Abstract
Purpose
This study aimed to investigate the association of breakfast consumption frequency (BCF) with glycemic control indices in a cross-sectional sample of adults from families at high risk for type 2 diabetes mellitus (T2DM), exploring the role of sex and socioeconomic status (SES).
Methods
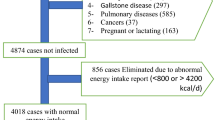
In 2370 adults (40.8 ± 5.6 years) from 6 European countries, sociodemographic, lifestyle, anthropometric and biochemical characteristics were assessed through standardized procedures. Multivariable regression models were used to examine the association between fasting glucose (FG), fasting insulin (FI), and insulin resistance (HOMA-IR) (dependent variables) with BCF (independent variable) controlling for multiple possible confounders.
Results
A linear association of BCF with FG (β = −0.557, 95% CI (−0.834, −0.280)) and a quadratic association with FI and HOMA-IR with the highest point of curve observed at BCF = 2.989 (times/week) and at BCF = 2.746, respectively, independent of the used covariates. In males and in participants of high SES, BCF was linearly and inversely associated with FG, while with FI and HOMA-IR there was an association with BCF in quadratic function. In females, BCF was linearly and inversely associated with FG and HOMA-IR, and there was a quadratic association with FI. In low SES there was only a linear association with FG, yet with no statistically significant findings for FI and HOMA-IR.
Conclusions
Regular breakfast consumption, especially >3 times/week is associated with improved indices of glycemic control. This association was diminished in low SES participants in the presence of the used covariates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available, since the data used is confidential based on Feel4Diabetes publications rules, but are available from the corresponding author on reasonable request.
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9. Diabetes Res Clin Pract. 2019;157:107843.
Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016;355:i5953.
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–90.
Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–86.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Ballon A, Neuenschwander M, Schlesinger S. Breakfast skipping is associated with increased risk of type 2 diabetes among adults: a systematic review and meta-analysis of prospective cohort studies. J Nutr. 2019;149:106–13.
Ogata H, Hatamoto Y, Goto Y, Tajiri E, Yoshimura E, Kiyono K, et al. Association between breakfast skipping and postprandial hyperglycaemia after lunch in healthy young individuals. Br J Nutr. 2019;122:431–40.
Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–9.
Kollannoor-Samuel G, Chhabra J, Fernandez ML, Vega-López S, Pérez SS, Damio G, et al. Determinants of fasting plasma glucose and glycosylated hemoglobin among low income Latinos with poorly controlled type 2 diabetes. J Immigr Minor Health. 2011;13:809–17.
Li Y, Nemoto T, Tobimatsu S, Saito M, Ebata M, Munakata H, et al. Relationship between skipping breakfast and impaired fasting glucose along with cardiovascular and pre-diabetes condition risk factors in apparently healthy subjects. Endocrinol Stud. 2011;1:e17–e.
St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–121.
Mekary RA, Giovannucci E, Willett WC, van Dam RM, Hu FB. Eating patterns and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr. 2012;95:1182–9.
Mekary RA, Giovannucci E, Cahill L, Willett WC, van Dam RM, Hu FB. Eating patterns and type 2 diabetes risk in older women: breakfast consumption and eating frequency. Am J Clin Nutr. 2013;98:436–43.
Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics. 2008;121:e638–45.
Sijtsma FP, Meyer KA, Steffen LM, Shikany JM, Van Horn L, Harnack L, et al. Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr. 2012;95:580–6.
Manios Y, Androutsos O, Lambrinou CP, Cardon G, Lindstrom J, Annemans L, et al. A school- and community-based intervention to promote healthy lifestyle and prevent type 2 diabetes in vulnerable families across Europe: design and implementation of the Feel4Diabetes-study. Public Health Nutr. 2018;21:3281–90.
Saaristo T, Peltonen M, Lindström J, Saarikoski L, Sundvall J, Eriksson JG, et al. Cross-sectional evaluation of the Finnish Diabetes Risk Score: a tool to identify undetected type 2 diabetes, abnormal glucose tolerance and metabolic syndrome. Diab Vasc Dis Res. 2005;2:67–72.
Schwarz PE, Li J, Lindstrom J, Tuomilehto J. Tools for predicting the risk of type 2 diabetes in daily practice. Horm Metab Res. 2009;41:86–97.
Anastasiou CA, Fappa E, Zachari K, Mavrogianni C, Van Stappen V, Kivelä J, et al. Development and reliability of questionnaires for the assessment of diet and physical activity behaviors in a multi-country sample in Europe the Feel4Diabetes Study. BMC Endocr Disord. 2020;20:135.
Androutsos O, Anastasiou C, Lambrinou CP, Mavrogianni C, Cardon G, Van Stappen V, et al. Intra- and inter- observer reliability of anthropometric measurements and blood pressure in primary schoolchildren and adults: the Feel4Diabetes-study. BMC Endocr Disord. 2020;20:27.
