Abstract
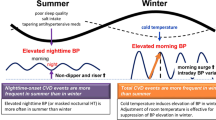
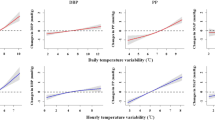
Environmental temperature is now well known to have a U-shaped relationship with cardiovascular (CV) and all-cause mortality. Both heat and cold above and below an optimum temperature, respectively, are associated with adverse outcomes. However, cold in general and moderate cold specifically is predominantly responsible for much of temperature-attributable adversity. Importantly, hypertension—the most important CV risk factor—has seasonal variation such that BP is significantly higher in winter. Besides worsening BP control in established hypertensives, cold-induced BP increase also contributes to long-term BP variability among normotensive and pre-hypertensive patients, also a known CV risk factor. Disappointingly, despite the now well-stablished impact of temperature on BP and on CV mortality separately, direct linkage between seasonal BP change and CV outcomes remains preliminary. Proving or disproving this link is of immense clinical and public health importance because if seasonal BP variation contributes to seasonal adversity, this should be a modifiable risk. Mechanistically, existing evidence strongly suggests a central role of the sympathetic nervous system (SNS), and secondarily, the renin–angiotensin–aldosterone axis (RAAS) in mediating cold-induced BP increase. Though numerous other inflammatory, metabolic, and vascular perturbations likely also contribute, these may also well be secondary to cold-induced SNS/RAAS activation. This review aims to summarize the current evidence linking temperature, BP and CV outcomes. We also examine underlying mechanisms especially in regard to the SNS/RAAS axis, and highlight possible mitigation measures for clinicians.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data used to prepare this review are available upon request from the authors
References
Climate in Earth History. Washington, DC: National Academies Press; 1982. http://www.nap.edu/catalog/11798.
GISTEMP team 2021. GISS Surface Temperature Analysis (GISTEMP), version 4. NASA Goddard Institute for Space Studies. 2021. https://data.giss.nasa.gov/gistemp/Dataset accessed 3 July 2021.
Herring D. Climate change: global temperature projections. 2012. https://www.climate.gov/news-features/understanding-climate/climate-change-global-temperature-projections.
Burkett VR, Suarez AG, Bindi M, Conde C, Mukerji R, Prather MJ, et al. Point of departure. In: Climate change 2014: impacts, adaptation, and vulnerability. Part A: global and sectoral aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2014. p. 169–194.
Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom: Cambridge University Press and New York, NY, USA: IPCC; 2014.p. 1132.
World Health Organization (WHO). Climate change and health. WHO Fact Sheet. 2018. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health.
Zafeiratou S, Samoli E, Dimakopoulou K, Rodopoulou S, Analitis A, Gasparrini A, et al. A systematic review on the association between total and cardiopulmonary mortality/morbidity or cardiovascular risk factors with long-term exposure to increased or decreased ambient temperature. Sci Total Environ. 2021;772:145383.
Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology 2014;25:781–9.
Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 2016;6:258–68.
Armstrong B, Bell ML, Coelho M de SZS, Guo YLL, Guo Y, et al. Longer-term impact of high and low temperature on mortality: An international study to clarify length of mortality displacement. Environ Health Perspect. 2017;125:107009.
Cao R, Wang Y, Huang J, He J, Ponsawansong P, Jin J, et al. The mortality effect of apparent temperature: a multi-city study in asia. Int J Environ Res Public Health. 2021;18:4675.
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–75. https://linkinghub.elsevier.com/retrieve/pii/S0140673614621140.
Martínez-Solanas È, Quijal-Zamorano M, Achebak H, Petrova D, Robine JM, Herrmann FR, et al. Projections of temperature-attributable mortality in Europe: a time series analysis of 147 contiguous regions in 16 countries. Lancet Planet Health. 2021;5:e446–54.
Zhang Y, Wang S, Zhang X, Hu Q, Zheng CJ. Association between moderately cold temperature and mortality in China. Environ Sci Pollut Res. 2020;27:26211–20.
