Abstract
Background
The Kilimanjaro Diabetic Programme used the Intervention Mapping framework to develop a theory- and evidence-based diabetic retinopathy screening programme. A Working Committee of health care workers and stakeholders ensured community engagement and empowerment of the target audience.
Objectives
To deliver a culturally appropriate, sustainable, community supported health intervention, promoting eye health behaviour change, to prevent avoidable blindness.
Methods
The six steps of the Intervention Mapping protocol incorporated eight components: (1) a needs assessment of people with diabetes and health care workers (2) a clinical trial of diabetic retinopathy screening modes, (3) comic strips as a motivational strategy for diabetic retinopathy screening uptake, (4) health care worker education (5) an electronic database of people with diabetes (6) a self-carry diary (7) implementation of mobile diabetic retinopathy retinal screening (8) process and outcome programme evaluation.
Results
The programme eliminated barriers to diabetic retinopathy screening in Kilimanjaro Christian Medical Centre eye and diabetic clinics, placing a digital retinal screening camera in the diabetic clinic and a fast-track screening system in the eye clinic. Two comic strips and a diary provided information about self-management and record of medications, treatment, blood sugar and blood pressure at clinic visits. An annual rural health care worker education programme met requests for knowledge on treatment and care of diabetes, targeting prevention of diabetic retinopathy. Rural digital retinal screening was implemented. Rural diabetes clinics were initiated.
Conclusions
Intervention Mapping provided a systematic, iterative model to formulate and deliver an urban and rural diabetic retinopathy screening programme.
Trial registration number
ISRCTN31439939. Details available at https://www.isrctn.com/
Similar content being viewed by others
Introduction
Diabetes in sub-Saharan Africa affects 21 million people and is expected to reach 31 million over the next two decades [1]. There are limited health resources, poor primary and secondary prevention of non-communicable diseases, undiagnosed diabetes estimated at 67%, and an aging population, despite the HIV/AIDs epidemic [1, 2].
Diabetic retinopathy (DR) is the most common microvascular complication of diabetes mellitus [3]. In developed countries poor glycaemic control, high blood pressure, and blood lipids levels have been linked to development and progression of DR [4]. If irreversible blindness is to be avoided, timely treatment with laser photocoagulation and intravitreal agents must be made available [5, 6]. Health systems of sub-Saharan Africa are overwhelmed by complex chronic diseases. Understanding of this pattern of multimorbidity is growing in low- and middle- income countries where public health expenditure is inadequate and insufficient to cover costs [7]. Few individuals can afford health insurance, making up the shortfall by paying out of pocket expenses, with devastating financial implications for the chronically ill [1, 2, 7].
Efforts to encourage people with diabetes (PWD) to adopt a healthy lifestyle including physical activity and eating a healthy diet are hindered by social norms in sub-Saharan Africa [8]. Collecting water and firewood, walking and cycling to and from work, and physical labour consume a significant amount of energy each day [8]. Many people suffer poverty, deprivation and hunger not comprehended outside of these communities [8]. In this context being overweight or even obese is seen as a sign of affluence [9, 10].
Education and health literacy go hand in hand. If patients have limited formal education, health care workers (HCW) face challenges in educating them about their disease conditions and motivating them to self-manage chronic diseases. Definitions, models and measuring tools for health literacy are continually being developed and refined [11]. Primarily the aim of health literacy is to ensure that individuals can access health information, and have the reading, writing and numeracy acumen necessary to complete self-management tasks required for self-care [11]. Presuming adult literacy is the basis for health literacy, then basic education is essential. PWD need to access written and verbal services from the health care system and information about their health and self-management [11].
Education of health care workers in sub-Saharan Africa is a serious challenge facing health provision and management of PWD with an undisputable mismatch between the volume of disease and the number of trained HCW [12]. Africa has 11 percent of the world’s population, carrying 24 percent of the global burden of disease, with less than 1 percent of global health expenditure and only 3 percent of the world’s health care workers; need and expenditure are grossly disproportionate [12].
