Abstract
There is growing evidence that suggests a potential association between particulate matter (PM) and suicide. However, it is unclear that PM exposure and suicide death among major depressive disorder (MDD) patients, a high-risk group for suicide. We aimed to assess the effect of short-term exposure to PM on the risk of suicide in MDD patients who are at high risk for suicide. We investigated the risk of suicide among 922,062 newly-diagnosed MDD patients from 2004 to 2017 within the Korean National Health Insurance Service (NHIS) database. We identified 3,051 suicide cases from January 1, 2015, to December 31, 2017, within the death statistics database of the Korean National Statistical Office. PMs with aerodynamic diameter less than 2.5 μm (PM2.5), less than 10 μm (PM10), and 2.5–10 μm (PM2.5–10) were considered, which were provided from the National Ambient Air Monitoring System in South Korea. Time-stratified case-crossover analysis was performed to investigate the association of particulate matter exposure to suicide events. The risk of suicide was significantly high upon the high level of exposure to PM2.5, PM2.5–10 (coarse particle) and PM10 on lag 1 (p for trend < 0.05). Short-term exposure to a high level of PM was associated with an elevated risk for suicide among MDD patients. There is a clear dose–response relationship between short-term PM exposures with suicide death among MDD patients. This result will be used as an essential basis for consideration when establishing an air pollution alarm system for reducing adverse health outcomes by PM.
Similar content being viewed by others
Introduction
There has been a significant increase in suicide cases in recent decades, posing a severe public health problem worldwide1,2. Globally, it is the second leading cause of death among young adults and approximately 800,000 people suicide every year1. Various social and environmental factors affect suicide, including culture, gender, age, socioeconomic status3,4. The risk of suicide is even higher with underlying disease (i.e., HIV, cancer)5,6, especially with a psychiatric disorder2,3,7. A previous study has noted that patients with depression or other mood disorders have a 20-fold increased suicide risk compared to the general population. Meanwhile, depression is becoming increasingly burdensome, and the number of incident cases of depression worldwide increased from 172 million in 1990 to 258 million in 2017, representing an increase of 49.9%8. Considering this trend, identifying and managing risk factors affecting suicide in major depressive disorder (MDD) patients is crucial.
Previous studies have shown that long-term exposure to particulate matter (PM) might increase the risk of depression through chronic inflammation and brain structure changes9,10. Additional studies were done to evaluated the effect of short-term exposure to PM and noted that it aggravates several psychiatric symptoms, including suicide attempts, increases emergency center visits, and hospitalization11,12. Based on these findings, recent studies have investigated the association of short-term exposure to PM with suicide and reported an elevated risk for suicide in the general population13,14,15,16.
However, this association of PM short-term exposure and suicide has not been explored in the depressive population. Since MDD patients are at high risk for suicide and vulnerable to short-term mood swings that PM might aggravate, a further investigation among MDD patients is merited. Therefore, we aimed to assess the effect of short-term exposure to PM on the risk of suicide in newly diagnosed MDD patients in Korea, using the National Health Insurance Service (NHIS) database.
Methods
Study population
The study population was derived from the Korean NHIS database. The NHIS is a single-payer of the Korean healthcare system and provides universal health insurance for 97% of Korean citizens17. The NHIS collects all forms of claimed healthcare service data, which includes outpatient visits, hospital admissions, emergency department usages, and pharmaceutic drug prescriptions. The NHIS provides collected data for research purposes, and multiple epidemiologic studies using this data have demonstrated its validity18.
We enrolled 922,062 newly-diagnosed major depressive disorder (MDD) patients above 20 years old from the NHIS database who was diagnosed between January 1, 2004, to December 31, 2017. The diagnosis of MDD was defined with diagnosis codes of MDD (F32, F33) from the International Classification of Diseases, Tenth Revision (ICD‐10) and the use of anti-depressant medication at least once during the study period. Participants who were diagnosed with bipolar disease (ICD-10 code F31) and schizophrenia(ICD-10 code F20) were also excluded, because patient with both disease are often first diagnosed as depression, but they have different characteristics from patients with MDD. We followed the study participants from their initial diagnosis date of MDD until December 31, 2017.