Burkart KG, Brauer M, Aravkin AY, Godwin WW, Hay SI, He J, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398:685–97. www.thelancet.com.
Chen R, Yin P, Wang L, Liu C, Niu Y, Wang W, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ. 2018;363:k4306. https://www.bmj.com/lookup/doi/10.1136/bmj.k4306.
van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG. Seasonal variation in cause-specific mortality: Are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol. 2001;30:1109–16.
Zhang Y, Li S, Pan X, Tong S, Jaakkola JJK, Gasparrini A, et al. The effects of ambient temperature on cerebrovascular mortality: An epidemiologic study in four climatic zones in China. Environ Health Glob Access Sci Source. 2014;13:24.
Singh N, Mhawish A, Ghosh S, Banerjee T, Mall RK. Attributing mortality from temperature extremes: a time series analysis in Varanasi, India. Sci Total Environ. 2019;665:453–64.
Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–13.
Baccini M, Kosatsky T, Analitis A, Anderson HR, D’Ovidio M, Menne B, et al. Impact of heat on mortality in 15 European cities: Attributable deaths under different weather scenarios. J Epidemiol Community Health. 2011;65:64–70.
Fu SH, Gasparrini A, Rodriguez PS, Jha P Mortality attributable to hot and cold ambient temperatures in India: a nationally representative case-crossover study. PLoS Med. 2018;15:e1002619.
Chen Q, Wang J, Tian J, Tang X, Yu C, Marshall RJ, et al. Association between ambient temperature and blood pressure and blood pressure regulators: 1831 hypertensive patients followed up for three years. PLoS ONE. 2013;8:e84522. https://doi.org/10.1371/journal.pone.0084522.
Carder M, McNamee R, Beverland I, Elton R, Cohen GR, Boyd J, et al. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup Environ Med. 2005;62:702–10.
Scovronick N, Sera F, Acquaotta F, Garzena D, Fratianni S, Wright CY, et al. The association between ambient temperature and mortality in South Africa: a time-series analysis. Environ Res. 2018;161:229–35.
Ballester J, Robine JM, Herrmann FR, Rodó X. Long-term projections and acclimatization scenarios of temperature-related mortality in Europe. Nat Commun. 2011;2:358.
Gasparrini A, Guo Y, Sera F, Vicedo-Cabrera AM, Huber V, Tong S, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1:e360–7.
Vicedo-Cabrera AM, Guo Y, Sera F, Huber V, Schleussner CF, Mitchell D, et al. Temperature-related mortality impacts under and beyond Paris Agreement climate change scenarios. Clim Change. 2018;150:391–402.
Vardoulakis S, Dear K, Hajat S, Heaviside C, Eggen B, McMichael AJ. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ Health Perspect. 2015;122:1285–92.
World Health Organization (WHO). Global health estimates 2020: deaths by cause, age, sex, by country and by region, 2000–2019. 2020. www.who.int/data/gho/data/themes/mortality.
MASTER AM, Dack S, Jaffe HL. Factors and events associated with onset of coronary artery thrombosis. J Am Med Assoc. 1937;109:546–9. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.1937.02780340002002.
Braga ALF, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110:859–63. http://ehpnet1.niehs.nih.gov/docs/2002/110p859-863braga/abstract.html.
Chu ML, Shih CY, Hsieh TC, Chen HL, Lee CW, Hsieh JC. Acute myocardial infarction hospitalizations between cold and hot seasons in an island across tropical and subtropical climate zones—a population-based study. Int J Environ Res Public Health. 2019;16:2769.
Eng H, Mercer JB. Seasonal variations in mortality caused by cardiovascular diseases in Norway and Ireland. J Cardiovasc Risk. 1998;5:89–95.
Loughnan ME, Nicholls N, Tapper NJ. Demographic, seasonal, and spatial differences in acute myocardial infarction admissions to hospital in Melbourne Australia. Int J Health Geogr. 2007;7. https://doi.org/10.1186/1476-072X-7-42.