Association WM, World Medical A. ssociation Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Kivelä J, Wikström K, Virtanen E, Georgoulis M, Cardon G, Civeira F, et al. Obtaining evidence base for the development of Feel4Diabetes intervention to prevent type 2 diabetes—a narrative literature review. BMC Endocr Disord 2020;20:140.
Organization WH. Obesity and overweight fact sheet. 2016. Department of Sustainable Development and Healthy Environments. http://www.searowhoint/entity/noncommunicable_diseases/media/non_communicable_diseases_obesity_fspdf. Accessed 10 June 2018.
Moschonis G, Karatzi K, Apergi K, Liatis S, Kivelä J, Wikström K, et al. Socio-demographic characteristics and body weight perceptions of study participants benefitting most from the Feel4Diabetes program based on their anthropometric and glycaemic profile changes. Nutrients. 2020;12:3117.
Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem. 2011;57:e1–47.
Association AD. 2. Classification and diagnosis of diabetes. Diabetes Care. 2019;42:S13–28.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Sirin SR. Socioeconomic status and academic achievement: a meta-analytic review of research. Rev Educ Res. 2005;75:417–53.
Manios Y, Mavrogianni C, Lambrinou CP, Cardon G, Lindström J, Iotova V, et al. Two-stage, school and community-based population screening successfully identifies individuals and families at high-risk for type 2 diabetes: the Feel4Diabetes-study. BMC Endocr Disord. 2020;20:12.
Virtanen E, Kivelä J, Wikström K, Lambrinou CP, De Miguel-Etayo P, Huys N, et al. Feel4Diabetes healthy diet score: development and evaluation of clinical validity. BMC Endocr Disord. 2020;20:46.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Odegaard AO, Jacobs DR, Steffen LM, Van Horn L, Ludwig DS, Pereira MA. Breakfast frequency and development of metabolic risk. Diabetes Care. 2013;36:3100–6.
Iqbal K, Schwingshackl L, Gottschald M, Knüppel S, Stelmach-Mardas M, Aleksandrova K, et al. Breakfast quality and cardiometabolic risk profiles in an upper middle-aged German population. Eur J Clin Nutr. 2017;71:1312–20.
Voronova N, Nikitin A, Chistiakov A, Chistiakov D. Skipping breakfast is correlated with impaired fasting glucose in apparently healthy subjects. Open Med. 2012;7:376–82.
Nas A, Mirza N, Hägele F, Kahlhöfer J, Keller J, Rising R, et al. Impact of breakfast skipping compared with dinner skipping on regulation of energy balance and metabolic risk. Am J Clin Nutr. 2017;105:1351–61.
Joo HJ, Kim GR, Park EC, Jang SI. Association between Frequency of Breakfast Consumption and Insulin Resistance Using Triglyceride-Glucose Index: A Cross-Sectional Study of the Korea National Health and Nutrition Examination Survey (2016–2018). Int J Environ Res Public Health. 2020;17:3322.
Leech RM, Worsley A, Timperio A, McNaughton SA. Understanding meal patterns: definitions, methodology and impact on nutrient intake and diet quality. Nutr Res Rev. 2015;28:1–21.
de Castro JM. When, how much and what foods are eaten are related to total daily food intake. Br J Nutr. 2009;102:1228–37.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–32.
Mauvais-Jarvis F. Gender differences in glucose homeostasis and diabetes. Physiol Behav. 2018;187:20–3.
Bes-Rastrollo M, Basterra-Gortari FJ, Sánchez-Villegas A, Marti A, Martínez JA, Martínez-González MA. A prospective study of eating away-from-home meals and weight gain in a Mediterranean population: the SUN (Seguimiento Universidad de Navarra) cohort. Public Health Nutr. 2010;13:1356–63.
Orfanos P, Naska A, Trichopoulos D, Slimani N, Ferrari P, van Bakel M, et al. Eating out of home and its correlates in 10 European countries. The European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2007;10:1515–25.
Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:804–18.
Mullan BA, Singh M. A systematic review of the quality, content, and context of breakfast consumption. Nutr Food Sci. 2010;40:81–114.
Trijsburg L, Geelen A, Hulshof PJM, Van't Veer P, Boshuizen HC, Hollman PCH, et al. Validity of absolute intake and nutrient density of protein, potassium, and sodium assessed by various dietary assessment methods: an exploratory study. Nutrients. 2019;12:109.
