Although all these domains are susceptible to antibody binding, the RBD is the predominant target of neutralizing antibodies, followed by the NTD. S2-binding antibodies are poorly neutralizing, although some react broadly against many members of the sarbecovirus subgenus30,31. Such a pattern of antibody recognition is seen in naturally infected and vaccinated individuals98,99, indicating that the S glycoprotein expressed through vaccines resembles those on the infectious particles.
a, Spike protein of SARS-CoV-2. Top, schematic diagram of the domain organization. SD1, subdomain 1; SD2, subdomain 2; FP, fusion peptide; HR1, heptad repeat 1; HR2, heptad repeat 2; TM, transmembrane domain. S1/S2 and S2 are two protease cleavage sites. Left, closed state of the spike trimer with three down RBDs; right, open state of the spike trimer with two down RBDs and one up RBD. The spike is presented as a gray cartoon, with the RBD highlighted in cyan. The structures were published in ref. 97. b, RBD-directed neutralizing antibodies. For each antibody community (RBD-1 to RBD-7), the footprint of a representative antibody on the RBD is shown. The highly conserved N343 glycosylation site on the outer face is colored in deep blue. The RBM is outlined in light coral. See Table 1 for corresponding references. c, NTD-directed neutralizing antibodies. For each antibody community (NTD-1 to NTD-3), a representative complex structure of the spike trimer bound by the antibody is shown. The spike trimer and antibody are both presented as surface, with RBD colored in cyan, NTD in purple and S2 in gray.
S protein demonstrates a high degree of variability among different virus strains or circulating VOCs, particularly in the RBD and NTD domains, in part due to continuous pressure exerted by the human immune system. The most mutated VOC — Omicron, with its BA.1 and BA.2 subvariants — has approximately 35 mutations in the S protein compared with the prototype strain initially found in Wuhan, China. At least 15 of the 35 mutations are located in the RBD and 8 mutations in the NTD100,101, making Omicron BA.1 and BA.2 the most distinct in antigenic properties. Such antigenic variability affords this VOC a significantly increased chance of escaping from neutralization by antibody treatment and vaccine protection64,102,103,104.
RBD-directed neutralizing antibodies
The landscape of neutralizing epitopes on the spike trimer of SARS-CoV-2 has been mapped by a total of seven core ‘communities’ of antibodies (RBD-1 to RBD-7; Fig. 2b)105. These antibodies target three major surfaces on RBD, namely the top RBM face, the solvent-exposed outer face, and the cryptic inner face. The correspondence of this community-based classification and previous classification based on germline usage and structural information106,107 is provided in Table 1.
RBM-face-targeting antibodies are among the most potent neutralizing antibodies against SARS-CoV-2, exemplified by RBD-1, RBD-2 and RBD-3 (ref. 105). While overlapping extensively in their binding sites on the RBM surface, each community demonstrates a somewhat unique binding pose and specificity. RBD-1 binds to the center of the ACE2 binding site, whereas RBD-2 shifts to the ‘peak’ and RBD-3 toward the flat surface ‘mesa.’ Many antibodies to RBD-2 overlap with those previously categorized in class 1 (see Table 1 for definition), such as C102, C105, P2C-1F11, CB6 and REGN10933 (refs. 16,79,80,106,108). These antibodies preferentially use heavy chain germline variable (VH) segment IGHV3-53/IGHV3-66 and have limited somatic hypermutation and relatively short complementarity-determining region CDR3 loops (<15 residues). Two signature motifs, NY at VH residues 32 and 33 in the CDR1 and an SGGS motif at VH residues 53 to 56 in the CDR2, are crucial for RBM binding109,110,111. Furthermore, a substantial portion of RBD-2 antibodies, such as COV2-2196, S2E12 and A23-58.1, prefer to use IGHV1-58 and are therefore named IGHV1-58 supersite antibodies112,113. Such common features suggest that the IGHV3-53/IGHV3-66 and IGHV1-58-encoded antibodies possess unique biochemical and structural features that render them naturally strong in binding and highly complementary in shape to the RBM surface. However, such specific and strong binding is also associated with VOC escape. For example, RBD-2 and RBD-3 antibodies are severely affected by the p.K417N/T, p.E484K/A and p.N501Y mutations found in Alpha, Beta, Gamma and the Omicron subvariants BA.1 and BA.2 (refs. 102,114,115).
Outer-face-targeting antibodies are among the most broad and potent neutralizing antibodies against SARS-CoV-2 VOCs and are attributed to the RBD-4 and RBD-5 communities105. Their footprints on the RBD are solvent-exposed, accessible in both the up and down conformations, and largely overlap with those previously categorized in class 2 and class 3 (ref. 106; see Table 1). Members of the RBD-4 community bind toward the outer edge of the RBM and block ACE2, exemplified by antibodies C002, A19-46.1, BD-368-2, COV2-2130 and P2B-2F6 (refs. 79,106,116,117). Those in the RBD-5 community, however, do not block ACE2, as they bind away from the RBM and toward sites recognized by S309, REGN10987, P36-5D2, LY-CoV1404, C110 and C135 (refs. 47,106,108,118). RBD-4 antibodies, like those in class 2, appear to interact with residues F486 and Q493 in the RBM, which distinguish SARS-CoV-2 from SARS-CoV-1 and are thought to enhance the RBD of SARS-CoV-2 for binding to ACE2 (ref. 106). Interaction between RBD-4 antibodies and F486 mimics the interaction between that residue and ACE2: F486 buries into a hydrophobic pocket between the light and heavy chains of the antibodies. Another common interaction is with E484, mediated through either the heavy or the light chain. However, the p.E484K/A mutation has recently been found in Beta, Gamma, Omicron BA.1 and BA.2, Mu, Eta and Lota; this mutation markedly reduces, or even completely abrogates, the neutralizing activity of many antibodies in RBD-4 community. Interestingly, a combination of COV2-2196 (RBD-2) and COV2-2130 (RBD-4), when used in the therapeutic mode as Tixagevimab–Cilgavimab, manufactured by AstraZeneca, achieves good neutralization against Omicron BA.1 and BA.2, despite each of the two therapies individually having reduced or lost neutralizing activity119,120. The p.L452R mutation, primarily found in Delta, Epsilon and Kappa, also significantly reduces or completely abolishes neutralizing activity of RBD-4 antibodies121,122,123,124. However, the footprints of RBD-5 antibodies appear to center around the N343 glycan, highly conserved among SARS-CoV-2, SARS-CoV-1, and many bat and pangolin viruses that are considered high risks for potential outbreaks47. Representative antibodies REGN10987, LY-CoV1404 (the parental antibody of Bebtelovimab, manufactured by Eli Lilly), and C110 bind to regions between the outer edge of the RBM and N343 glycan106,108, whereas the other representative antibodies S309 (the parental antibody of Sotrovimab, manufactured by GlaxoSmithKline/Vir Biotechnology) and C135 bind to regions containing the N343 glycan. Escape mutations from REGN10987 include those at positions N439, N440 and G446 (refs. 102,125). Notably, LY-CoV1404 potently neutralizes Omicron BA.1 and BA.2 and has recently been approved by the US Food and Drug Administration (FDA) for emergency use126. Although S309 maintains its potency and breadth of neutralization against Omicron BA.1 and BA.2 in vitro, the FDA recently announced that the current 500 mg dose would not be effective against Omicron BA.2 infection. GlaxoSmithKline/Vir is preparing evidence in support of a higher dose for treating this subvariant. Lastly, like RBM face-targeting antibodies, the outer-face-targeting antibodies show low levels of somatic hypermutations without undergoing apparent maturation, indicating that they too exert timely and powerful antiviral functions during early infection. The relatively conserved nature of the outer surface could be explored more extensively for the development of antibody drugs and vaccines.