Madaniyazi L, Chung Y, Kim Y, Tobias A, Ng CFS, Seposo X, et al. Seasonality of mortality under a changing climate: a time-series analysis of mortality in Japan between 1972 and 2015. Environ Health Prev Med. 2021;26:69.
Sheth T, Nair C, Muller J, Yusuf S. Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol. 1999;33:1916–9.
Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second national registry of myocardial infarction. J Am Coll Cardiol. 1998;31:1226–33.
Luan G, Yin P, Li T, Wang L, Zhou M. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci Rep. 2017;7:13531.
Silveira IH, Oliveira BFA, Cortes TR, Junger WL. The effect of ambient temperature on cardiovascular mortality in 27 Brazilian cities. Sci Total Environ. 2019;691:996–1004.
Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J. 2015;36:1178–85. https://academic.oup.com/eurheartj/article-lookup/doi/10.1093/eurheartj/ehv023.
Zhang Y, Xiang Q, Yu Y, Zhan Z, Hu K, Ding Z. Socio-geographic disparity in cardiorespiratory mortality burden attributable to ambient temperature in the United States. Environ Sci Pollut Res. 2019;26:694–705.
Lee WH, Lim YH, Dang TN, Seposo X, Honda Y, Guo YLL, et al. An investigation on attributes of ambient temperature and diurnal temperature range on mortality in five East-Asian countries. Sci Rep. 2017;7:10207.
Iñiguez C, Royé D, Tobías A. Contrasting patterns of temperature related mortality and hospitalization by cardiovascular and respiratory diseases in 52 Spanish cities. Environ Res. 2021;192:110191.
Ma Y, Zhou L, Chen K. Burden of cause-specific mortality attributable to heat and cold: A multicity time-series study in Jiangsu Province, China. Environ Int. 2020;144:105994.
Li G, Li Y, Tian L, Guo Q, Pan X. Future temperature-related years of life lost projections for cardiovascular disease in Tianjin, China. Sci Total Environ. 2018;630:943–50.
Huang J, Li G, Liu Y, Huang J, Xu G, Qian X, et al. Projections for temperature-related years of life lost from cardiovascular diseases in the elderly in a Chinese city with typical subtropical climate. Environ Res. 2018;167:614–21.
Zhang B, Li G, Ma Y, Pan X. Projection of temperature-related mortality due to cardiovascular disease in beijing under different climate change, population, and adaptation scenarios. Environ Res. 2018;162:152–9.
ROSE G. Seasonal variation in blood pressure in man. Nature. 1961;189:235–235. http://www.nature.com/articles/189235a0.
Marti-Soler H, Gubelmann C, Aeschbacher S, Alves L, Bobak M, Bongard V, et al. Seasonality of cardiovascular risk factors: an analysis including over 230 000 participants in 15 countries. Heart. 2014;100:1517–23.
Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ. The effect of temperature on systolic blood pressure. Blood Press Monit. 2007;12:195–203. http://journals.lww.com/bpmonitoring.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. The relationship between indoor, outdoor and ambient temperatures and morning BP surges from inter-seasonally repeated measurements. J Hum Hypertens. 2014;28:482–8.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32:1582–9.
Zhao H, Jivraj S, Moody A. My blood pressure is low today, do you have the heating on? The association between indoor temperature and blood pressure. J Hypertens. 2019;37:504–12.
Aubinière-Robb L, Jeemon P, Hastie CE, Patel RK, Mccallum L, Morrison D, et al. Blood pressure response to patterns of weather fluctuations and effect on mortality seasonal effects and blood pressure. Hypertension. 2013;62:190–6. http://hyper.ahajournals.org/lookup/suppl/doi:10.1161/HYPERTENSIONAHA.
Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, et al. Association between amplitude of seasonal variation in self-measured home blood pressure and cardiovascular outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure) study. J Am Heart Assoc. 2018;7:e008509.
