Abstract
This study aimed to examine whether nontuberculous mycobacteria (NTM) inside household showerheads are identical to those in patients with NTM-pulmonary disease (PD) since household water is one of the potential NTM sources. Samples were obtained from 32 household showerheads of patients with NTM-PD recruited through the Pulmonary Outpatient Department at the Severance Hospital between October 2018 and October 2019. All isolates from patients with NTM-PD were diagnosed using a reverse-hybridization line probe assay based on the ropB gene. To determine the mycobacterial compositions, the washing fluids were collected and investigated using multiplex polymerase chain reaction assay and NTM culture; suspected microbial isolates in these fluids and culture were identified using sequencing analysis of 16S rRNA gene. NTM species causing the PD in the patients were Mycobacterium avium, M. intracellulare, M. abscessus, M. massiliense, and M. fortuitum complex. The mycobacteria isolated from the showerhead were M. lentiflavum, M. gordonae, M. triplex, M. phocaicum, M. mucogenicum, M. florentinum, M. gilvum, M. llatzerense, and M. peregrinum. However, the species identified in the showerheads did not match those of the patients. Despite NTM species in the showerheads, clinical implications in the main pathogenesis associated with the disease in the patients studied were not elucidated.
Similar content being viewed by others
Introduction
Nontuberculous mycobacteria (NTM) species are opportunistic pathogens responsible for progressive pulmonary disease as well as skin and soft tissue infection, lymphadenitis, and other health issues1. An increase in the incidence and prevalence of pulmonary disease caused by NTM has been reported worldwide2. In Korea, the incidence and prevalence of NTM infection increased rapidly from 2003 to 2016, particularly among women and older age groups. For reported cases of NTM infection, the incidence and prevalence rates were 17.9 and 33.3 per 100,000 populations in 2016, respectively. Additionally, the mortality rate in the NTM infected-population was higher than that in the general population3.
Mycobacterium avium complex (MAC) members, such as M. avium and M. intracellulare; M. abscessus complex (MABC) members, such as M. abscessus and M. massiliense are the major causative organisms of NTM-pulmonary disease (PD) and are frequently isolated from patients with NTM-PD. Recent studies have focused on identifying risk factors for both host and environmental factors associated with NTM-PD. NTM has been isolated from different environmental sources, including water, soil, food, dust, and aerosols4,5. Infections with NTM are caused by ingestion or inhalation of contaminated food or aerosol, and through injured skin, which indicates that a significant entry gate of NTM into a host organism is from environmental sources, such as water6. Previous studies have frequently identified mycobacteria in household water systems, and it has raised considerable concern among individuals susceptible to this infection. Some studies reported that patients with chronic obstructive pulmonary disease or immunodeficiency could have developed acute disorder when exposed to water contaminated with NTM7,8. To date this evidence has been reported mainly for MAC4,9,10,11,12,13. Thomson et al. showed that disease-causing NTM species were isolated from household water and aerosols, such as M. avium, M. kansasii, M. lentiflavum, and M. abscessus14. Although implicated as a potential source of disease, the mycobacterial composition and environmental predictors of showerhead-associated mycobacteria remain unresolved. Accordingly, there is a need for further epidemiological investigations of potential sources of NTM infections, including showerheads. Our study aimed to isolate and identify the NTM species present in household showerheads and compare the NTM found in biofilm with the NTM from patients with NTM-PD.
Methods
Sample collection and mycobacteria isolation from household showerheads
Patients with NTM-PD were recruited through the Pulmonary Outpatient Department at the Severance Hospital between October 2018 and October 2019. All patients with NTM-PD were diagnosed according to the American Thoracic Society/Infectious Disease Society of America (ATS/IDSA) 2007 guidelines15. For AFB smear and cultures were examined by fluorochrome staining using auramine–rhodamine and culturing in 3% Ogawa medium and mycobacteria growth-indicator tube medium (MGIT; Becton Dickson, NJ, USA). A reverse-hybridization line probe assay based on the rpoB gene, conducted at Seoul Clinical Laboratories (Yongin, Korea), was used for NTM species identification.