Inner-face-targeting antibodies belong to recently classified antibodies in the RBD-6 and RBD-7 communities. They are relatively smaller in number, weaker in neutralizing potency, and bind to cryptic epitopes opposite to the outer surface, accessible only when the RBD is in the up conformation. Some members require at least two or three RBDs in the up conformation for binding127,128,129. As the RBD can adopt a variety of conformations, such as tilting and turning when bound to various ligands compared with the ligand-free configuration, cryptic epitopes on the inner face can be transiently exposed and accessed by antibodies. Overall, the inner-face antibodies demonstrated stronger propensities to crosslink spike trimer than did the RBM antibodies, but their neutralizing potencies are generally weaker. This response is perhaps due to their transient nature and limited accessibility that adversely affects antibody recognition and penetration. Examples of such antibodies include S2X259, DH1047 and CR3022 (refs. 18,47,129). However, recently emerged Omicron subvariants BA.1 and BA.2 have resulted in marked reduction in and complete loss of neutralizing activity of RBD-6 and RBD-7 antibodies, largely due to mutations at positions S371, S373 and S375 (64,102).
Of note, there are some antibodies that do not exactly fall into the existing classification systems, such as ADG-2 and S2H97. While the epitope of ADG-2 partially overlaps with those in class 1 and class 4, ADG-2 approaches its epitope from a distinct angle130. S2H97 binds to a cryptic epitope at the cliff region right below the peak of RBM. S2H97 binding requires more opening of the RBD than does binding by ACE2 or RBD-6 and RBD-7 antibodies. Like the antibodies that do not compete with ACE2, S2H97 likely neutralizes the virus by interfering with and interrupting post-ACE2-binding steps before viral entry125.
NTD-directed neutralizing antibodies
These antibodies exhibit weaker neutralizing potency than that of antibodies to the RBD. They do not compete with ACE2 for binding to RBD, but may involve interference with conformational changes required for fusion or proposed interactions with attachment receptors, such as transmembrane lectins DC-SIGN, L-SIGN and SIGLEC1 (refs. 131,132). Some studies indicate their critical role in Fc-mediated effector functions, both in vitro and in vivo133. NTD neutralizing antibodies are categorized into three major communities (NTD-1 to NTD-3) on the basis of their binding pose and specificity, which are largely convergent to the ‘NTD supersite.’ The supersite is made of N1 (residues 14–26), N3 (residues 141–156), and N5 (residues 246–260) loops that are positively charged and surrounded by glycans105,131,134. The NTD-1 antibodies bind from the top side of NTD, covering the N terminus and residue Y144. 4A8, the first NTD-directed antibody identified, is the representative of this antibody community135. The NTD-2 antibodies bind to the front side, whereas the NTD-3 antibodies bind to the left side of the NTD, close to the RBD of the adjacent protomer105,131. However, all these antibodies seem to be sensitive to mutations occurring both inside and outside of their discrete footprint, suggesting that NTD-directed antibodies are largely conformation-sensitive136. Surprisingly, many mutations found in circulating VOCs and VOIs are insertions and deletions, such as 69–70del, Y144del, 157–158del and 242–244del, as opposed to the point mutations found in the RBD75,114,115,135. Interestingly, Omicron BA.2 has relatively fewer mutations than BA.1 in the NTD, providing a potential explanation for its reduced serological escape compared with that of BA.1. Nevertheless, these results may indicate that the deleted residues, or perhaps the supersite, are not absolutely required for viral infections, although the relative fitness of these mutants is currently unknown. As NTD-directed antibodies are prone to viral escape, it is not surprising that no antibodies directed to this domain are under clinical development. The reduction of serum neutralizing activity against VOCs and VOIs found in infected and vaccinated individuals must therefore be in part due to the deletions found in the NTD. Design of vaccine candidates capable of minimizing or completely overcoming the mutational effect in the NTD domain is highly desired.
Fc-dependent antibody functions and non-neutralizing antibodies
By engaging different Fc receptors expressed on different cell types, antibodies exert multiple effector functions upon antigen binding. For neutralizing antibodies, FcR-dependent effector functions can contribute to the potency of neutralization, particularly evident when neutralizing antibodies are used in a therapeutic mode137,138,139. When effector functions of non-neutralizing antibodies are considered, the outcome can be more complex and nuanced. These antibodies may contribute to protection by mediating antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP). However, they may contribute to disease exacerbation through antibody-dependent enhancement (ADE) of infection. ADE could occur when non-neutralizing or sub-neutralizing antibodies bind to and facilitate virus entry into Fc-receptor-expressing cells, or when such antibodies cause excessive inflammation and immune pathology. Elevated serum ADCC activities have been seen in individuals with COVID-19, particularly those who are hospitalized140,141. Kinetically, serum ADCC activities generally follow overall antibody titers, peaking at 2–4 weeks following infection and gradually declining thereafter142,143,144. Definitive evidence for ADE in human SARS-CoV-2 infection is relatively thin, although a very recent study reports Fc-receptor-mediated entry of antibody-opsonized SARS-CoV-2 into monocytes, leading to inflammatory cell death that may exacerbate the COVID-19 disease145. More studies and continuous monitoring of ADE are warranted, because in principle cross-reactive antibodies from previous coronavirus infection could exacerbate SARS-CoV-2 infection and, as new VOCs continue to emerge, neutralizing antibodies against earlier strains may lose neutralizing potency and become capable of mediating ADE instead146,147. This latter point is important from a vaccination perspective, because vaccines appear to induce more binding antibodies than neutralizing antibodies, compared with natural infection148.