See CY, Tseng CT, Lin WR, Chao JY, Kuo TH, Wang MC. Seasonal change in home blood pressure monitoring is associated with renal outcome and mortality in patients with chronic kidney disease. Front Med. 2021;8:672651.
Jansky L, Sramek P, Savlikova J, Ulicny B, Janakova H, Horky K. Change in sympathetic activity, cardiovascular functions and plasma hormone concentrations due to cold water immersion in men. Eur J Appl Physiol. 1996;74:148–52.
Hiramatsu K, Yamada T, Katakura M. Acute effects of cold on blood pressure, renin-angiotensin-aldosterone system, catecholamines and adrenal steroids in man. Clin Exp Pharmacol Physiol. 1984;11:171–179.
Marino F, Sockler JM, Fry JM. Thermoregulatory, metabolic and sympathoadrenal responses to repeated brief exposure to cold. Scand J Clin Lab Investig. 1998;58:537–46.
Zhang X, Zhang S, Wang C, Wang B, Guo P. Effects of moderate strength cold air exposure on blood pressure and biochemical indicators among cardiovascular and cerebrovascular patients. Int J Environ Res Public Health. 2014;11:2472–87.
Cummings MF, Peter SM, Mahar LJM, Frewin DB, Russell JW. The role of adrenal medullary catecholamine release in the response to a cold pressor test. Cardiovasc Res. 1983;17:189–91. https://academic.oup.com/cardiovascres/article/17/4/189/618956.
Lenders JWM, Peters JHM, Pieters GFF, Willemsen JJ, Thien T. Hemodynamic reactivity to sympathoadrenal stimulation in adrenalectomized women. J Clin Endocrin Metab. 1988. https://academic.oup.com/jcem/article/67/1/139/2654014.
Celi FS, Brychta RJ, Linderman JD, Butler PW, Alberobello AT, Smith S, et al. Minimal changes in environmental temperature result in a significant increase in energy expenditure and changes in the hormonal homeostasis in healthy adults. Eur J Endocrinol. 2010;163:863–72.
Fagius J, Kay R. Low ambient temperature increases baroreflex-governed sympathetic outflow to muscle vessels in humans. Acta Physiol Scand. 1991;142:201–9.
Hintsala HE, Kiviniemi AM, Tulppo MP, Helakari H, Rintamäki H, Mäntysaari M, et al. Hypertension does not alter the increase in cardiac baroreflex sensitivity caused by moderate cold exposure. Front Physiol. 2016;7:204
Yamazaki F, Sone R. Modulation of arterial baroreflex control of heart rate by skin cooling and heating in humans. J. Appl. Physiol. 2000;88. http://www.jap.org.
Gasic S, Ratheiser K, Wagner O, Nowotny P, Vierhapper H, Waldhäusl W. Alterations in angiotensin II release and vascular reactivity in hypertensive men: a pilot study. 1999. https://academic.oup.com/ajh/article/12/11/1055/242236.
Sramek P, Simeckova M, Jansky L, Savlikova J, Vybiral S. Human physiological responses to immersion into water of different temperatures. Eur J Appl Physiol. 2000;81:436–42.
Komulainen S, Tähtinen T, Rintamäki H, Virokannas H, Keinänen-Kiukaanniemi S. Blood pressure responses to whole-body cold exposure: effect of carvedilol. Eur J Clin Pharmacol. 2000;56:637–42.
Polonia JJ, Monteiro A, Esteves A, Eugenia Cunha M, Lurdes Santos PM, Coutinho J, et al. Influence of sublingual captopril on plasma catecholamine levels during hypertensive emergencies and cold immersion. Am J Med. 1988;84:148–151.
Headley SA, Moser D, Golan R, Kendrick ZV, Finck A, Paolone AM. Cardiovascular responses to-blockade and 5C cold air stress. Canadian Journal of Physiology and Pharmacology 1996;74:112–115.