Among 922,062 newly-diagnosed MDD patients, we identified 3085 suicide cases after January 1, 2015. Suicide events before January 1, 2015 were excluded in the main analysis due to the lack of PM2.5 data before 2015. The suicide events were defined by death due to intentional self-harm (ICD-10 codes X60–X84). 34 suicide cases were excluded from the analysis due to missing value for PM2.5 data and average daily temperature. Total 3051 suicide cases were included in the main analysis.
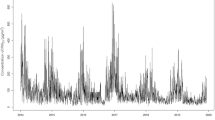
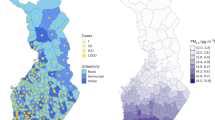
Particulate matter exposure
The NHIS database also provides demographic information of the participants, which include the residential district code. Using the code, we have linked the residential district to the daily ambient level of PM10 and PM2.5, provided by the National Ambient Air Monitoring System in South Korea. There are approximately 300 atmospheric monitoring stations in Korea and these sites are selected according to certain criteria, such as the number of residents, location, emission source, and representative are of the target site. There was no district with more than two monitoring stations. All residential districts but two were covered by atmospheric monitoring stations, which covers 1.4% of the total population. Particulate matter levels in unmonitored sites were estimated by using the closest monitoring station19. The concentration of the coarse particle was calculated by subtraction of the PM2.5 value from that of PM10.
Statistical analysis
We used a time-stratified case-crossover analysis study design to investigate the association of particulate matter exposure with suicide events. The case-crossover study is a validated study design to assess the short-term effect of the exposure. Each patient serves as his or her own control, thereby time-invariant individual variables such as age, sex, and individual comorbidities, are automatically controlled. Among several case-crossover designs, the time-stratified case-crossover design yielded better results with the least bias on previous systemic reviews20,21. We used single-day lag models to investigate the effect of PM exposure on suicide from lag0 (the day of the suicide event) to lag3 (3 days prior to the suicide event). Also, we used a 4-day cumulative lag model (lag0–3) to assess the effect of short-term cumulative PM exposure on suicidality. This is based on the results from the previous study, which noted that evidence of associations suggested short exposure periods lasting up to an average of 0–3 days16. The control days were matched by other days with the same day of the week from the same calendar month, and the same calendar year. The PM value of each case day (lag0 to lag3 and lag0–3) and control days were divided into approximate quartile. The conditional logistic regression was used to estimate the adjusted odds ratios (aORs) and 95% confidence intervals (CIs) of each quartile compared to the 1st quartile of the PM10, PM2.5, and coarse particles exposure, which represented the least exposure to the PM. An indicator variable for national holidays, an indicator variable for weekends, rainfall, and temperature were included as covariates. Stratified analysis according to subgroups of age, sex, household income, and duration of MDD, stratified analysis was conducted to examine the effect modification. According to the individual's physical activity and alcohol consumption, an additional stratified analysis was conducted on 1606 suicide cases among MDD patients who underwent health examinations within 2 years before the suicide event. All statistical tests were two-sided manner with a p value of less than 0.05. Data collection and statistical analyses were performed using SAS Enterprise Guide 7.1 (SAS Institute Inc., Cary, NC).
Ethical consideration
This study was conducted in accordance with the Declaration of Helsinki and the study protocol approved by the Institutional Review Board (IRB) at the National Center for Mental Health, Seoul, Korea (IRB number: 116271-1027-57). The requirement for informed consent was waived by IRB at National Center for Mental Health since the patient information was de-identified and anonymized according to South Korean personal data protection laws.
Results
The descriptive characteristics of the study population are depicted in Table 1 by chi-square test and analysis of variance test. Among 3051 suicide cases we have enrolled, 765, 767 759 and 760 cases were allocated for the first, second, third, and fourth quartile of lag0 PM10 exposure respectively. The mean PM10 values of the suicide day on each quartile were 23.6, 36.6, 48.9, and 78.7 μg/m3, respectively. Participants exposed to the higher concentration of PM10 on the day of suicide (lag0) were more likely to be exposed to high PM2.5 and coarse particle concentration. However, the distribution of age, gender, household income, disease duration, alcohol consumption and physical activity were not significantly different by quartiles of PM10 exposure.
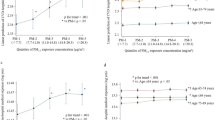
Table 2 shows the association between PM10 exposure and completed suicide events among MDD patients. Compared to those exposed to the lowest concentration of PM10 on lag1 (a day before the suicide event), those exposed to the highest concentration of PM10 on lag1 had higher odds of completed suicide (aOR 1.19, 95% CI 1.03–1.36). Furthermore, the risk of suicide increased upon the higher exposure to PM10 on lag1 (p for trend = 0.017).