Perspectives on SARS-CoV-2 vaccines
We have gained significant insights into the humoral immune response and antibody immunity following SARS-CoV-2 infection. Perhaps not surprisingly, the response to SARS-CoV-2 generally follows the same stereotypical pattern that is established in animal models and can be expected of acute viral infections. These insights help guide our design, implementation, and evaluation of prophylactic and therapeutic strategies.
Most current SARS-CoV-2 vaccines target the prototype SARS-CoV-2 strain identified during at the beginning of the pandemic149,150,151,152,153,154. Given the multiple waves of increased infection rates and breakthrough infections associated with escaping VOCs such as Alpha, Beta, Gamma, Delta and Omicron, broadly neutralizing vaccines are highly desirable. Interestingly, recent studies have identified potent, broadly neutralizing antibodies to the RBD that are capable of neutralizing all VOCs, including Omicron119,155,156, suggesting the likely existence of highly conserved and vulnerable regions within the RBD, a notion underscored in recent structural analyses of antibodies capable of neutralizing Omicron113. Broad and potent neutralizing antibodies can be substantially boosted after a third vaccine shot, particularly in individuals convalescing from COVID-19157,158, supporting a strategy to improve the neutralizing potency and breadth by a booster shot, potentially through heterologous vaccine modality. This notion is supported by an increasing number of clinical studies in which heterologous vaccine boosting has been found to be superior to homologous vaccine boosting159,160,161,162,163,164,165. Features of memory B cells that are activated by the boost, epitope specificities, and mechanisms of action of boosted antibodies are under investigation. Such results will inform on how to design and execute booster shots to maximize utility of the current vaccines.
Vaccines are also being developed to specifically target the S glycoprotein of emerging VOCs, similar to how flu vaccines are updated on an annual basis. Antigenically, the Omicron variant deviates the most from the prototype strain and is the most capable of escaping from vaccine protection64,102,103,104,120,166, providing an impetus for creating Omicron-targeted vaccine. However, preliminary studies of Omicron-specific messenger-RNA vaccines have not demonstrated superiority in inducing high-level Omicron-specific neutralizing antibodies over the prototype vaccine, raising concerns about this vaccine strategy167. An important point to consider when targeting strain-specific RBD is the fact that, while high-affinity antibodies are generally desired, antibodies with the highest neutralizing potency also tend to have limited breadth against the spectrum of variants. For example, antibodies in the RBD-1, RBD-2, RBD-3 and RBD-4 communities are very sensitive to the p.K417N, p.L452R and p.E484K mutations found in the Beta, Gamma, Delta and Omicron variants. By contrast, antibodies with relatively moderate potency, such as those in RBD-5, RBD-6 and RBD-7, are largely able to cross-neutralize many variants and even some animal coronaviruses in wild bats and pangolins105,127. Striking a balance between potency and breadth of antibodies elicited by vaccination is certainly an issue to address on the road toward broadly neutralizing and universal vaccines.
To develop a universal vaccine capable of inducing broad and potent neutralizing against all VOCs, multiple antigens from different VOCs could be combined in the same vaccine. For example, nanoparticle vaccines derived from distinct and mosaic RBDs from various coronavirus strains represent a viable strategy in this direction168,169,170,171. This strategy is further supported by a preclinical study in which a recombinant RBD trimer vaccine induced robust, long-lasting and protective immunity against SARS-CoV-2 challenge in small animals and rhesus macaques without obvious lung-tissue pathology170,172,173. Monoclonal antibodies isolated from mice immunized with the RBD trimer are able to cross-neutralize various antigenically distinct variants, suggesting that the trimer formulation is particular apt at inducing broad antibodies against major variants174. Lastly, individuals infected with and recovered from SARS-CoV-1 infection 17 years ago can generate broad and potent neutralizing antibodies against a wide variety of SARS-CoV-2 VOCs and five bat and pangolin sarbecoviruses after being vaccinated with an mRNA vaccine against SARS-CoV-2 (ref. 175). These results further highlight the possibility of a pan-coronavirus vaccine. Such broad protection implies the existence of long-lived memory B cells that recognize conserved features of these various related viruses. A deeper understanding of how such memory cells are induced, how they survive, and how they are recalled probably holds the key to designing broadly neutralizing vaccines that offer long-term protection.
References
Carvalho, T., Krammer, F. & Iwasaki, A. The first 12 months of COVID-19: a timeline of immunological insights. Nat. Rev. Immunol. 21, 245–256 (2021).
Tong, J. Y., Wong, A., Zhu, D., Fastenberg, J. H. & Tham, T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol. Head. Neck Surg. 163, 3–11 (2020).
da Rosa Mesquita, R. et al. Clinical manifestations of COVID-19 in the general population: systematic review. Wien. Klin. Wochenschr. 133, 377–382 (2021).
Wichmann, D. et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann. Intern. Med. 173, 268–277 (2020).
Jose, R. J. & Manuel, A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir. Med 8, e46–e47 (2020).
Lippi, G., Sanchis-Gomar, F. & Henry, B. M. COVID-19: unravelling the clinical progression of nature’s virtually perfect biological weapon. Ann. Transl. Med 8, 693 (2020).
Cevik, M., Kuppalli, K., Kindrachuk, J. & Peiris, M. Virology, transmission, and pathogenesis of SARS-CoV-2. Brit. Med. J. 371, m3862 (2020).
Mangalmurti, N. & Hunter, C. A. Cytokine storms: understanding COVID-19. Immunity 53, 19–25 (2020).