Hata T, Ogihara T, Maruyama A, Mikami H, Nakamura M, Naka T, et al. The seasonal variation of blood pressure in patients with essential hypertension. Clin Exp Hypertens A 1982;4:341–54.
Kruse HJ, Wieczorek I, Hecker H, Creutzig A, Schellong SM. Seasonal variation of endothelin-1, angiotensin II, and plasma catecholamines and their relation to outside temperature. J Lab Clin Med. 2002;140:236–41.
Radke KJ, Izzo JL. Seasonal variation in haemodynamics and blood pressure-regulating hormones. J Hum Hypertens. 2010;24:410–6.
Winnicki M, Canali C, Accurso F, Dorigatti P, Giovinazzo P, Palatini P. Relation of 24-hour ambulatory blood pressure and short-term blood pressure variability to seasonal changes in environmental temperature an stage 1 hypertensive subjects. Results of the HARVEST trial. Clin Exp Hypertens. 1996;18:995–1012.
Komers R, Plotkin H. Dual inhibition of renin-angiotensin-aldosterone system and endothelin-1 in treatment of chronic kidney disease. Am J Physiol Integr Comp Physiol. 2016;310:R877–84. https://doi.org/10.1152/ajpregu.00425.2015.
Abassi ZA, Ellahham S, Winaver J, Hoffman A. The intrarenal endothelin system and hypertension. Physiology. 2001;16:152–6. https://doi.org/10.1152/physiologyonline.2001.16.4.152.
Rossi GP, Cavallin M, Nussdorfer GG, Pessina AC. The endothelin-aldosterone axis and cardiovascular diseases. J Cardiovasc Pharmacol. 2001;38:S49–52. http://journals.lww.com/00005344-200111002-00013.
McLaren M, Kirk G, Bolton-Smith C, Belch JJF. Seasonal variation in plasma levels of endothelin-1 and nitric oxide. Int Angiol. 2000;19:351–3.
Adamopoulos D, Vyssoulis G, Karpanou E, Kyvelou SM, Argacha JF, Cokkinos D, et al. Environmental determinants of blood pressure, arterial stiffness, and central hemodynamics. J Hypertens. 2010;28:903–9.
Youn JC, Rim SJ, Park S, Ko YG, Kang SM, Choi D, et al. Arterial stiffness is related to augmented seasonal variation of blood pressure in hypertensive patients. Blood Press. 2007;16:375–80.
Widlansky ME, Vita JA, Keyes MJ, Larson MG, Hamburg NM, Levy D, et al. Relation of season and temperature to endothelium-dependent flow-mediated vasodilation in subjects without clinical evidence of cardiovascular disease (From The Framingham Heart Study). Am J Cardiol. 2007;100. http://www.ncdc.noaa.gov/oa/ncdc.html.
Imamura M, Biro S, Kihara T, Yoshifuku S, Takasaki K, Otsuji Y, et al. Endothelial function repeated thermal therapy improves impaired vascular endothelial function in patients with coronary risk factors. Journal of the American College of Cardiology 2001;38:1083–8.
Papanek PE, Wood CE, Fregly MJ. Role of the sympathetic nervous system in cold-induced hypertension in rats. J Appl Physiol. 1991;71:300–6.
Sun Z, Fregly MJ, Cade JR. Effect of renal denervation on elevation of blood pressure in cold-exposed rats. Can J Physiol Pharmacol. 1995;73:72–8.
Sun Z, Wang X, Wood CE, Cade JR, Sun X, Wang CE, et al. Genetic AT 1A receptor deficiency attenuates cold-induced hypertension. Am J Physiol Regul Integr Comp Physiol. 2005;288:433–9. www.ajpregu.org.
Sun Z, Cade R, Zhang Z, Alouidor J, Van H. Angiotensinogen gene knockout delays and attenuates cold-induced hypertension. Hypertension. 2003;41:322–7.
Shechtman O, Fregly MJ, Van Bergen P, Papanek PE. Prevention of cold-induced increase in blood pressure of rats by captopril. Hypertension 1991;17:763–70.http://ahajournals.org.