The association of PM2.5 exposure and suicide events on MDD patients is demonstrated in Table 3. Patients exposed to the highest level of PM2.5 on lag1 was associated with higher odds of suicide (aOR 1.17, 95% CI 1.03–1.34) compared to those exposed to the lowest concentration of PM2.5 on lag 1. The dose-responsive association of PM2.5 exposure and suicide was also statistically significant (p for trend 0.021).
The association of coarse particle exposure and suicide events is depicted in Table 4. There were statistically significant dose-responsive associations of completed suicide with coarse particle exposure on lag1 (p for trend 0.017). MDD patients who were exposed to the highest concentration of coarse particles on lag1 (4th quartile) had higher odds for suicide (aOR 1.19, 95% CI 1.03–1.38), compared to those who were exposed to the lowest concentration of coarse particle (1st Quartile).
Table 5 shows the results of the stratified analysis on the association of PM exposure and suicidal events. The risk elevating effect of PM was prominent among MDD patients aged 40 years or older, women, within 5 years of MDD diagnosis, who do not exercise. Although the statistical significance tended to be attenuated most likely due to the reduce number of cases upon stratification, exposure to high concentration of PM on lag1 and had tendency to increase the risk for suicide among MDD patients in multiple subgroups.
Supplementary Table 1 shows the suicide risk per interquartile range (IQR) increase in PM10, PM2.5, and coarse particle based on linear modeling of PM with suicide. There was a significant increased risk for suicide upon IQR increase in PM10 (aOR 1.05, 95% CI 1.01–1.10), and coarse particle (aOR 1.04, 95% CI 1.01–1.07) on lag1, but not in PM2.5.
Discussion
In this study of 3051 suicide cases from 922,062 newly diagnosed MDD patients in South Korea, we found that short-term exposure to a high PM level was associated with increased suicide risk. The higher the concentration of PM (lag1) was, the higher the risk for completed suicide MDD patients had (p for trend < 0.05), confirming a dose-responsive relationship between PM level and risk of completed suicide. To our knowledge, this is the first and largest epidemiological study to assess suicide risk among MDD patients to PM exposure. We found a significant association between suicide risk and PM.
A recent study on 134,811 suicide cases in 10 cities in northeast Asia reported significantly increased suicidal risk upon the increased level of PM10 and coarse particles at lag 0–1 but not with PM2.516. Similar findings were noted in multiple previous studies among the general population, although the results were slightly different from13,14. A study on 4341 suicide cases in 2004 in South Korea reported a significantly increased suicidal risk upon the increased level of both PM 10 at lag 0–2 and PM 2.5 at lag 113, while another study on 1546 suicide cases from 2001 to 2010 in Utah USA reported an increased suicide risk associated with PM 2.5 levels at lag 2 but not with PM1014. Our study shows similar results with these studies, supporting increased suicidal risk upon the increased level of the PM, and further expands the concept to depression patients at high risk for suicide. Also, there was a dose-responsive elevated risk for suicide upon PM exposure in our study, showing an 19%, 17% and 19% increase risk for suicide among participants exposed to the highest level of PM10, PM2.5, and coarse particles respectively, compared to the least exposed group. Previous studies on the general population used a different measure of exposure such as an increase in interquartile range13,14,15,16. These studies reported 2–9% increased risk for suicide per interquartile range increase of PM level. Direct comparison of the strength of association is difficult with previous studies, however the result from our study was similar to the previous studies in general population.
PM exposure was associated with an increase in suicide, and various mechanisms have been suggested to explain this association, with the etiology of depression. The significant effects of PM are explained through low-grade systemic inflammation originating in peripheral tissues such as the lung and skin. Systemic-induced cytokines circulate the body and possibly causing neuroinflammation, neuronal damage, and neurotransmitter change. Since smaller particles enter the systemic circulation and invade the brain parenchyma more easily, PM2.5 and ultrafine PM (diameter < 0.1 μm) are usually considered as the leading cause of inflammatory damage from the PM9. Moreover coarse particles are known to cause more inflammatory reactions in an acute exposure22,23, sometimes immediate and excessive inflammatory reactions such as allergic reactions24. Beside chemical components on coarse PM enter through the olfactory mucosa and bulb affect the brain rapidly and directly, coarse particles might also be a major cause of short-term neuroinflammatory. This exacerbation of neuroinflammation by PM may aggravate the depressive symptoms and stimulate the hyperactivated hypothalamic–pituitary–adrenal axis, which might cause mood instability and future suicide risk.