Elsner, R. A. & Shlomchik, M. J. Germinal center and extrafollicular B cell responses in vaccination, immunity, and autoimmunity. Immunity 53, 1136–1150 (2020).
Lam, J. H., Smith, F. L. & Baumgarth, N. B cell activation and response regulation during viral Infections. Viral Immunol. 33, 294–306 (2020).
Palm, A. E. & Henry, C. Remembrance of things past: long-term B cell memory after infection and vaccination. Front. Immunol. 10, 1787 (2019).
Long, Q. X. et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 26, 845–848 (2020).
Piccoli, L. et al. Mapping neutralizing and immunodominant sites on the SARS-CoV-2 spike receptor-binding domain by structure-guided high-resolution serology. Cell 183, 1024–1042 (2020).
Suthar, M. S. et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep. Med 1, 100040 (2020).
Premkumar, L. et al. The receptor binding domain of the viral spike protein is an immunodominant and highly specific target of antibodies in SARS-CoV-2 patients. Sci. Immunol. 5, eabc8413 (2020).
Robbiani, D. F. et al. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature 584, 437–442 (2020).
Chen, X. et al. Disease severity dictates SARS-CoV-2-specific neutralizing antibody responses in COVID-19. Signal Transduct. Target Ther. 5, 180 (2020).
Dan, J. M. et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science 371, eabf4063 (2021).
Hueso, T. et al. Convalescent plasma therapy for B-cell-depleted patients with protracted COVID-19. Blood 136, 2290–2295 (2020).
Klassen, S. A. et al. The effect of convalescent plasma therapy on mortality among patients with COVID-19: systematic review and meta-analysis. Mayo Clin. Proc. 96, 1262–1275 (2021).
Group, R. C. Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): a randomised controlled, open-label, platform trial. Lancet 397, 2049–2059 (2021).
Khoury, D. S. et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 27, 1205–1211 (2021).
Wajnberg, A. et al. Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science 370, 1227–1230 (2020).
Isho, B. et al. Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients. Sci. Immunol. 5, eabe5511 (2020).
Seow, J. et al. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat. Microbiol. 5, 1598–1607 (2020).
Wang, K. et al. Longitudinal dynamics of the neutralizing antibody response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Clin. Infect. Dis. 73, e531–e539 (2021).
Muecksch, F. et al. Longitudinal serological analysis and neutralizing antibody levels in coronavirus disease 2019 convalescent patients. J. Infect. Dis. 223, 389–398 (2021).
Chen, Y. et al. Quick COVID-19 healers sustain anti-SARS-CoV-2 antibody production. Cell 183, 1496–1507(2020).
Stamatatos, L. et al. mRNA vaccination boosts cross-variant neutralizing antibodies elicited by SARS-CoV-2 infection. Science 372, 1413–1418 (2021).
Wang, C. et al. A conserved immunogenic and vulnerable site on the coronavirus spike protein delineated by cross-reactive monoclonal antibodies. Nat. Commun. 12, 1715 (2021).
Pinto, D. et al. Broad betacoronavirus neutralization by a stem helix-specific human antibody. Science 373, 1109–1116 (2021).
Song, G. et al. Cross-reactive serum and memory B-cell responses to spike protein in SARS-CoV-2 and endemic coronavirus infection. Nat. Commun. 12, 2938 (2021).
Woodruff, M. C. et al. Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19. Nat. Immunol. 21, 1506–1516 (2020).
Sakharkar, M. et al. Prolonged evolution of the human B cell response to SARS-CoV-2 infection. Sci. Immunol. 6, eabg6916 (2021).
Kuri-Cervantes, L. et al. Comprehensive mapping of immune perturbations associated with severe COVID-19. Sci. Immunol. 5, eabd7114 (2020).
Long, Q. X. et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 26, 1200–1204 (2020).
Shenoy, S. SARS-CoV-2 (COVID-19), viral load and clinical outcomes; lessons learned one year into the pandemic: a systematic review. World J. Crit. Care Med. 10, 132–150 (2021).
Russell, M. W., Moldoveanu, Z., Ogra, P. L. & Mestecky, J. Mucosal immunity in COVID-19: a neglected but critical aspect of SARS-CoV-2 infection. Front. Immunol. 11, 611337 (2020).
Wang, Z. et al. Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci. Transl. Med. 13, eabf1555 (2021).
Cervia, C. et al. Systemic and mucosal antibody responses specific to SARS-CoV-2 during mild versus severe COVID-19. J. Allergy Clin. Immunol. 147, 545–557 e549 (2021).
Sterlin, D. et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci. Transl. Med. 13, eabd2223 (2021).
Froberg, J. et al. SARS-CoV-2 mucosal antibody development and persistence and their relation to viral load and COVID-19 symptoms. Nat. Commun. 12, 5621 (2021).
Hu, B., Guo, H., Zhou, P. & Shi, Z. L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 19, 141–154 (2021).
Lu, R. et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395, 565–574 (2020).
Dugan, H. L. et al. Profiling B cell immunodominance after SARS-CoV-2 infection reveals antibody evolution to non-neutralizing viral targets. Immunity 54, 1290–1303(2021).
Che, X. Y. et al. Antigenic cross-reactivity between severe acute respiratory syndrome-associated coronavirus and human coronaviruses 229E and OC43. J. Infect. Dis. 191, 2033–2037 (2005).
Pinto, D. et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature 583, 290–295 (2020).
Tian, X. et al. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg. Microbes Infect. 9, 382–385 (2020).
Zhu, Y. et al. Cross-reactive neutralization of SARS-CoV-2 by serum antibodies from recovered SARS patients and immunized animals. Sci. Adv. 6, eabc9999 (2020).
Shrock, E. et al. Viral epitope profiling of COVID-19 patients reveals cross-reactivity and correlates of severity. Science 370, eabd4250 (2020).
Ng, K. W. et al. Preexisting and de novo humoral immunity to SARS-CoV-2 in humans. Science 370, 1339–1343 (2020).
Anderson, E. M. et al. Seasonal human coronavirus antibodies are boosted upon SARS-CoV-2 infection but not associated with protection. Cell 184, 1858–1864 e1810 (2021).
Majdoubi, A. et al. A majority of uninfected adults show preexisting antibody reactivity against SARS-CoV-2. JCI Insight 6, e146316 (2021).