Social cognitive theory was used as the guiding theory for understanding the health behaviours of the target population. A major component of social cognitive theory is observational learning which occurs through four processes: Attention, retention, production, and motivation. Firstly, an individual observes information from their environment, in real life or from a media source. Secondly, the individual remembers the information so that it can be recalled and reconstructed. Thirdly, in the production process, what has been learned can be applied in appropriated situations. This does not mean that the behaviour modelled will be exactly as observed but will be modified to fit the context of the individual’s situation. Finally, if the observed behaviour is rewarded it is more likely to be emulated than if the observed behaviour is punished. SCT suggests that individuals do not model every observationally learned behaviour [13].
Perceived self-efficacy refers to the individual’s capabilities to set goals and act to achieve planned behavioural outcomes [14]. Self-efficacy beliefs influence the course of action individuals take, the effort they exert in adopting health behaviours, their resilience when facing adversity, whether their thought patterns are self-hindering or self-helping, how much stress and depression they encounter from challenging environmental demands and the success they achieve [14]. Self-efficacy theory acknowledges the diversity of human capabilities [14]. Efficacy beliefs operate as a key factor in a generative system of human competence. For this reason, different individuals with similar skills or the same individual under different circumstance may perform badly, with competence or extraordinarily well, depending on variations in their beliefs in their personal efficacy [14].
At every level of the KDP health intervention programme the need to promote behavioural change through increasing self-esteem and modelling healthy behaviour were key change objectives, for both PWD and HCW.
Method
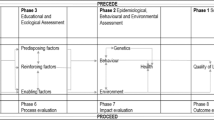
The KDP adopted the IM protocol to the DR screening programme in Kilimanjaro to prevent avoidable blindness [15]. Intervention Mapping (IM) is a robust theory and evidence-based protocol used in planning, developing, implementing, and evaluating behaviour change programmes [16]. IM is divided into six iterative step, sub-divided into tasks guiding ecological application to promote behaviour change for the target population, engaging and empowering the local community, in culturally, environmentally appropriate, sustainable, safe programme activities, free of discrimination [17,18,19]. Three perspectives characterize IM. (a) A social ecological approach in which health is viewed as a function of the environment where individuals live, work, and socialise. At each level ‘agents’ (decision makers or actors) can impact at individual (person living with diabetes), intrapersonal (ophthalmologists at Kilimanjaro Christian Medical Centre (KCMC) hospital), community (women’s groups) or societal (Ministry of Health) levels. Using the IM protocol programme planners focus on appropriate change agents within the levels of the system to achieve desired outcomes for the target population (PWD) [17]. (b) The second perspective is participation of stakeholders to ensure input from conception of the health intervention reflecting cultural, contextual, and environmental community concerns. This further ensures local knowledge, skills and expertise are used, empowering the community, giving them programme ownership, guaranteeing transparency and increasing the external validity of interventions and evaluation [17]. (c) The use of theory and evidence in IM enables the programme planner to look at relevant qualitative and quantitative research, consolidating information, reviewing theories, brain storming and comprising a working list of questions to begin Step 1 of the programme [16].
A broad outline of the IM steps and tasks used by the KDP are outlined in the Key Activities (Table 1).
Step 1. Logic model of the problem: A systematic literature review was undertaken on databases such as PubMed, Medline, Elsevier and Google Scholar to search for reviews and original studies world-wide and in low- and middle- income countries. It included intervention mapping, diabetic retinopathy screening, uptake of diabetic retinopathy screening, health literacy, health care worker education, diabetes, and mental health, for example.
Next the KDP Working Committee was established and met to discuss the week’s activities and plan ahead. From the outset local collaborative networks were established to enable the programme to develop and be responsive to the specific geographical, economic, and cultural context of the target population.
A qualitative needs assessment using a semi-structured interview was conducted with HCW and qualitative and quantitative needs assessment of PWD was conducted [18].