Moreover, PM can affect mood swings and inadequate control of impulsivity in another way. Previous studies reported that PM could cause circadian rhythm disturbance by reducing sunlight or solar radiation and also affects mood swings25,26. This association can be explained by decreased serotonin activity. Serotonin is a crucial neurotransmitter in stabilizing mood and regulating aggression and impulsivity27 and is produced according to sunlight exposure. Since PM decreases sunlight exposure, it might reduce serotonin level and possibly cause aggressiveness or uncontrolled impulsivity, directly linked to completed suicide. Particularly serotonin's rapid turnover is especially crucial in the pathophysiology of MDD, so the impact due to serotonin reduction would be critical for MDD patients.
Increasing suicide risk on PM exposure can be understood with the stress–diathesis model. The stress–diathesis model is one of the explanatory and predictive models of suicidal behavior28. It is hypothesized that individuals with a diathesis (predisposes vulnerability to the stressor) will lead to suicidal behaviors when confronted with stressors. Acute psychiatric disease aggravation or psychosocial crises are a common stressor. Various factors such as sex, religion, genetic factor, childhood experiences, familial factors, and cholesterol levels influence the diathesis28. Higher PM is associated with increasing suicide by exacerbating the disease13, and PM is proposed as a novel environmental trigger of suicide29. Once depressive patients who already have a hypersensitive hypothalamic–pituitary–adrenal axis, which induces mood instability and impulsivity, are triggered by stressors such as PM can develop suicidal behavior readily.
In our study, a high PM concentration increased the risk of suicide among MDD patients in multiple subgroups. Although statistical significance declined due to the decrease in the number of samples, we need to consider that this result may be reflecting the subgroup characteristics of depressed patients who are sensitive to PM exposure. Participants aged 40 years or older, women, within 5 years of MDD diagnosis and who do not exercise were particularly susceptible to PM exposure (Table 5). Consistent with previous findings13, we found a strong association among participants aged over 40 years. It is probably because the middle age group (35–64 years old) is exposed to higher PM more often during commuting or other activity, and also elderly people are sensitive to PM exposure30. Women were strong associated with PM exposure in our study. This result is also similar to the previous study31, explained by estrogen’s proinflammatory effect while androgen has immunosuppressive when exposed PM32. Exercise and physical activity have beneficial effects as antidepressant33, lowers suicidal ideation34, which explains why people who do not exercise was sensitive to PM exposure on our study. Finally, the risk of suicide is highest within 90 days of diagnosis of depression depression (aOR 7.33, 95% CI 4.76–11.3)35 or the first 90 days after hospital discharge36. Moreover regardless of the severity or duration, patient with MDD has highest risk of suicide within 5 years of the diagnosis37, which explains the result of our study. The synergistic effect of predisposing factors of suicide and PM on mood swings could explain these results.
Our study has several limitations. First, suicide cases might have been underreported because it can be recorded as accidental or undetermined. Second, the participants' residence area might be different from the actual place where the participants spend most of the time, such as the workplace or school. The level of exposure to PM might not be accurately calculated in such cases. Further studies with a more accurate measure of an individual's exposure to PM will be needed. Third, the possible confounder, daylight hours, were not considered in the analysis. On the other hand, daylight hours vary over a seasonal time frame. Therefore, daylight hours of control dates within a few weeks from the case dates would not vary from the case daylight hours. Additionally, we tried to take account of meteorological effects including temperature and precipitation, which indirectly reflect the sunlights hours besides seasonal variation. Fourth, other underlying diseases that could be affected the risk for suicide were not considered. Although, we used a time-stratified case-crossover design, in which each participant serves as their control. However, it is estimated that exacerbation of underlying disease caused by PM exposure increases the risk of suicide, so it is necessary to investigate disease groups that are particularly sensitive to PM exposure. Fifth, the severity of the disease among MDD participants was not reflected. Drug compliance and symptoms of depression at the time of suicide were not accounted for. Therefore, further studies considering the severity of psychiatric symptoms and treatment regimen will be merited. Finally, the suicide date in our study was based on death registry data, so it is possible directly reflect the suicide attempted date. For example, if a participant has attempted suicide but died in the hospital a couple of days later, the recorded suicide date would be later than the exposure day. However, the 4-day cumulative lag model takes account for this possibility and suggests that short-term exposure to the high level of PM in MDD patients increases the risk for suicide.