Tso, F. Y. et al. High prevalence of pre-existing serological cross-reactivity against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in sub-Saharan Africa. Int J. Infect. Dis. 102, 577–583 (2021).
Ortega, N. et al. Seven-month kinetics of SARS-CoV-2 antibodies and role of pre-existing antibodies to human coronaviruses. Nat. Commun. 12, 4740 (2021).
Guo, L. et al. Cross-reactive antibody against human coronavirus OC43 spike protein correlates with disease severity in COVID-19 patients: a retrospective study. Emerg. Microbes Infect. 10, 664–676 (2021).
Grifoni, A. et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell 181, 1489–1501 e1415 (2020).
Mateus, J. et al. Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science 370, 89–94 (2020).
Sette, A. & Crotty, S. Pre-existing immunity to SARS-CoV-2: the knowns and unknowns. Nat. Rev. Immunol. 20, 457–458 (2020).
Hansen, K. E., Arnason, J. & Bridges, A. J. Autoantibodies and common viral illnesses. Semin. Arthritis Rheum. 27, 263–271 (1998).
Rivera-Correa, J. & Rodriguez, A. Divergent roles of antiself antibodies during infection. Trends Immunol. 39, 515–522 (2018).
Wang, E. Y. et al. Diverse functional autoantibodies in patients with COVID-19. Nature 595, 283–288 (2021).
Bastard, P. et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 370, eabd4584 (2020).
Bastard, P. et al. Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths. Sci. Immunol. 6, eabl4340 (2021).
Hadjadj, J. et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 369, 718–724 (2020).
Blanco-Melo, D. et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell 181, 1036–1045 (2020).
Galani, I. E. et al. Untuned antiviral immunity in COVID-19 revealed by temporal type I/III interferon patterns and flu comparison. Nat. Immunol. 22, 32–40 (2021).
Bonometti, R. et al. The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection. Eur. Rev. Med. Pharm. Sci. 24, 9695–9697 (2020).
Gigli, G. L. et al. HLA and immunological features of SARS-CoV-2-induced Guillain–Barre syndrome. Neurol. Sci. 41, 3391–3394 (2020).
Finsterer, J., Scorza, F. A. & Fiorini, A. C. SARS-CoV-2-associated Guillain–Barre syndrome in 62 patients. Eur. J. Neurol. 28, e10–e12 (2021).
Patil, N. R., Herc, E. S. & Girgis, M. Cold agglutinin disease and autoimmune hemolytic anemia with pulmonary embolism as a presentation of COVID-19 infection. Hematol. Oncol. Stem Cell Ther. 20, 30113–30116 (2020).
Jensen, C. E., Wilson, S., Thombare, A., Weiss, S. & Ma, A. Cold agglutinin syndrome as a complication of Covid-19 in two cases. Clin. Infect. Pr. 7, 100041 (2020).
Liu, Y., Sawalha, A. H. & Lu, Q. COVID-19 and autoimmune diseases. Curr. Opin. Rheumatol. 33, 155–162 (2021).
Kaneko, N. et al. Loss of Bcl-6-expressing T follicular helper cells and germinal centers in COVID-19. Cell 183, 143–157 (2020).
Duan, Y. Q. et al. Deficiency of TFH cells and germinal center in deceased COVID-19 patients. Curr. Med. Sci. 40, 618–624 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506 (2020).
Giamarellos-Bourboulis, E. J. et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe 27, 992–1000 (2020).
Chen, G. et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Invest. 130, 2620–2629 (2020).
Ju, B. et al. Human neutralizing antibodies elicited by SARS-CoV-2 infection. Nature 584, 115–119 (2020). This study shows that potent neutralizing antibodies against SARS-CoV-2 can be elicited in convalescent individuals and that the major mode of action is through competition with the receptor ACE2 for RBD binding.
Shi, R. et al. A human neutralizing antibody targets the receptor-binding site of SARS-CoV-2. Nature 584, 120–124 (2020).
Brouwer, P. J. M. et al. Potent neutralizing antibodies from COVID-19 patients define multiple targets of vulnerability. Science 369, 643–650 (2020).
Gaebler, C. et al. Evolution of antibody immunity to SARS-CoV-2. Nature 591, 639–644 (2021).
Sokal, A. et al. Maturation and persistence of the anti-SARS-CoV-2 memory B cell response. Cell 184, 1201–1213(2021).
Muecksch, F. et al. Affinity maturation of SARS-CoV-2 neutralizing antibodies confers potency, breadth, and resilience to viral escape mutations. Immunity 54, 1853–1868(2021).
Wang, Z. et al. Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature 595, 426–431 (2021).
Moriyama, S. et al. Temporal maturation of neutralizing antibodies in COVID-19 convalescent individuals improves potency and breadth to circulating SARS-CoV-2 variants. Immunity 54, 1841–1852 e1844 (2021).
Turner, J. S. et al. SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Nature 595, 421–425 (2021). Analyses of bone marrow aspirates from convalescent individuals show persistence of SARS-CoV-2-specific plasma cells.
Mathew, D. et al. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science 369, eabc8511 (2020).
Sekine, T. et al. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. Cell 183, 158–168 e114 (2020).
Chen, Z. & John Wherry, E. T cell responses in patients with COVID-19. Nat. Rev. Immunol. 20, 529–536 (2020).
Chandrashekar, A. et al. SARS-CoV-2 infection protects against rechallenge in rhesus macaques. Science 369, 812–817 (2020).
Munster, V. J. et al. Respiratory disease in rhesus macaques inoculated with SARS-CoV-2. Nature 585, 268–272 (2020).
Poon, M. M. L. et al. SARS-CoV-2 infection generates tissue-localized immunological memory in humans. Sci. Immunol. 6, eabl9105 (2021). A rare analysis of seropositive organ donors that reveals persistence of virus-specific GCs in lung-associated lymph nodes 6 months after infection.
Yao, H. et al. Molecular architecture of the SARS-CoV-2 virus. Cell 183, 730–738 e713 (2020). By cryo-electron tomography (cryo-ET) and subtomogram averaging (STA), this study structurally resolves the S protein in pre- and post- fusion conformations and characterizes the molecular architecture of the SARS-CoV-2 virion at a high resolution.
Ge, J. et al. Antibody neutralization of SARS-CoV-2 through ACE2 receptor mimicry. Nat. Commun. 12, 250 (2021). This study shows that IGHV3-53 antibodies neutralize by competing with ACE2 for RBD binding through receptor mimicry and inducing rapid and premature shedding of S1 from the spike trimer.