Fregly MJ, Rossi F, Van Bergen P, Brummermann M, Cade R. Effect of chronic treatment with losartan potassium (DuP 753) on the elevation of blood pressure during chronic exposure of rats to cold. Pharmacology. 1993;46:198–205. https://www.karger.com/Article/FullText/139046.
Wang X, Sun Z, Cade R. Prolonged attenuation of cold-induced hypertension by adenoviral delivery of renin antisense. Kidney Int. 2005;68:680–87
Peng J, Kimura B, Phillips MI. The predominant role of brain angiotensinogen and angiotensin in environmentally induced hypertension. Regulatory Peptides 2002;110:25–32
Sun Z, Cade R, Morales C. Role of central angiotensin ii receptors in cold-induced hypertension. American Journal of Hypertension 2002;15:85–92.
Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807–20.
Burgaz A, Orsini N, Larsson SC, Wolk A. Blood 25-hydroxyvitamin D concentration and hypertension: a meta-analysis. J Hypertens. 2011;29:636–45.
Li YC, Kong J, Wei M, Chen Z-F, Liu SQ, Cao L-P. 1,25-Dihydroxyvitamin D3 is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110:229–38.
Qi D, Nie X, Cai J. The effect of vitamin D supplementation on hypertension in non-CKD populations: a systemic review and meta-analysis. Int J Cardiol. 2017;227:177–86.
Zhang D, Cheng C, Wang Y, Sun H, Yu S, Xue Y, et al. Effect of Vitamin D on blood pressure and hypertension in the general population: An update meta-analysis of cohort studies and randomized controlled trials. Prev Chronic Dis. 2020;17:E03.
He S, Hao X. The effect of vitamin D3 on blood pressure in people with vitamin D deficiency: a system review and meta-analysis. Medicine. 2019;98:e15284.
Frohlich M, Sund M, Russ S, Hoffmeister A, Fischer HG, Hombach V, et al. Seasonal variations of rheological and hemostatic parameters and acute-phase reactants in young, healthy subjects. Arteriosclerosis, thrombosis, and Vascular Biology 1997;17:2692–7.
Ghebre MA, Wannamethee SG, Rumley A, Whincup PH, Lowe GDO, Morris RW. Prospective study of seasonal patterns in hemostatic factors in older men and their relation to excess winter coronary heart disease deaths. J Thromb Haemost. 2012;10:352–8.
Saeki K, Obayashi K, Kurumatani N. Platelet count and indoor cold exposure among elderly people: a cross-sectional analysis of the HEIJO-KYO study. J Epidemiol. 2017;27:562–7.
Keatinge WR, Coleshaw SRK, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J. 1984;289:1405–8.
Preckel D, Von Känel R. Regulation of hemostasis by the sympathetic nervous system: any contribution to coronary artery disease? HeartDrug. 2004;4:123–30.
Sechi LA, Novello M, Colussi G, Di Fabio A, Chiuch A, Nadalini E, et al. Relationship of plasma renin with a prothrombotic state in hypertension: relevance for organ damage. Am J Hypert. 2008;21:1347–53.
Geerling JJ, Boon MR, Kooijman S, Parlevliet ET, Havekes LM, Romijn JA, et al. Sympathetic nervous system control of triglyceride metabolism: Novel concepts derived from recent studies. J Lipid Res. 2014;55:180–9.
Singh BM, Mehta JL. Interactions between the renin-angiotensin system and dyslipidemia relevance in the therapy of hypertension and coronary heart disease. Arch Intern Med. 2003;163:1296–304.
Bruno RM, Ghiadoni L, Seravalle G, Dell’Oro R, Taddei S, Grassi G. Sympathetic regulation of vascular function in health and disease. Front Physiol. 2012;3:1–15.
Aroor AR, DeMarco VG, Jia G, Sun Z, Nistala R, Meininger GA, et al. The role of tissue renin-angiotensin-aldosterone system in the development of endothelial dysfunction and arterial stiffness. Front Endocrinol. 2013;4:161.