Despite these limitations, this study was the first large-scale study investigating PM's effects on suicide among MDD patients. Conjunction with the etiology of depression, we tried to elucidate the effects of PM exposure on suicide in depressed patients.
Conclusion
Short-term exposure to PM was associated with increased risk of suicide in pre-existing depressed patients. The evidence supporting the mechanism of PM on depression and mood swings were not enough. However, this result suggests that awareness of harm for PM is needed for public mental health, emphasizes the importance of establishing an air pollution alarm system. Further researches on PM's neurophysiological responses are needed to understand the potential mechanism of PM's impact on suicide.
References
Suicide, http://www.who.int/mental_health/suicide-prevention/en (2019).
Turecki, G. et al. Suicide and suicide risk. Nat. Rev. Dis. Primers. 5, 1–22 (2019).
Bachmann, S. Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public Health. https://doi.org/10.3390/ijerph15071425 (2018).
Qin, P., Agerbo, E. & Mortensen, P. B. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: A national register–based study of all suicides in Denmark, 1981–1997. Am. J. Psychiatry 160, 765–772 (2003).
Schlebusch, L. & Govender, R. Elevated risk of suicidal ideation in HIV-positive persons. Depress. Res. Treat. 2015, 1–6 (2015).
Lee, S. J. et al. Depression and suicide ideas of cancer patients and influencing factors in South Korea. Asian Pac. J. Cancer Prev. 15, 2945–2950 (2014).
Ösby, U., Brandt, L., Correia, N., Ekbom, A. & Sparén, P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch. Gen. Psychiatry 58, 844–850 (2001).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr. Res. 126, 134–140 (2020).
Block, M. L. & Calderón-Garcidueñas, L. J. T. I. N. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 32, 506–516 (2009).
Calderón-Garcidueñas, L. et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid β-42 and α-synuclein in children and young adults. Toxicol. Pathol. 36, 289–310 (2008).
Cho, J. et al. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. J. Affect. Disord. 157, 45–51 (2014).
Szyszkowicz, M., Willey, J. B., Grafstein, E., Rowe, B. H. & Colman, I. Air pollution and emergency department visits for suicide attempts in Vancouver, Canada. Environ. Health Insights 4, EHI S5662 (2010).
Kim, C. et al. Ambient particulate matter as a risk factor for suicide. Am. J. Psychiatry 167, 1100–1107 (2010).
Bakian, A. V. et al. Acute air pollution exposure and risk of suicide completion. Am. J. Epidemiol. 181, 295–303 (2015).
Lee, H. et al. Association between dust storm occurrence and risk of suicide: Case-crossover analysis of the Korean national death database. Environ. Int. 133, 105146. https://doi.org/10.1016/j.envint.2019.105146 (2019).
Kim, Y. et al. Air pollution and suicide in 10 cities in Northeast Asia: A time-stratified case-crossover analysis. Environ. Health Perspect. 126, 037002. https://doi.org/10.1289/ehp2223 (2018).
Cheol Seong, S. et al. Data resource profile: The National Health Information database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 46, 799–800. https://doi.org/10.1093/ije/dyw253 (2017).
Son, J. S. et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association Guidelines with subsequent cardiovascular disease events. JAMA 320, 1783–1792. https://doi.org/10.1001/jama.2018.16501 (2018).
Kim, S. R. et al. Association of combined effects of physical activity and air pollution with diabetes in older adults. Environ. Int. 145, 106161 (2020).
Carracedo-Martinez, E., Taracido, M., Tobias, A., Saez, M. & Figueiras, A. Case-crossover analysis of air pollution health effects: A systematic review of methodology and application. Environ. Health Perspect. 118, 1173–1182. https://doi.org/10.1289/ehp.0901485 (2010).
Janes, H., Sheppard, L. & Lumley, T. Case-crossover analyses of air pollution exposure data: Referent selection strategies and their implications for bias. Epidemiology 16, 717–726. https://doi.org/10.1097/01.ede.0000181315.18836.9d (2005).