Following analysis of NTM, showerheads were collected from the homes of the patients with NTM, and a total of 32 samples were collected and 7 of the 32 samples included the shower hose. After disassembling the showerhead, the inside was wiped with a cotton swab, and the cotton swab was put in 50 mL of phosphate-buffered saline (PBS) and vortexed for 1 min. In the case of shower hoses, the front and rear entrances were parafilmed after adding 0.05% tween 20 in PBS into the shower hose. Then, the shower hose was sealed in a sterilized plastic bag and sonicated in a water bath for 5 min. After vortexing or sonicating, microbial cells in PBS were pelleted by centrifugation at 4000 rpm for 30 min. After centrifugation, the supernatant was removed, and the pellet was resuspended in 3 mL of PBS. The sample collection process from showerheads is briefly presented in Supplemental Fig. 1. The resuspended pellets were stored at 4 °C before further use. To identify the mycobacterium from natural samples, the analysis was performed using resuspended samples and cultivated of the isolates. Additionally, all resuspended samples (1 mL) were stained by Ziehl–Neelsen staining, and smear-positivity was confirmed by light microscope at 100× magnification16.
Supplementation of media and growth conditions
For cultivation, the resuspended samples were decontaminated with 0.01% cetylpyridinium chloride (CPC, Sigma) and cultivated in Mycobacteria Growth Indicator Tubes (MGIT, BD BACTEC). They were supplemented with PANTA/enrichment (BD BACTEC) to obtain the following final concentrations of antibiotics in the culture medium: 40 U/mL of polymyxin, 4 µ/mL of amphotericin B, 16 µ/mL of nalidixic acid, 4 µ/mL of trimethoprim, and 4 µ/mL of azlocillin for 4 weeks (slow growers) in the MGIT system. After 4 weeks, the samples were subcultured onto 7H11 agar supplemented with 10% oleic acid-albumin-dextrose-catalase (OADC, Difco) for 4 weeks at 37 °C. After 4 weeks, they were subcultured onto Ogawa medium for 4 weeks at 37 °C17. Colonies of putative acid-fast bacteria were picked after 5, 10, 21, and 28 days.
DNA preparation, multiplex polymerase chain reaction (PCR), and identification of mycobacterial target sequences
DNA was extracted from 1 mL of the resuspended sample using the conventional cetyltrimethylammonium bromide method (CTAB) as previously described18. Three primers were used in the PCR (IS1311, DT1, and 16s rRNA) according to a previously described method (Table 1)19,20. For amplification, each PCR mixture contained 25 μL of 2X EF-Taq PCR Smart mix (Solgent Co., Ltd. Daejeon, South Korea), 2 μL each of the 4 primer sets (all primer solutions in 10 pmol), 2 μL of DNA template, and 17 μL of water in a final volume of 50 μL. PCR was performed at 61.5 °C for 45 s for the annealing step, and followed by 30 cycles. The rest of the PCR parameters and electrophoresis were performed based on previous publications19. According to the multiplex PCR interpretation criteria, amplification of 16S rRNA was interpreted as identification of M. tuberculosis; amplification of IS1311 or DT1 with the 16S rRNA gene was interpreted as identification of M. avium or M. intracellulare, respectively. Mycobacterium species outside the multiplex PCR target species were indicated by observation of only 16S rRNA gene amplification19.
Isolates identified as other Mycobacterium spp. were further determined using 16S rRNA sequencing in liquid and colony samples. Sequencing reactions were performed using the BigDye (R) Terminator v3.1 Cycle Sequencing Kit from Applied Biosystems. At the end of the reaction, the dNTPs and the reactants that were not involved in the response were removed by the method recommended by Applied Biosystems. Then, the samples were loaded onto ABI Prism 3730XL DNA Analyzer to obtain sequencing results. The analyzed sequences were determined using the Sequencher 5.4.6 program from Gene Codes. The base sequence was searched in BLAST.