Acknowledgements
The authors would like to thank the members of the Feel4Diabetes-study group: coordinator, YM; steering committee, YM, GC, Jaana Lindström, Peter Schwarz, KM, Lieven Annemans, and Winne Ko; Harokopio University (Greece), YM, KK, Odysseas Androutsos, George Moschonis, Spyridon Kanellakis, Christina Mavrogianni, Konstantina Tsoutsoulopoulou, Christina Katsarou, Eva Karaglani, Irini Qira, Efstathios Skoufas, Konstantina Maragkopoulou, Antigone Tsiafitsa, Irini Sotiropoulou, Michalis Tsolakos, Effie Argyri, Mary Nikolaou, Eleni-Anna Vampouli, Christina Filippou, Kyriaki Apergi, Amalia Filippou, Gatsiou Katerina, and Efstratios Dimitriadis; Finnish Institute for Health and Welfare (Finland), Jaana Lindström, Tiina Laatikainen, Katja Wikström, Jemina Kivelä, Päivi Valve, Esko Levälahti, Eeva Virtanen, Tiina Pennanen, Seija Olli, and Karoliina Nelimarkka; Ghent University (Belgium), Department of Movement and Sports Sciences, GC, Vicky Van Stappen, and Nele Huys; Department of Public Health, Lieven Annemans and Ruben Willems; Department of Endocrinology and Metabolic Diseases, Samyah Shadid; Technische Universität Dresden (Germany), Peter Schwarz and Patrick Timpel; University of Athens (Greece), KM, Stavros Liatis, George Dafoulas, Christina-Paulina Lambrinou, and Angeliki Giannopoulou; International Diabetes Federation European Region (Belgium), Winne Ko and Ernest Karuranga; Universidad De Zaragoza (Spain), Luis Moreno, Fernando Civeira, Gloria Bueno, Pilar De Miguel-Etayo, Esther M Gonzalez-Gil, María L. Miguel-Berges, Natalia Giménez-Legarre; Paloma Flores-Barrantes, Aleli M. Ayala-Marín, Miguel Seral-Cortés, Lucia Baila-Rueda, Ana Cenarro, Estíbaliz Jarauta, and Rocío Mateo-Gallego; Medical University of Varna (Bulgaria), Violeta Iotova, Tsvetalina Tankova, Natalia Usheva, Kaloyan Tsochev, Nevena Chakarova, Sonya Galcheva, Rumyana Dimova, Yana Bocheva, Zhaneta Radkova, Vanya Marinova, Yuliya Bazdarska, and Tanya Stefanova; University of Debrecen (Hungary), Imre Rurik, Timea Ungvari, Zoltán Jancsó, Anna Nánási, László Kolozsvári, Csilla Semánova, Éva Bíró, Emese Antal, and Sándorné Radó; Extensive Life Oy (Finland), Remberto Martinez and Marcos Tong.
Funding
The publication of this supplement was funded by Feel4Diabetes study. The Feel4Diabetes-study has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement n° 643708. The content of this article reflects only the authors’ views and the European Community is not liable for any use that may be made of the information contained therein.
Author information
Authors and Affiliations
Contributions
Conceptualization: KA, KK, and YM; Methodology: KA, KK, and YM; formal analysis, KA and KK; Investigation and data collection: KA, KK, KR, CM, SS, GC, PFB, PME, YB, TT, RS, RI, KW, VI, and YM.; Resources: YM, GC, VI, KM, YM; Data curation: KA, KK, and YM; Writing-original draft preparation: KA, KK, and YM; Writing—review and editing: KA., KK, KR, CM, SS, GC, PFB, PME, YB, TT, RS, RI, KW, VI, and YM; Visualization: KA, KK, YM; Supervision: YM; Project administration: YM; Funding acquisition: YM, GC, VI, KM, YM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. All authors have made substantial contributions to this work and approve the final version of the paper to be submitted.
Ethics approval and consent to participate
The Feel4Diabetes-study adhered to the Declaration of Helsinki and the conventions of the Council of Europe on human rights and biomedicine. All participating countries obtained ethical clearance from the relevant ethical committees and local authorities. More specifically, in Belgium, the study was approved by the Medical Ethics Committee of the Ghent University Hospital (ethical approval code: B670201524437); in Bulgaria, by the Ethics Committee of the Medical University of Varna (ethical approval code: 52/10-3-2016r) and the municipalities of Sofia and Varna, as well as the Ministry of Education and Science local representatives; in Finland, by the hospital district of Southwest Finland ethical committee (ethical approval code: 174/1801/2015); in Greece, by the Bioethics Committee of Harokopio University (ethical approval code: 46/3–4-2015) and the Greek Ministry of Education; in Hungary, by the National Committee for Scientific Research in Medicine (ethical approval code: 20095/2016/EKU); and in Spain, by the Clinical Research Ethics Committee and the Department of Consumers’ Health of the Government of Aragón (ethical approval code: CP03/2016). This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the ethics committees in all countries (in Belgium, by the Medical Ethics Committee of the Ghent University Hospital; in Bulgaria, by the Ethics Committee of the Medical University of Varna; in Finland, by the hospital district of Southwest Finland ethical committee; in Greece, by the Bioethics Committee of Harokopio University; in Hungary, by the National Committee for Scientific Research in Medicine; in Spain, by the Clinical Research Ethics Committee). Written informed consent was obtained from all subjects. All participants gave their written informed consent prior to their enrollment in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Apergi, K., Karatzi, K., Reppas, K. et al. Association of breakfast consumption frequency with fasting glucose and insulin sensitivity/b cells function (HOMA-IR) in adults from high-risk families for type 2 diabetes in Europe: the Feel4Diabetes Study. Eur J Clin Nutr 76, 1600–1610 (2022). https://doi.org/10.1038/s41430-022-01160-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01160-z