Pozzi, R., De Berardis, B., Paoletti, L. & Guastadisegni, C. Inflammatory mediators induced by coarse (PM2.5–10) and fine (PM2.5) urban air particles in RAW 264.7 cells. Toxicology 183, 243–254 (2003).
Becker, S., Soukup, J. M., Sioutas, C. & Cassee, F. R. Response of human alveolar macrophages to ultrafine, fine, and coarse urban air pollution particles. Exp. Lung Res. 29, 29–44 (2003).
Phalen, R. F. J. N. I. B. The particulate air pollution controversy. Nonlinearity Biol. Toxicol. Med. 2, 15401420490900244 (2004).
Luo, H., Han, Y., Lu, C., Yang, J. & Wu, Y. Characteristics of surface solar radiation under different air pollution conditions over Nanjing, China: Observation and simulation. Adv. Atmos. Sci. 36, 1047–1059. https://doi.org/10.1007/s00376-019-9010-4 (2019).
Wang, Y. et al. Ambient fine particulate matter exposure perturbed circadian rhythm and oscillations of lipid metabolism in adipose tissues. Chemosphere 251, 126392 (2020).
Bourgeois, M. Serotonin, impulsivity and suicide. Hum. Psychopharmacol. Clin. Exp. 6, S31–S36 (1991).
Mann, J. J., Waternaux, C., Haas, G. L. & Malone, K. M. Toward a clinical model of suicidal behavior in psychiatric patients. Am. J. Psychiatry 156, 181–189 (1999).
Casas, L. et al. Does air pollution trigger suicide? A case-crossover analysis of suicide deaths over the life span. Eur. J. Epidemiol. 32, 973–981 (2017).
Sacks, J. D. et al. Particulate matter-induced health effects: Who is susceptible?. Environ. Health Perspect. 119, 446–454 (2011).
Stickley, A., Ng, C. F. S., Konishi, S., Koyanagi, A. & Watanabe, C. Airborne pollen and suicide mortality in Tokyo, 2001–2011. Environ. Res. 155, 134–140 (2017).
Chen, W., Mempel, M., Schober, W., Behrendt, H. & Ring, J. Gender difference, sex hormones, and immediate type hypersensitivity reactions. Allergy 63, 1418–1427 (2008).
Dinas, P., Koutedakis, Y. & Flouris, A. Effects of exercise and physical activity on depression. Ir. J. Med. Sci. 180, 319–325 (2011).
Vancampfort, D. et al. Physical activity and suicidal ideation: A systematic review and meta-analysis. J. Affect. Disord. 225, 438–448. https://doi.org/10.1016/j.jad.2017.08.070 (2018).
Randall, J. R. et al. Acute risk of suicide and suicide attempts associated with recent diagnosis of mental disorders: A population-based, propensity score—matched analysis. Can. J. Psychiatry 59, 531–538 (2014).
Olfson, M. et al. Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiat. 73, 1119–1126 (2016).
Malone, K. M., Haas, G. L., Sweeney, J. A. & Mann, J. J. Major depression and the risk of attempted suicide. J. Affect. Disord. 34, 173–185. https://doi.org/10.1016/0165-0327(95)00015-F (1995).
Funding
This research was supported by the National Health Insurance Service of Korea. The National Health Insurance Service of Korea had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript, and decision to submit for publication.
Author information
Authors and Affiliations
Contributions
S.M.P. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: D.C., S.C., J.C., S.M.P. Acquisition of data: A.J.G. Analysis and interpretation of data: all authors. Drafting of the manuscript: I.Y.H., D.C., J.A.K. Critical revision of the manuscript: all authors. Statistical analysis: D.C., J.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hwang, I.Y., Choi, D., Kim, J.A. et al. Association of short-term particulate matter exposure with suicide death among major depressive disorder patients: a time-stratified case-crossover analysis. Sci Rep 12, 8471 (2022). https://doi.org/10.1038/s41598-022-12421-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12421-z
This article is cited by
-
The short-term effect of ambient particulate matter on suicide death
Environmental Health (2024)
-
Short-term exposure to PM2.5 and 1.5 million deaths: a time-stratified case-crossover analysis in the Mexico City Metropolitan Area
Environmental Health (2023)
-
Ecological correlation between short term exposure to particulate matter and hospitalization for mental disorders in Shijiazhuang, China
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.