Ethics approval
This research protocol was approved by the Institutional Review Board of the Severance Hospital, South Korea (IRB No. 4-2018-0444), and the study design was approved by the appropriate ethics review boards. All methods were carried out in accordance with the approved guidelines and regulations as well as in accordance with the Declaration of Helsinki. All patients gave their written informed consent.
Results
Baseline characteristics
A total of 32 patients were diagnosed with NTM pulmonary disease before the study period. The baseline characteristics of the patients are summarized in Table 2. There were 25 (78%) female patients, and the median age of all patients was 59 years (range 30 to 72 years). Seventeen (53%) had Mycobacterium avium infection, seven (22%) had M. intracellulare infection, and one each (3%) had M. abscessus, M. massiliense, and M. fortuitum complex infections. A further 5 (16%) had mixed infections. Ten of these patients were naïve for NTM treatment and the others had a history of previous or ongoing treatment for NTM-PD. Eight (25%) patients had a history of prior treatment for pulmonary tuberculosis. There were 20 patients with NTM prevalence period of 1 year or longer. Up to 6 months prior to enrollment in this study, NTM was isolated from the sputum of 30 patients.
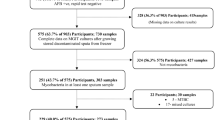
Isolation of NTM from the washing fluids of showerheads using multiplex PCR
As described in “Methods”, samples were obtained by a swab of the surfaces of 32 showerheads, including the shower hoses from seven of the 32 showers. To isolate the NTM from the showerheads, we amplified rRNA genes from resuspended sample DNAs by PCR, using three primers (IS1311, DT1, and 16s rRNA, Table 1). Figure 1 shows the amplification products of isolates using multiplex PCR primer sets. Seventeen samples showed a single amplification band of 500 base pair (bp) product specific to the 16S rRNA gene for all mycobacteria. The sizes of the resulting PCR products and the groups that they identify are described in Table 1. In addition, the AFB smear was performed using resuspended samples, and identified positive results in eight samples (1+, n = 7; 4+, n = 1; negative, n = 16, and non-detected, n = 8; Table 3).
Agarose gel electrophoresis of polymerase chain reaction (PCR) amplification products using multiplex PCR primer sets on resuspended samples. Only one 500-bp band specific to the 16S rRNA gene was detected in a total of 17samples. Each line is the showerhead sample from each subject. Lane M, molecular size marker (100-bp ladder).
Identification of NTM in both liquid and culture samples from the showerheads by genetic analysis
In order to identify accurate mycobacterium spp., genotype sequencing was performed in liquid and colonies of isolates sampled by PCR assay using 16s rRNA and rpoB. The species of NTM isolated from washing fluids and colonies from 32 showerheads included M. florentinum, M. phocaicum, M. gordonae, M. mucogenicum, M. gilvum, M. llatzerense, M. peregrinum, M. sherrisii, M. aurum, M. porcinum, M. lentiflavum, M. colombiense, M. triplex, M. gordonae, and M. arupense, and details are summarized in Table 3. However, none of the species from the showerhead washing fluids and cultivating colonies matched the NTM isolates from patients with NTM-PD.
Discussion
In light of the increasing prevalence of NTM-PD without a known cause, clinicians have a substantial interest in identifying the source of the NTM infection and the number of species identified in both clinical samples and environments. In this study, NTM was isolated from the showerheads as a potential source of infection for patients with NTM-PD, and a total of 18 species (subspecies, complexes) of NTM were identified. Among them, none of the mycobacteria matched the patients’ infectious mycobacteria, but various NTM species were identified, suggesting that it could be a potential source of infection in susceptible persons.