Goel H, Tayel H, Nadar SK. Aiming higher in hopes to achieve lower: the European Society of Cardiology/European Society of Hypertension versus the American College of Cardiology/American Heart Association guidelines for diagnosis and management of hypertension. J Hum Hypertens. 2019;33:635–8.
Goyal A, Aslam N, Kaur S, Soni RK, Midha V, Chaudhary A, et al. Factors affecting seasonal changes in blood pressure in North India: a population based four-seasons study. Indian Heart J. 2018;70:360–7.
Sinha P, Taneja DK, Singh NP, Saha R. Seasonal variation in prevalence of hypertension: implications for interpretation. Indian J Public Health. 2010;54:7–10.
Su D, Du H, Zhang X, Qian Y, Chen L, Chen Y, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural chinese population. Int J Epidemiol. 2014;43:1835–45.
Alpérovitch A, Lacombe J-M, Hanon O, Dartigues J-F, Ritchie K, Ducimetière P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals the Three-city Study. Archives of Internal Medicine 2009;169:75–80.
Kamezaki F, Sonoda S, Tomotsune Y, Yunaka H, Otsuji Y. Seasonal variation in metabolic syndrome prevalence. Hypertens Res. 2010;33:568–72.
Ciardullo S, Muraca E, Cannistraci R, Manzoni G, Perra S, Bianconi E, et al. Seasonal variation in estimated cardiovascular risk in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2021;31:1494–500.
Narita K, Hoshide S, Fujiwara T, Kario K. Seasonal variation in prevalence of masked uncontrolled hypertension in general practice outpatients. J Hypertens. 2019;37:e125–6.
Rothwell PM, Howard SC, Dolan E, O’brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905. www.thelancet.com.
Clark D, Nicholls SJ, St John J, Elshazly MB, Ahmed HM, Khraishah H, et al. Visit-to-visit blood pressure variability, coronary atheroma progression, and clinical outcomes. JAMA Cardiol. 2019;4:437–43.
Wang J, Shi X, Ma C, Zheng H, Xiao J, Bian H, et al. Visit-to-visit blood pressure variability is a risk factor for all-cause mortality and cardiovascular disease: a systematic review and meta-analysis. J Hypertens. 2017;35:10–7.
Parati G, Ochoa JE, Lombardi C, Bilo G. Blood pressure variability: assessment, predictive value, and potential as a therapeutic target. Current Hypertension Reports. Current Med Group LLC 1. 2015;17:1–18.
Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, et al. Seasonal variation in blood pressure: Evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2020;38:1235–43.
Saeki K, Obayashi K, Iwamoto J, Tanaka Y, Tanaka N, Takata S, et al. Influence of room heating on ambulatory blood pressure in winter: A randomised controlled study. J Epidemiol Community Health. 2013;67:484–90.
Saeki K, Obayashi K, Kurumatani N. Short-termeffects of instruction in home heating on indoor temperature and blood pressure in elderly people: a randomized controlled trial. J Hypertens. 2015;33:2338–43.
The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349:1341–6. https://linkinghub.elsevier.com/retrieve/pii/S0140673696123382.
Hanazawa T, Asayama K, Watabe D, Hosaka M, Satoh M, Yasui D, et al. Seasonal variation in self-measured home blood pressure among patients on antihypertensive medications: HOMED-BP study. Hypertens Res. 2017;40:284–90.
McAlister FA, Lethebe BC, Leung AA, Padwal RS, Williamson T. Visit-to-visit blood pressure variability is common in primary care patients: retrospective cohort study of 221,803 adults. PLoS ONE. 2021;16:e0248362.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, et al. Weather-related changes in 24-hour blood pressure profile. effects of age and implications for hypertension management. Hypertension. 2006;47:155–61. http://www.hypertensionaha.org.