Analysis of the needs assessment produced the behavioural and environmental determinants of barriers to uptake of DR screening, the corresponding health problems and impact of quality of life on the PWD [18]. The findings of the needs assessment are summarised in the Logic model of the Problem. (Table 2).
Step 2. Programme outcomes and objectives: Logic Model of Change: The needs assessment identified what needed to change to achieve the desired behavioural outcomes. Performance objectives stated what the programme participants would do, or how the environment would be changed (including implementers) to achieve these objectives (The Logic Model of Change: Table 3) (Table 4 -Step 2: Behavioural outcomes and performance objectives.).
Step 3. Programme design: Based on social cognitive theory the KDP programme drew on modelling, framing, persuasive communication, goal setting and self-efficacy in the programme design. KDP PWD information, public community announcements, resources, and education materials, focused on observational learning and providing role models that would capacity build and empower both implementers and adopters. In collaboration with stakeholders the KDP Working Committee worked to develop culturally relevant strategies. (Supplementary files 1.1–1.4 Matrices of change objectives).
Step 4. Programme production: Stakeholders were kept informed of the KDP programme through newsletters and quarterly meetings. The diabetologist from KCMC hospital visited the rural HCF (Health Care Facilities) in his free time and encouraged the setting up of 14 specific diabetes clinics in Kilimanjaro Region.
Environment change methods focused on community involvement to ensure the KDP became a sustainable programme. Stakeholder meetings enabled the KDP Working Committee to interact with the community about the KDP programme, seek their opinions for implementation and provided feedback on how the programme was progressing, and the provision of training workshops.
Education was an important component of the KDP programme. Firstly, training to capacity build the facilitators who would educate rural HCW. Secondly, a one-day training at KCMC hospital to be followed by a rural education programme run annually, for three years, at different rural HCF in Kilimanjaro Region to educate HCW caring for PWD in these remote areas.
Provision of resources was necessary to support the HCW working at rural HCF, to meet the basic needs of PWD to monitor weight, blood pressure and blood glucose. Provision of reference books for each HCF as requested by HCW during the needs assessment. Educational comic strips and information leaflets on DR screening and treatment to motivate PWD for uptake of DR screening. Public awareness campaign posters to raise public awareness of KCMC hospital clinics and Direct Referral Site screening opportunities. KDP stickers for PWD to wear after DR screening to promote community awareness and dialogue about need for DR screening.
Follow-up and continuity of care through the KDP electronic database register PWD in Kilimanjaro: A CBM ophthalmologist created an electronic database, to enable KDP registration of PWD in Kilimanjaro. Demographic information, DR screening data, digital retinal images, and details of treatment are stored on the database to facilitate access for follow-up or treatment. Reminders to attend annual DR screening, follow-up appointments or treatment at KCMC hospital can be sent from the database via short message service.
A self-carry diary for PWD who registered with the KDP was produced, to take to clinic visits to document a personalised record of treatment and progress in self-management. The diary contains information about diet, exercise, foot and wound care, DR screening etc.
Methods and strategies to increase knowledge, social norms, self-efficacy and awareness access/availability: During the rural education programme, the facilitators modelled effective communication skills to the HCW. Goal setting strategies were taught, and HCW practised these skills before applying them in the clinical setting. The aim was to raise self-efficacy and motivate HCW to empower PWD to engage in self-management of diabetes.
Slogans were used to promote the message to PWD that ‘You can be Healthy Living with Diabetes’. The acronym KISS was used for the HCW,’ Keep it Simple Sasa’ (now), as there is a temptation among HCW to use technical language to impress patients with their knowledge rather than effectively communicate the information PWD need to know [18].
Methods to change social norms and health beliefs: Facilitators addressed the social norms affecting healthy eating, exercise and the use of traditional healers in the search for a cure for diabetes through evidence-based teaching, persuasive communication, modelling and goal setting. For example, social norms of cooking with fat, and not exercising are deeply imbedded in the culture of Tanzania, where obesity is seen as a sign of affluence [9, 10].