NTM are ubiquitous in the environment and have been isolated from different environmental sources, particularly water in homes, swimming pools, whirlpool therapy baths, soils, and the workplace21,22. Geographic and behavioral variabilities are also associated with the incidence of NTM infection among patients23. Particularly, water is one of the main vehicles for NTM transmission, as confirmed by isolation of the same species from both water and patients in several studies. For example, Covert et al. reported that 35% of samples from municipal water supplies in 21 states in the United States were found to test positive for NTM24. In one study, strains from the water system identical to those in the patients were found in 7 (41%) of 17 patients sampled12. For another example, Feazel et al. showed that the showerhead environment strongly enriched for microbes that are known to form biofilms in water systems, including Mycobacterium spp., Shpingomonas spp., Methylobacterium spp. and others in United States25. Our results, and those described by various studies, show that NTM are quite frequent in household water. However, in this study, we rarely detected the major causative organisms of NTM disease, including MAC members, such as M. avium and M. intracellulare, or M. abscessus, M. massiliense from the surfaces of the showerheads. In addition, when the isolates from the patients’ showerheads were compared with those from their sputum samples, none had matching pathogens in the present study. Many factors affect the ability of NTM to adhere and form a biofilm on various materials26. The materials used for the showerhead, the water sources, and the type of hot-water supply system may influence the regional presence of NTM spp. on showerheads. In addition to exposure, host factors are influential in NTM infection7,8,27,28,29. According to the study by Falkinham et al.30, the potential impact of human activities on the ecology of NTM has also been described. Our study examined the household showerhead as a potential source of NTM. Although we did not demonstrate Mycobacteria spp., which was the main pathogen associated with disease in the patients diagnosed with NTM infection, we found that 17 (57%) biofilm (swab) samples collected from the showerheads of patients with NTM-PD yielded NTM, using 16S rRNA sequences. In this study, many of the isolates were identified as M. lentiflavum 7 (10.9%), M. gordonae 6 (9.4%), M. triplex 4 (6.3%), and M. mucogenicum 3 (4.7%). In our study, as in the results of several studies, M. lentiflavum was also the most frequently identified isolate from the house water system and could be a potential pathogen that can cause pulmonary lung disease14,31,32.
M. gordonae is known to rarely causes pulmonary lung disease due to its low pathogenicity, and when M. gordonae is detected in sputum, it has been considered as a contamination33. However, there are case reports that M. gordonae can cause pulmonary lung disease in immunosuppressed patients such as human immunodeficiency virus infection, steroid treatment, and organ transplant patients34,35,36. Moreover, M. triplex and M. mucogenicum be known as opportunistic infections in both immunocompromised and immunocompetent humans exposed to environmental sources and may be fatal if the infection is disseminated24,37,38. Accordingly, our study supports the evidence that a common indoor shower facility can be a potential source of NTM infection, which has clear relevance to public health.
In our study, the identified NTM isolates from resuspended samples and culture samples were different in several cases. There is a possibility that the specimen acquired each showerhead had a mixed microbial composition. In addition, some NTM might have hard nature to grow in cultivation. Thus, analysis of the resuspension sample and culture sample could be complementary.
The limitation of this study is that we did not consider some relevant factors, such as household water sources, estimated time since showerhead installation, usage frequency, and cleaning frequency, which may influence the ability of NTM to adhere and form a biofilm. Second, the number of acquired sample was small and most of isolated NTM were low pathogenicity species. The strength of this study is that we recovered the NTM from environmental samples by establishing methods of sample collection, processing, and cultivation.
In conclusion, our study showed the possible way of isolation and cultivation of NTM in showerhead biofilms. However, the species identified in the showerheads did not match those of the patients. Despite the identified NTM species in the showerheads, clinical implications in the main pathogenesis associated with the NTM-PD were not elucidated. Thus, further studies to explain the relationship between environmental exposure, infectious source and the route of NTM-PD are warranted.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Piersimoni, C. & Scarparo, C. Extrapulmonary infections associated with nontuberculous mycobacteria in immunocompetent persons. Emerg. Infect. Dis. 15, 1351 (2009).