Wrapp, D. et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367, 1260–1263 (2020). Together with ref. 97, this study reports the cyro-EM structure of 2019-nCoV S trimer in the prefusion conformation, revealing its predominant state of having one of the three RBDs in a conformation accessible to ACE2.
Walls, A. C. et al. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 181, 281–292 e286 (2020).
Wang, Z. et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. Nature 592, 616–622 (2021). This study shows that antibodies induced by Moderna (mRNA-1273) and Pfizer–BioNTech (BNT162b2) mRNA vaccines substantially or completely lost neutralizing activities against SARS-CoV-2 variants carrying single or combined substitutions of K417N, E484K and N501Y.
Turner, J. S. et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 596, 109–113 (2021).
Viana, R. et al. Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa. Nature 603, 679–686 (2022).
McCallum, M. et al. Structural basis of SARS-CoV-2 Omicron immune evasion and receptor engagement. Science 375, eabn8652 (2022). A structural study of the Omicron spike trimer and its RBD bound by the broadly neutralizing antibody S309 (the parent antibody of Sotrovimab) or the human ACE2, explaining how Omicron partially or completely escapes many neutralizing antibodies.
Liu, L. et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature 602, 676–681 (2022). Together with refs. 102,103, this study shows the Omicron variant partially or fully escapes most neutralizing antibodies identified thus far.
Cele, S. et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature 602, 654–656 (2022).
Cao, Y. et al. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature 602, 657–663 (2022).
Hastie, K. M. et al. Defining variant-resistant epitopes targeted by SARS-CoV-2 antibodies: a global consortium study. Science 374, 472–478 (2021). A comprehensive analysis of 269 RBD-binding monoclonal antibodies that classifies these antibodies into 7communities with distinct footprints and competition profiles.
Barnes, C. O. et al. SARS-CoV-2 neutralizing antibody structures inform therapeutic strategies. Nature 588, 682–687 (2020). This study classifies RBD-binding monoclonal antibodies into four major classes based on distinct structural features.
Yuan, M., Liu, H., Wu, N. C. & Wilson, I. A. Recognition of the SARS-CoV-2 receptor binding domain by neutralizing antibodies. Biochem. Biophys. Res. Commun. 538, 192–203 (2021). This study classifies RBD-binding monoclonal antibodies into RBS-A, RBS-B and RBS-C based on distinct structural and germline features.
Hansen, J. et al. Studies in humanized mice and convalescent humans yield a SARS-CoV-2 antibody cocktail. Science 369, 1010–1014 (2020).
Zhang, Q. et al. Potent and protective IGHV3-53/3-66 public antibodies and their shared escape mutant on the spike of SARS-CoV-2. Nat. Commun. 12, 4210 (2021).
Barnes, C. O. et al. Structures of human antibodies bound to SARS-CoV-2 spike reveal common epitopes and recurrent features of antibodies. Cell 182, 828–842.e816 (2020).
Yuan, M. et al. Structural basis of a shared antibody response to SARS-CoV-2. Science 369, 1119–1123 (2020). A comprehensive study of 294 anti-SARS-CoV-2 antibodies that reveals preferential usage of IGHV3-53 in RBD-targeting antibodies.
Jones, B. E. et al. The neutralizing antibody, LY-CoV555, protects against SARS-CoV-2 infection in nonhuman primates. Sci. Transl. Med. 13, eabf1906 (2021).
Zhou, T. et al. Structural basis for potent antibody neutralization of SARS-CoV-2 variants including B.1.1.529. Science 376, eabn8897 (2022). A comprehensive cyro-EM structural study of Omicron S protein trimer and various RBD-binding that delineates potential mechanims of broadly neutralizing antibodies and mechansims to escape.
Wang, R. et al. Analysis of SARS-CoV-2 variant mutations reveals neutralization escape mechanisms and the ability to use ACE2 receptors from additional species. Immunity 54, 1611–1621(2021).
Wang, P. et al. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature 593, 130–135 (2021).
Cao, Y. et al. Potent neutralizing antibodies against SARS-CoV-2 identified by high-throughput single-cell sequencing of convalescent patients’ B cells. Cell 182, 73–8 (2020).
Wang, L. et al. Ultrapotent antibodies against diverse and highly transmissible SARS-CoV-2 variants. Science 373, eabh1766 (2021).
Shan, S. et al. A potent and protective human neutralizing antibody against SARS-CoV-2variants. Front. Immunol. 12, 766821 (2021).
VanBlargan, L. A. et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat. Med. 28, 490–495 (2022).
Dejnirattisai, W. et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell 185, 467–484(2022).
Planas, D. et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature 596, 276–280 (2021).
Zhang, J. et al. Membrane fusion and immune evasion by the spike protein of SARS-CoV-2 Delta variant. Science 374, 1353–1360 (2021).
Garcia-Beltran, W. F. et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell 184, 2372–2383(2021).
McCallum, M. et al. SARS-CoV-2 immune evasion by the B.1.427/B.1.429 variant of concern. Science 373, 648–654 (2021).
Starr, T. N. et al. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science 371, 850–854 (2021). An efficient high-throughput yeast library system is used to reveal potential mutations of the SARS-CoV-2 RBD that would escape three therapeutic antibodies, LY-CoV016, REGN10933 and REGN10987.
Westendorf, K. et al. LY-CoV1404 (bebtelovimab) potently neutralizes SARS-CoV-2 variants. Cell Rep. 39, 110812 (2022).
He, W. T. et al. Targeted isolation of diverse human protective broadly neutralizing antibodies against SARS-like viruses. Nat. Immunol. 23, 960–970 (2022).
Yuan, M. et al. A highly conserved cryptic epitope in the receptor binding domains of SARS-CoV-2 and SARS-CoV. Science 368, 630–633 (2020).
Tortorici, M. A. et al. Broad sarbecovirus neutralization by a human monoclonal antibody. Nature 597, 103–108 (2021).
Rappazzo, C. G. et al. Broad and potent activity against SARS-like viruses by an engineered human monoclonal antibody. Science 371, 823–829 (2021).
McCallum, M. et al. N-terminal domain antigenic mapping reveals a site of vulnerability for SARS-CoV-2. Cell 184, 2332–2347(2021).