Methods to change awareness/access/availability: PWD were given comic strips (modelling uptake of DR screening) to read and take home. The comic strips provided information to explain the need for DR screening and act as a motivational strategy for uptake of DR screening.
After DR screening each recipient was given a KDP sticker to place on their blouse, shirt, or coat to promote community awareness and dialogue about the KDP and DR screening.
Establishing digital retinal screening in the diabetic and eye clinics at KCMC hospital and at rural direct referral sites (DRS) at HCF increased awareness, access, and availability of DR screening for PWD in Kilimanjaro region.
Environmental changes requiring change to improve access and availability of DR screening resulted in the provision of digital retinal screening in the diabetic and the fast track service in the eye clinics at KCMC hospital for PWD attending for DR screening. This significantly reduced waiting times for DR screening. Mobile digital retinal DR screening was introduced at rural DRS in Kilimanjaro Region, enabling opportunistic DR screening that did not rely on PWD travelling to KCMC hospital to attend for DR screening.
Step 5. Programme implementation plan: Adoption and implementation were addressed by including stakeholders from the start of the programme. HCW, PWD and, the annual rural education programme ensured that there was further ownership and integration of the DR screening programme.
Initially the KDP programme received specific funding for a three-year term from CBM and Australian Aid, which was increased, after monitoring and evaluation, for a further three years. It is now a sustainable programme; the eye department at KCMC continues to be funded by CBM. KCMC eye department is linked to Birmingham Eye Hospital through the VISION 2020 LINKSs Programme. The team gave advice at the outset of the KDP programme and provided the laptop computer and retinal camera to make digital retinal DR screening possible.
Step 6. Evaluation plan: The final step was developing and implementing evaluation plans for each component of the health intervention as they were conducted. Each aspect of the programme had process outcome and summation evaluations to ensure that the programme achieved its objectives. Monitoring and evaluation training were undertaking by the Working Committee and stakeholders as part of this process. The Monitoring and Evaluation training was run by an external educator so that process and outcome evaluation of the programme could be conducted by programme implementers and users and be a transparent process. Independent external evaluation was conducted by the programme funders.
Results
Step 1. Logic Model of Problem (Table 1): Needs assessment data on prevalence of DR in Kilimanjaro region n = 79 with 71/79 accepting DR screening. Visual impairment = 13.92%, Cataract = 5.06%, Severe visual impairment = 2.5%, DR 11.39% [18].
Eye Health Questionnaire: n = 79 56/79 knew DM damages the eyes. 55/79 not previously been screened for DR. Results of 5 psychometric measure, High levels of anxiety and depression, excessive burden of living with diabetes especially following diet regime, limited access to eye health care and treatment [18].
HCW interview findings: n = 31. 22/31 knew that diabetes damages the eye. 18/31 did not know that PWD need annual dilated annual eye exam. 21/31 did not know how DR could be treated [18].
Process Evaluation (Step 6: Pilot study indicated semi-structed interview and psychometric tools required some questions to be adapted. Findings of NA showed need to expand KDP screening programme to include comprehensive diabetes health education.)
Step 2. Programme outcomes and objectives: Logic Model of Change: (Table 2).
Step 5. Programme Implementation Programme:
-
1.
Drafts comic strip readability Flesch-Kincaid 75.7%, comprehension 87.4%. Soap opera comic strip readability Flesch-Kincaid 75.6%, comprehension 86.54%.
-
2.
Previous KCMC hospital trial improved DR screening from 29% to 47% with a nurse counsellor in diabetic clinic. [20] KDP CT n = 273 Diabetic Clinic n = 124 (91%) and Eye Clinic n = 122 (89%) (less exclusions).
-
3.
KDP self-carry diary for PWD who registered with KDP.
-
4.
Process evaluation was received by facilitators from HCW participating in the education programme. Feedback and course material were reviewed and updated to improve material and presentation.
-
5.