Murakami S, Otsuka K, Kono T, Soyama A, Umeda T, Yamamoto N, et al. Impact of outdoor temperature on prewaking morning surge and nocturnal decline in blood pressure in a Japanese population. Hypertens Res. 2011;34:70–3.
Zhao Q, Guo Y, Ye T, Gasparrini A, Tong S, Overcenco A, et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. 2021;5:e415–25.
Arbuthnott K, Hajat S, Heaviside C, Vardoulakis S. Years of life lost and mortality due to heat and cold in the three largest English cities. Environ Int. 2020;144:105966.
Hajat S, Vardoulakis S, Heaviside C, Eggen B. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68:641–8. https://doi.org/10.1136/jech-2013-202449.
Martin SL, Cakmak S, Hebbern CA, Avramescu ML, Tremblay N. Climate change and future temperature-related mortality in 15 Canadian cities. Int J Biometeorol. 2012;56:605–19.
Lu P, Xia G, Zhao Q, Xu R, Li S, Guo Y. Temporal trends of the association between ambient temperature and hospitalisations for cardiovascular diseases in Queensland, Australia from 1995 to 2016: a time-stratified case-crossover study. PLoS Med. 2020;17:e1003176 https://doi.org/10.1371/journal.pmed.1003176.
Achebak H, Devolder D, Ballester J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet Health. 2019;3:e297–306.
Ferreira L de CM, Nogueira MC, Pereira RV de B, de Farias WCM, Rodrigues MM de S, Teixeira MTB, et al. Ambient temperature and mortality due to acute myocardial infarction in Brazil: an ecological study of time-series analyses. Sci Rep. 2019;9:13790. http://www.nature.com/articles/s41598-019-50235-8.
Breitner S, Wolf K, Peters A, Schneider A. Short-term effects of air temperature on cause-specific cardiovascular mortality in Bavaria, Germany. Heart. 2014;100:1272–80. https://doi.org/10.1136/heartjnl-2014-305578.
Lin YK, Chang CK, Wang YC, Ho TJ. Acute and prolonged adverse effects of temperature on mortality from cardiovascular diseases. PLoS ONE. 2013;8e82678.
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, et al. Effects of cold weather on mortality: Results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168:1397–408.
Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: A study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64:827–33.
Goodman PG, Dockery DW, Clancy L. Cause-specific mortality and the extended effects of particulate pollution and temperature exposure. Environ Health Perspect . 2004;112:179–85. https://doi.org/10.1289/ehp.6451.
Huang C-C, Chen Y-H, Hung C-S, Lee J-K, Hsu T-P, Wu H-W, et al. Assessment of the relationship between ambient temperature and home blood pressure in patients from a web-based synchronous telehealth care program: retrospective study. J Med Internet Res. 2019;21:e12369. http://www.jmir.org/2019/3/e12369/.
Wyse CA, Celis Morales CA, Ward J, Lyall D, Smith DJ, Mackay D, et al. Population-level seasonality in cardiovascular mortality, blood pressure, BMI and inflammatory cells in UK biobank. Ann Med. 2018;50:410–9.
Hong YC, Kim H, Oh SY, Lim YH, Kim SY, Yoon HJ, et al. Association of cold ambient temperature and cardiovascular markers. Sci Total Environ. 2012;435–436:74–9.
Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: The China Kadoorie Biobank. J Hypertens. 2012;30:1383–91.
Madsen C, Nafstad P. Associations between environmental exposure and blood pressure among participants in the Oslo Health Study (HUBRO). Eur J Epidemiol. 2006;21:485–91.
Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology. 2004;50:315–21.
Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. J Hypertens. 1998;16:1585–92.
Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J. 1982;285:919–23.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the literature search, preparing the manuscript and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goel, H., Shah, K., Kumar, A. et al. Temperature, cardiovascular mortality, and the role of hypertension and renin–angiotensin–aldosterone axis in seasonal adversity: a narrative review. J Hum Hypertens 36, 1035–1047 (2022). https://doi.org/10.1038/s41371-022-00707-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00707-8