Lempp, F. A. et al. Lectins enhance SARS-CoV-2 infection and influence neutralizing antibodies. Nature 598, 342–347 (2021).
Suryadevara, N. et al. Neutralizing and protective human monoclonal antibodies recognizing the N-terminal domain of the SARS-CoV-2 spike protein. Cell 184, 2316–2331.e2315 (2021).
Cerutti, G. et al. Potent SARS-CoV-2 neutralizing antibodies directed against spike N-terminal domain target a single supersite. Cell Host Microbe 29, 819–833.e817 (2021).
Chi, X. et al. A neutralizing human antibody binds to the N-terminal domain of the spike protein of SARS-CoV-2. Science 369, 650–655 (2020).
Graham, C. et al. Neutralization potency of monoclonal antibodies recognizing dominant and subdominant epitopes on SARS-CoV-2 spike is impacted by the B.1.1.7 variant. Immunity 54, 1276–1289(2021).
Winkler, E. S. et al. Human neutralizing antibodies against SARS-CoV-2 require intact Fc effector functions for optimal therapeutic protection. Cell 184, 1804–1820 (2021). This study shows that neutralizing antibodies require Fc to achieve maximal clinical and virological benefits in a manner that also depends on monocytes and CD8 T cells.
Yamin, R. et al. Fc-engineered antibody therapeutics with improved anti-SARS-CoV-2 efficacy. Nature 599, 465–470 (2021).
Schafer, A. et al. Antibody potency, effector function, and combinations in protection and therapy for SARS-CoV-2 infection in vivo. J. Exp. Med. 218, e20201993 (2021).
Dufloo, J. et al. Asymptomatic and symptomatic SARS-CoV-2 infections elicit polyfunctional antibodies. Cell Rep. Med 2, 100275 (2021).
Chen, X. et al. The development and kinetics of functional antibody-dependent cell-mediated cytotoxicity (ADCC) to SARS-CoV-2 spike protein. Virology 559, 1–9 (2021).
Lee, W. S. et al. Decay of Fc-dependent antibody functions after mild to moderate COVID-19. Cell Rep. Med. 2, 100296 (2021).
Anand, S. P. et al. Longitudinal analysis of humoral immunity against SARS-CoV-2 spike in convalescent individuals up to 8 months post-symptom onset. Cell Rep. Med. 2, 100290 (2021).
Yu, Y. et al. Antibody-dependent cellular cytotoxicity response to SARS-CoV-2 in COVID-19 patients. Signal Transduct. Target Ther. 6, 346 (2021).
Junqueira, C. et al. FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation. Nature 606, 576–584 (2022).
Iwasaki, A. & Yang, Y. The potential danger of suboptimal antibody responses in COVID-19. Nat. Rev. Immunol. 20, 339–341 (2020).
Lee, W. S., Wheatley, A. K., Kent, S. J. & DeKosky, B. J. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat. Microbiol. 5, 1185–1191 (2020).
Amanat, F. et al. SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD, and S2. Cell 184, 3936–3948(2021).
Dai, L. & Gao, G. F. Viral targets for vaccines against COVID-19. Nat. Rev. Immunol. 21, 73–82 (2021).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 384, 403–416 (2021).
Bos, R. et al. Ad26 vector-based COVID-19 vaccine encoding a prefusion-stabilized SARS-CoV-2 spike immunogen induces potent humoral and cellular immune responses. NPJ Vaccines 5, 91 (2020).
Heath, P. T. et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N. Engl. J. Med. 385, 1172–1183 (2021).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Zhu, F. C. et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 396, 479–488 (2020).
Yin, W. et al. Structures of the Omicron spike trimer with ACE2 and an anti-Omicron antibody. Science 375, 1048–1053 (2022).
Wang, K. et al. Memory B cell repertoire from triple vaccinees against diverse SARS-CoV-2 variants. Nature 603, 919–925 (2022).
Muecksch, F. et al. Increased memory B cell potency and breadth after a SARS-CoV-2 mRNA boost. Nature, https://doi.org/10.1038/s41586-022-04778-y (2022).
Pajon, R. et al. SARS-CoV-2 Omicron variant neutralization after mRNA-1273 booster vaccination. N. Engl. J. Med. 386, 1088–1091 (2022).
Munro, A. P. S. et al. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. Lancet 398, 2258–2276 (2021).
Liu, X. et al. Safety and immunogenicity of heterologous versus homologous prime-boost schedules with an adenoviral vectored and mRNA COVID-19 vaccine (Com-COV): a single-blind, randomised, non-inferiority trial. Lancet 398, 856–869 (2021).
Yorsaeng, R. et al. Immunogenicity of a third dose viral-vectored COVID-19 vaccine after receiving two-dose inactivated vaccines in healthy adults. Vaccine 40, 524–530 (2022).
Ai, J. et al. Recombinant protein subunit vaccine booster following two-dose inactivated vaccines dramatically enhanced anti-RBD responses and neutralizing titers against SARS-CoV-2 and variants of concern. Cell Res. 32, 103–106 (2022).
Zhu, F. et al. Safety and immunogenicity of a recombinant adenovirus type-5-vectored COVID-19 vaccine with a homologous prime-boost regimen in healthy participants aged 6 years and above: a randomised, double-blind, placebo-controlled, phase 2b trial. Clin. Infect. https://doi.org/10.1093/cid/ciab845 (2021).
Li, J. et al. Heterologous AD5-nCOV plus CoronaVac versus homologous CoronaVac vaccination: a randomized phase 4 trial. Nat. Med. 28, 401–409 (2022).
Atmar, R. L. et al. Homologous and heterologous Covid-19 booster vaccinations. N. Engl. J. Med. 386, 1046–1057 (2022).
Carreno, J. M. et al. Activity of convalescent and vaccine serum against SARS-CoV-2 Omicron. Nature 602, 682–688 (2022).
Gagne, M. et al. mRNA-1273 or mRNA-Omicron boost in vaccinated macaques elicits similar B cell expansion, neutralizing responses, and protection from Omicron. Cell 185, 1556–1571.e1518 (2022).