Winthrop, K. L. et al. Incidence and prevalence of nontuberculous mycobacterial lung disease in a large US managed care health plan, 2008–2015. Ann. Am. Thorac. Soc. 17, 178–185 (2020).
Park, S. C. et al. Prevalence, incidence, and mortality of nontuberculous mycobacterial infection in Korea: A nationwide population-based study. BMC Pulm. Med. 19, 1–9 (2019).
Falkinham, J. O. III., Iseman, M. D., de Haas, P. & van Soolingen, D. Mycobacterium avium in a shower linked to pulmonary disease. J. Water Health 6, 209–213 (2008).
De Groote, M. A., Pace, N. R., Fulton, K. & Falkinham, J. O. Relationships between Mycobacterium isolates from patients with pulmonary mycobacterial infection and potting soils. Appl. Environ. Microbiol. 72, 7602–7606 (2006).
Falkinham, J. 3rd. Epidemiology of infection by nontuberculous mycobacteria. Clin. Microbiol. Rev. 9, 177 (1996).
Marras, T. K. & Daley, C. L. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin. Chest Med. 23, 553–568 (2002).
Kim, J. S. et al. Nontuberculous mycobacterial infection: CT scan findings, genotype, and treatment responsiveness. Chest 128, 3863–3869 (2005).
Castillo-Rodal, A. et al. Potentially pathogenic nontuberculous mycobacteria found in aquatic systems. Analysis from a reclaimed water and water distribution system in Mexico City. Eur. J. Clin. Microbiol. Infect. Dis. 31, 683–694 (2012).
Falkinham, J. O. Environmental sources of nontuberculous mycobacteria. Clin. Chest Med. 36, 35–41 (2015).
Embil, J. et al. Pulmonary illness associated with exposure to Mycobacterium-avium complex in hot tub water: Hypersensitivity pneumonitis or infection?. Chest 111, 813–816 (1997).
Falkinham, J. O. III. Nontuberculous mycobacteria from household plumbing of patients with nontuberculous mycobacteria disease. Emerg. Infect. Dis. 17, 419 (2011).
Nishiuchi, Y. et al. The recovery of Mycobacterium avium-intracellulare complex (MAC) from the residential bathrooms of patients with pulmonary MAC. Clin. Infect. Dis. 45, 347–351 (2007).
Thomson, R. et al. Isolation of nontuberculous mycobacteria (NTM) from household water and shower aerosols in patients with pulmonary disease caused by NTM. J. Clin. Microbiol. 51, 3006–3011 (2013).
Society, A. T. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175, 367–416 (2007).
Chen, P. et al. A highly efficient Ziehl-Neelsen stain: Identifying de novo intracellular Mycobacterium tuberculosis and improving detection of extracellular M. tuberculosis in cerebrospinal fluid. J. Clin. Microbiol. 50, 1166–1170 (2012).
Radomski, N. et al. Comparison of culture methods for isolation of nontuberculous mycobacteria from surface waters. Appl. Environ. Microbiol. 76, 3514–3520 (2010).
Wilson, K. Preparation of genomic DNA from bacteria. Curr. Protocols Mol. Biol. 56, 2.4.1-2.4.5 (2001).
Chae, H. et al. Development of a one-step multiplex PCR assay for differential detection of major Mycobacterium species. J. Clin. Microbiol. 55, 2736–2751 (2017).
Lee, H., Park, H.-J., Cho, S.-N., Bai, G.-H. & Kim, S.-J. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of therpoB gene. J. Clin. Microbiol. 38, 2966–2971 (2000).
Thomson, R. M. Changing epidemiology of pulmonary nontuberculous mycobacteria infections. Emerg. Infect. Dis. 16, 1576 (2010).