Education at HCF: examples of outcomes from second year of the three-year programme: HCW n = 59 demonstrated pre- and post- test improvement of knowledge with a two-tailed t test 17.27 df = 58, std error of difference =1.35, (p < 0.001). The mean difference was t = 23.39 (95% CI 20.68-26.10). Overall facilitator evaluation ratings were a mean of 87.5, SD 2.18 and overall satisfaction ratings were a mean of 90.0, SD 2.35.
-
6.
Year 2 post rural education programme, HCW n = 43 follow-up questionnaire, 33:43 HCW reported a positive change in clinical practice.
-
7.
Roll out of rural DR screening programme at DRS in Kilimanjaro Region. November 2010 and December 2014 DR screening n = 3187. The prevalence of any DR was 27.9% (95% CI 26.4–29.5%) [21].
-
8.
Reduced waiting times for PWD attending eye clinic at KCMC hospital due to fast track service.
Step 6. Evaluation:
-
1.
Process evaluation was conducted through each step of the programme. For example, in Step I, during the needs assessment, after the pilot project some questions were revised on the semi-structured interviews for the HCW and PWD, and on the quantitative questionnaires as they were not clearly understood [18].
-
2.
Analysis of the responses from HCW and PWD indicated not only the importance of health education but the need to expand this from eye health to include comprehensive treatment and management of diabetes.
-
3.
In Step 3 some of the initial artwork for the comic strip was considered culturally unacceptable by the KDP working committee and had to be revised.
-
4.
KDP programme was delivered to the intended recipients:
-
A.
PWD during clinical trial at KCMC hospital.
-
B.
PWD received comic strips during clinical trial and rural DR screening.
-
C.
HCW received education at rural HCF.
-
D.
Implementation of KDP register/database for recording for DR screening, demographic information, follow-up and treatment of PWD.
-
A.
-
5.
Adoption of DR screening at KCMC hospital and at DRS by PWD. PWD n = 203 153/203 did not attend for follow-up assessment or treatment after DR screening [22].
Discussion
At the start of the needs assessment, PWD were asked ‘What are the needs of PWD and understanding of eye health in Kilimanjaro Region?’ [18]. Innumerable challenges face PWD: socio-economic, cultural, and environmental. Health policies and funding are not adequate to cope with the needs of PWD in Kilimanjaro, as diabetes exists alongside increasing levels of multi-morbidity [23, 24].
The KDP was a small health intervention focusing on developing a comprehensive, integrated, theoretical and evidence-based screening programme to detected DR to prevent avoidable blindness. The IM framework provided an iterative framework to plan, develop, and implement the KDP programme with stakeholder participation. It included relevant change methods, appropriately and effectively applying them. The programme had a strong capacity building element and a sense of ownership among participants, securing funding to ensure viability of the programme in this low resource setting.
Strengths of the study
As has been reported the rural DR screening programme has been successful rolled out and collected data on the prevalence of DR in Kilimanjaro [21]. Data were collected on blood pressure, random blood sugar, duration of diabetes, Body Mass Index and visual acuity [21]. The study shows that the KDP achieved its initial objectives and its’ DR screening programme findings provide policymakers with data to assist in the planning of DR screening and treatment services in Kilimanjaro Region [21]. The study highlights the importance of managing comorbidities within DR screening programmes [21].
Weaknesses of the study
It is not clear that the outcome expectations of PWD were clearly communicated, understood or met [18, 21]. The aim of the KDP was to screen PWD while they were still asymptomatic, with no loss of visual acuity. PWD frequently did not attend for screening until they had some loss of vision [21]. A DR screening programme is only effective if PWD identified as having DR attend for follow-up and treatment. While the electronic database and Short Message Service recall system are useful tools, more needs to be done to ensure that at risk PWD are not lost once they are diagnosed with PDR and called for further follow-up or treatment [22].