Saunders, K. O. et al. Neutralizing antibody vaccine for pandemic and pre-emergent coronaviruses. Nature 594, 553–559 (2021). This study shows nanoparticle vaccines that express the SARS-CoV-2 RBD could induce a cross-neutralizing antibody response in macaques against bat coronaviruses, SARS-CoV-1 and SARS-CoV-2.
Joyce, M. G. et al. SARS-CoV-2 ferritin nanoparticle vaccines elicit broad SARS coronavirus immunogenicity. Cell Rep. 37, 110143 (2021).
Cohen, A. A. et al. Mosaic nanoparticles elicit cross-reactive immune responses to zoonotic coronaviruses in mice. Science 371, 735–741 (2021).
Walls, A. C. et al. Elicitation of broadly protective sarbecovirus immunity by receptor-binding domain nanoparticle vaccines. Cell 184, 5432–5447 (2021). By showing that mosaic and cocktail nanoparticles displaying multiple sarbecovirus RBDs can elicit broadly neutralizing antibodies and confer protection, this study offers a promising sign for such vaccines to be further tested in clinical studies.
Wuertz, K. M. et al. A SARS-CoV-2 spike ferritin nanoparticle vaccine protects hamsters against Alpha and Beta virus variant challenge. NPJ Vaccines 6, 129 (2021).
Li, D. et al. Breadth of SARS-CoV-2 neutralization and protection induced by a nanoparticle vaccine. Preprint at bioRxiv https://doi.org/10.1101/2022.01.26.477915 (2022).
Qu, L. et al. Circular RNA vaccines against SARS-CoV-2 and emerging variants. Cell 185, 1728–1744.e1716 (2022).
Tan, C. W. et al. Pan-sarbecovirus neutralizing antibodies in BNT162b2-immunized SARS-CoV-1 survivors. N. Engl. J. Med. 385, 1401–1406 (2021).
Hurlburt, N. K. et al. Structural basis for potent neutralization of SARS-CoV-2 and role of antibody affinity maturation. Nat. Commun. 11, 5413 (2020).
Wu, Y. et al. A noncompeting pair of human neutralizing antibodies block COVID-19 virus binding to its receptor ACE2. Science 368, 1274–1278 (2020).
Zost, S. J. et al. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature 584, 443–449 (2020).
Tortorici, M. A. et al. Ultrapotent human antibodies protect against SARS-CoV-2 challenge via multiple mechanisms. Science 370, 950–957 (2020).
Wu, N. C. et al. An alternative binding mode of IGHV3-53 antibodies to the SARS-CoV-2 receptor binding domain. Cell Rep. 33, 108274 (2020).
Kreye, J. et al. A therapeutic non-self-reactive SARS-CoV-2 antibody protects from lung pathology in a COVID-19 hamster model. Cell 183, 1058–1069(2020).
Kim, C. et al. A therapeutic neutralizing antibody targeting receptor binding domain of SARS-CoV-2 spike protein. Nat. Commun. 12, 288 (2021).
Liu, L. et al. Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature 584, 450–456 (2020).
Du, S. et al. Structurally resolved SARS-CoV-2 antibody shows high efficacy in severely infected hamsters and provides a potent cocktail pairing strategy. Cell 183, 1013–1023 (2020).
VanBlargan, L. A. et al. A potently neutralizing SARS-CoV-2 antibody inhibits variants of concern by utilizing unique binding residues in a highly conserved epitope. Immunity 54, 2399–2416(2021).
Wec, A. Z. et al. Broad neutralization of SARS-related viruses by human monoclonal antibodies. Science 369, 731–736 (2020).
Liu, H. et al. Cross-neutralization of a SARS-CoV-2 antibody to a functionally conserved site is mediated by avidity. Immunity 53, 1272–1280 (2020).
Li, D. et al. In vitro and in vivo functions of SARS-CoV-2 infection-enhancing and neutralizing antibodies. Cell 184, 4203–4219 (2021).
Huo, J. et al. Neutralization of SARS-CoV-2 by destruction of the prefusion spike. Cell Host Microbe 28, 445–454 (2020).
Zhou, D. et al. Structural basis for the neutralization of SARS-CoV-2 by an antibody from a convalescent patient. Nat. Struct. Mol. Biol. 27, 950–958 (2020).
Lv, Z. et al. Structural basis for neutralization of SARS-CoV-2 and SARS-CoV by a potent therapeutic antibody. Science 369, 1505–1509 (2020).
Acknowledgements
The authors thank S. Shan for help with preparation of Table 1. Work of H.Q. is funded in part by National Natural Science Foundation of China (grant 81621002, 31830023), the Tsinghua-Peking Center for Life Sciences, the Beijing Municipal Science & Technology Commission, and the Beijing Frontier Research Center for Biological Structure. H.Q. is an HHMI-Gates International Research Scholar. L.Z. is funded by the National Key Plan for Scientific Research and Development of China (2020YFC0848800, 2020YFC08499, 2021YFC0864500, 2020YFC0861200), the National Natural Science Foundation (9216920007), Beijing Municipal Science and Technology Commission (Z201100005420019), Tsinghua University Scientific Research Program (20201080053 and 2020Z99CFG004), and Tencent Foundation, Shuidi Foundation, and TH Capital. The findings and conclusions within are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation or the Howard Hughes Medical Institute.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
L.Z. has filed patent applications for BRII-196 and BRII-198 antibodies against SARS-CoV-2 and is a share holder of Tsb Therapeutics.
Peer review
Peer review information
Nature Immunology thanks the anonymous reviewers for their contribution to the peer review of this work. Editor recognition statement: L. A. Dempsey was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qi, H., Liu, B., Wang, X. et al. The humoral response and antibodies against SARS-CoV-2 infection. Nat Immunol 23, 1008–1020 (2022). https://doi.org/10.1038/s41590-022-01248-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41590-022-01248-5
This article is cited by
-
Redefining serological diagnostics with immunoaffinity proteomics
Clinical Proteomics (2023)
-
Humoral immunity for durable control of SARS-CoV-2 and its variants
Inflammation and Regeneration (2023)
-
Broadly neutralizing antibodies to SARS-CoV-2 and other human coronaviruses
Nature Reviews Immunology (2023)
-
sciCSR infers B cell state transition and predicts class-switch recombination dynamics using single-cell transcriptomic data
Nature Methods (2023)
-
Human memory B cells show plasticity and adopt multiple fates upon recall response to SARS-CoV-2
Nature Immunology (2023)