Cook, J. L. Nontuberculous mycobacteria: Opportunistic environmental pathogens for predisposed hosts. Br. Med. Bull. 96, 45–59 (2010).
Prevots, D. R., Adjemian, J., Fernandez, A. G., Knowles, M. R. & Olivier, K. N. Environmental risks for nontuberculous mycobacteria. Individual exposures and climatic factors in the cystic fibrosis population. Ann. Am. Thorac. Soc. 11, 1032–1038 (2014).
Covert, T. C., Rodgers, M. R., Reyes, A. L. & Stelma, G. N. Occurrence of nontuberculous mycobacteria in environmental samples. Appl. Environ. Microbiol. 65, 2492–2496 (1999).
Feazel, L. M. et al. Opportunistic pathogens enriched in showerhead biofilms. Proc. Natl. Acad. Sci. 106, 16393–16399 (2009).
Mullis, S. N. & Falkinham, J. III. Adherence and biofilm formation of Mycobacterium avium, Mycobacterium intracellulare and Mycobacterium abscessus to household plumbing materials. J. Appl. Microbiol. 115, 908–914 (2013).
Wolinsky, E. Nontuberculous mycobacteria and associated diseases. Am. Rev. Respir. Dis. 119, 107–159 (1979).
Olivier, K. N. et al. Nontuberculous mycobacteria: I: Multicenter prevalence study in cystic fibrosis. Am. J. Respir. Crit. Care Med. 167, 828–834 (2003).
Chan, E. D. et al. Alpha-1-antitrypsin (AAT) anomalies are associated with lung disease due to rapidly growing mycobacteria and AAT inhibits Mycobacterium abscessus infection of macrophages. Scand. J. Infect. Dis. 39, 690–696 (2007).
Falkinham, J. O. Impact of human activities on the ecology of nontuberculous mycobacteria. Future Microbiol. 5, 951–960 (2010).
Lee, E.-S., Lee, M.-Y., Han, S.-H. & Ka, J.-O. Occurrence and molecular differentiation of environmental mycobacteria in surface waters. J. Microbiol. Biotechnol. 18, 1207–1215 (2008).
Marshall, H. M. et al. Mycobacterium lentiflavum in drinking water supplies, Australia. Emerg. Infect. Dis. 17, 395 (2011).
Griffith, D. E. et al. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175, 367–416 (2007).
Weinberger, M., Berg, S. L., Feuerstein, I. M., Pizzo, P. A. & Witebsky, F. G. Disseminated infection with Mycobacterium gordonae: Report of a case and critical review of the literature. Clin. Infect. Dis. 14, 1229–1239 (1992).
Mazumder, S. A., Hicks, A. & Norwood, J. Mycobacterium gordonae pulmonary infection in an immunocompetent adult. N. Am. J. Med. Sci. 2, 205 (2010).
Choi, J. S. et al. A case of Mycobacterium gordonae pulmonary disease in a patient with ulcerative colitis treated with infliximab. Korean J. Med. 89, 452–456 (2015).
Shirata, M., Tamaru, A., Marumo, S. & Fukui, M. Mycobacterium triplex pulmonary disease in an immunocompetent host: A case report and literature review. IDCases 18, e00648 (2019).
Johnson, M. M. & Odell, J. A. Nontuberculous mycobacterial pulmonary infections. J. Thorac. Dis. 6, 210 (2014).
Author information
Authors and Affiliations
Contributions
C.J.Y. and S. B.R. designed the report and wrote the paper; P.Y.M., Y.S.H., and S.S.J. drafted and revised the manuscript; K.Y.A. designed the concept and finally approved the paper. All authors have taken due care to ensure the integrity of this work, and this final manuscript has been seen and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, J.Y., Sim, B.R., Park, Y. et al. Identification of nontuberculous mycobacteria isolated from household showerheads of patients with nontuberculous mycobacteria. Sci Rep 12, 8648 (2022). https://doi.org/10.1038/s41598-022-12703-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12703-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.