For policy makers and politicians
Issues facing policy makers and politicians are linked to the funding of health care in sub-Saharan Africa. Adequate and appropriate education of health care workers is imperative, to enable medical management to focus on primary prevention of diabetes complications, including DR, within effective integrated diabetes services if avoidable blindness is to be prevented [4].
Conclusion
Researchers must seek further strategies for diabetes detection and management, tailoring models of care to the local geographical and social context. Health care education at all levels is a key component of care, along with appropriate cultural strategies for communicating health literature to PWD. It is important to conduct clinical trials in the sub-Saharan Africa context and focus on service development as complex challenges face health care provision in sub-Saharan Africa. Effective, theoretical, evidence-based interventions are urgently needed to relieve the burden of visual loss from DR in this region [4].
Intervention Mapping provided a powerful, evidence and theory-based health promotion platform on which to assess, plan, implement, promote, and evaluate the KDP programme. The steps of the model ensured that the programme was culturally and contextually grounded, engaging the target audience and stakeholders from the outset. The work of the KDP continues in Kilimanjaro, facing ongoing challenges and barriers to screening, follow-up, and treatment.
Summary
What is known about this topic
-
Intervention mapping is a robust, theory and evidence-based protocol used to develop, plan, implement, and evaluate health intervention programmes.
-
There was poor uptake of screening for diabetic retinopathy in rural Kilimanjaro region.
-
Kilimanjaro region is an area of low health literacy.
-
Access to eye health services is limited in rural Kilimanjaro region.
What this study adds
-
It demonstrates the development of a rural diabetic retinopathy screening program using the Intervention mapping protocol.
-
A culturally and contextually grounded health intervention, exemplifying engagement with the target audience and stakeholders from the outset.
-
The strategies and processes used to establish a rural diabetic retinopathy screening program where previously these services were either unavailable or difficult to access.
Change history
07 June 2022
The original online version of this article was revised to a Open Access.
References
Atun R, Gale EAM. The challenge of diabetes in sub-Saharan Africa. Lancet Diabetes Endocrinol. 2015;3:675–7.
Brown JB, Ramaiya K, Besançon S, Rheeder P, Tassou CM, Mbanya J-C, et al. Use of medical services and medicines attributable to diabetes in Sub-Saharan Africa. PloS ONE. 2014;9:e106716–e.
Sivaprasad S, Gupta B, Crosby-Nwaobi R, Evans J. Prevalence of diabetic retinopathy in various ethnic groups: a worldwide perspective. Surv Ophthalmol. 2012;57:347–70.
Burgess PI, Msukwa G, Beare NAV. Diabetic retinopathy in sub-Saharan Africa: meeting the challenges of an emerging epidemic. BMC Med. 2013;11:157.
DRS. Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of diabetic retinopathy study (DRS) findings, DRS report number 8. Ophthalmology. 1981;88:583–600.
ETDRS. Photocoagulation for diabetic macular edema: early treatment diabetic retinopathy study report number 1 early treatment diabetic retinopathy study research group. JAMA Ophthalmol. 1985;103:1796–806.
Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of noncommunicable disease multimorbidity on healthcare utilisation and out-of-pocket expenditures in middle-income countries: cross sectional analysis. PLOS ONE. 2015;10:e0127199.
Mbalilaki JA, Masesa Z, Strømme SB, Høstmark AT, Sundquist J, Wändell P, et al. Daily energy expenditure and cardiovascular risk in Masai, rural and urban Bantu Tanzanians. Br J Sports Med. 2010;44:121.
Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–66.
Brewis AA, Wutich A, Falletta-Cowden A, Rodriguez-Soto I. Body Norms and Fat Stigma in Global Perspective. Curr Anthropol. 2011;52:269–76.
Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promotion Int. 2017;33:901–11.
International Finance Corporation. Health and Education in Africa (2018). 2018.
Bandura A. Self-efficay mechanism in human agency. Am Psychologist. 1982;37:122–47.
Bandura A Self-Efficacy. The Exercise of Control. 1st ed. New York: W.H. Freeman and Company; 1997. 1-604 p.
Bartholomew LK, Parcel, GS, Kok, G, Gottlieb, NH, Fernandez, ME Planning Health Programs, An Intervention Mapping Approach. Planning Health Programs, An Intervention Mapping Approach. 1. 3rd ed. San Franciso, CA: Jossey-Bass, A Wiley Imprint; 2011. p. 745.
Bartholomew KL, Parcel, GS, Kok, G, Gottlieb, NH Planning Health Promotion Programs: An Intervention Mapping Approach. Second Edition ed. United States of America: Jossey-Bass; 2011 January 2011. 800 p.
Kok G, Peters LWH, Ruiter RAC. Planning theory- and evidence-based behavior change interventions: a conceptual review of the intervention mapping protocol. Psicologia: Reflexão e Crítica. 2017;30:19.
Hall CE, Hall AB, Kok G, Mallya J, Courtright P. A needs assessment of people living with diabetes and diabetic retinopathy. BMC Res Notes. 2016;9:56.
Olapade-Olaopa EO, Sewankambo NK, Iputo JE. Defining sub-saharan africa’s health workforce needs: going forwards quickly into the past comment on “non-physician clinicians in Sub-Saharan Africa and the evolving role of physicians”. Int J Health Policy Manag. 2016;6:111–3.
Mumba M, Hall A, Lewallen S Compliance with eye screening examinations among diabetic patients at a Tanzanian referral hospital. Ophthalmic Epidemiol. 2007.
Cleland CR, Burton MJ, Hall C, Hall A, Courtright P, Makupa WU, et al. Diabetic retinopathy screening: experiences from northern Tanzania. Lancet Diabetes Endocrinol. 2016;4:10–2.
Mtuya C, Cleland CR, Philippin H, Paulo K, Njau B, Makupa WU, et al. Reasons for poor follow-up of diabetic retinopathy patients after screening in Tanzania: a cross-sectional study. BMC Ophthalmol. 2016;16:115.
Alaba F, Chola L. The social determinants of multimorbidity in South Africa. Int J Equity health. 2013;12:63.
Harper K, Armelagos G. The changing disease-scape in the third epidemiological transition. Int J Environ Res Public Health. 2010;7:675–97.
Acknowledgements
We acknowledge the tremendous work of the staff at the Kilimanjaro Christian Medical Centre, Tumaini University and in the regional health care facilities. We acknowledge the support of the VISION 2020 LINKS Programme and the Ophthalmologists at Birmingham Hospital for their kindness and support of our program.
Funding
CBM (Christian Blind Mission) and AusAid provided the funding for the KDP. Grant number P0393 The publication costs for this article were funded by The Queen Elizabeth Diamond Jubilee Trust through the Commonwealth Eye Health Consortium. The funding body did not participate in the design of the study, data collection and analysis, interpretation of data and writing the manuscript
Author information
Authors and Affiliations
Contributions
CH contributed to the concept, design and implementation of the Kilimanjaro Diabetic Project, lead the research, analysed the data and wrote the manuscript. AH contributed to the concept, design and implementation of the Kilimanjaro Diabetic Project, corrections and comments on the draft and the final revision. JM contributed to the concept and design of the Kilimanjaro Diabetic Project, interviewed subjects, collected data, and translated interviews PC contributed to the concept and design of the Kilimanjaro Diabetic Project, helped with data analysis and comments on the draft. GK revised and edited the manuscript All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was granted by Kilimanjaro Christian Medical Centre Ethics Committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have permission under this license to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hall, C.E., Hall, A.B., Mallya, J. et al. Establishing a screening programme for diabetic retinopathy in Kilimanjaro Region, Tanzania using intervention mapping. Eye 36 (Suppl 1), 17–24 (2022). https://doi.org/10.1038/s41433-022-02001-w
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02001-w
This article is cited by
-
Present and future screening programs for diabetic retinopathy: a narrative review
International Journal of Retina and Vitreous (2024)