When Johnson & Johnson released its single-dose COVID-19 vaccine in early 2021, the company touted it as a “critical tool for fighting this pandemic.”
It could be stored at standard refrigeration temperatures and shipped widely, which would be beneficial for rural areas and developing countries. And while it was slightly less effective than the Moderna and Pfizer-BioNTech mRNA vaccines, it still provided strong protection against severe disease and hospitalization.
But since then, the vaccine has met some challenges. Its distribution was paused after a small number of people developed a blood clotting disorder after receiving the shot; it was resumed shortly after.
With the omicron variant of COVID-19 now dominant across Colorado, health care experts recommend all eligible people get vaccinated, and receive a booster in order to be fully protected.
But what does that mean for the more than 300,0000 people in the state who received the Johnson & Johnson shot? Are they as protected as those who received doses of the mRNA vaccines? If they get a booster, should they get the same shot or can they mix and match?
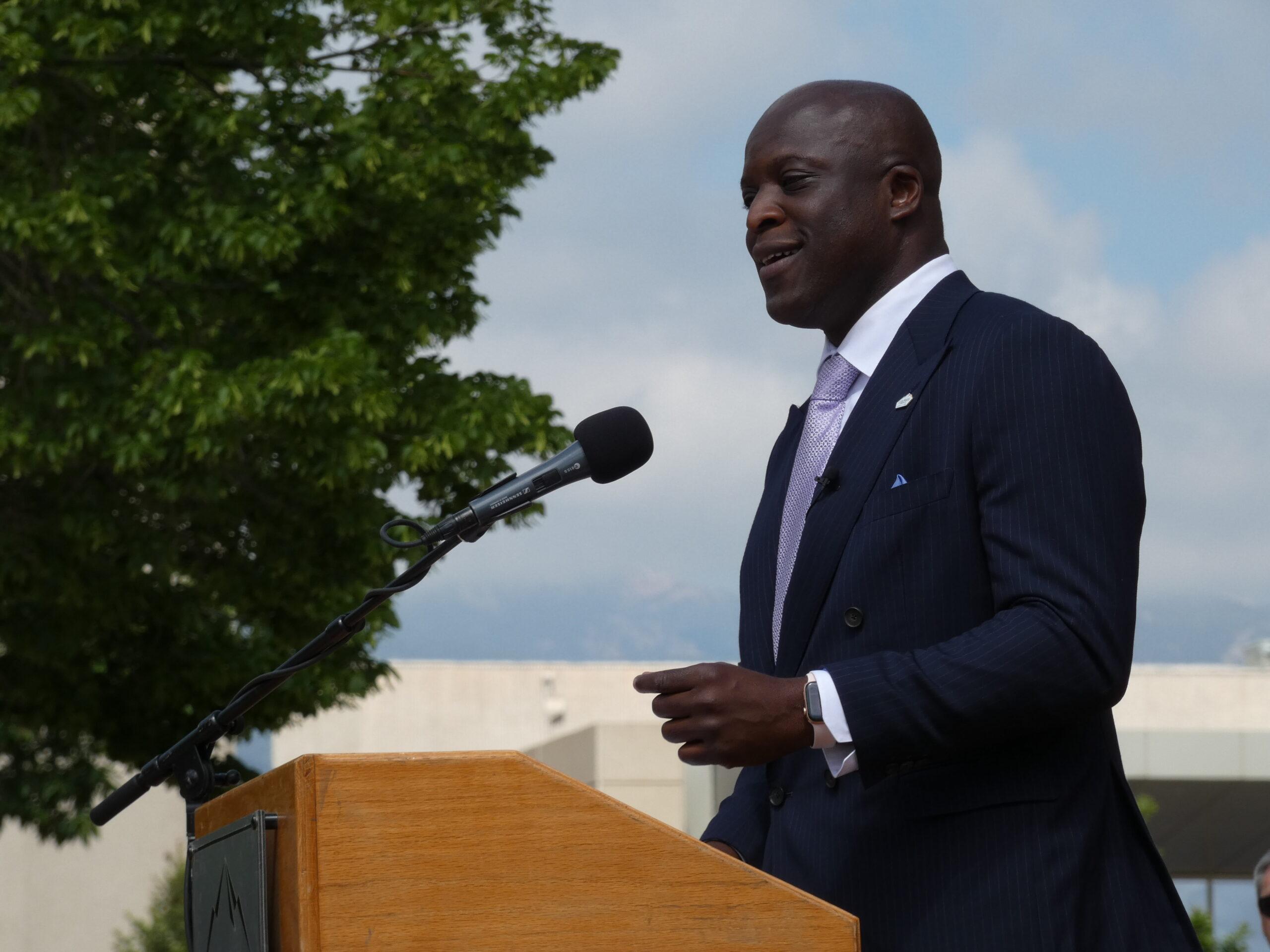
Dr. Anuj Mehta joined Colorado Matters to answer some of these questions. Mehta is a critical care and ICU physician at Denver Health, who also advised the state on vaccine allocation and crisis standards of care criteria.
This interview has been edited for clarity and length.
Nathan Heffel: Are people who received the Johnson & Johnson vaccine protected from COVID-19?
Dr. Anuj Mehta: The data overwhelmingly supports that people who received the Johnson & Johnson vaccine should receive a booster. The current recommendations are two months after the first dose, they should get a booster, whether it's Johnson and Johnson or an mRNA booster — they're eligible for all of them.
And we know that the booster provides significant protection against severe disease and hospitalization. And there's actually very recent data coming out of South Africa that suggests that two doses of the Johnson & Johnson vaccine has roughly 85 percent protection against hospitalization from omicron, which is the major concern right now.
Heffel: Is that the same level of protection as someone who received an mRNA vaccine?
Mehta: The original data suggested that there was slightly decreased efficacy as compared to the mRNA vaccines, but there was the benefit of [the Johnson & Johnson vaccine] needing one dose. What we've learned more during the pandemic — and one of the key things is that we're constantly learning more — is that additional doses, regardless of what type of vaccine you received up front, are necessary to ensure ongoing protection. Eighty-five percent protection with two doses of Johnson & Johnson to reduce the chances of being hospitalized is pretty fantastic. That's better than a lot of our other previous vaccines.
There is a possibility that the mRNA vaccines may have slightly higher protection [when combined with a booster], but we don't really know that and it's really hard to do a head-to-head comparison. What I can say is that regardless of your primary series, if you're eligible for a booster and you get a booster, you [have] good protection against severe disease and hospitalization. Even if you got Johnson & Johnson up front, and get a Johnson & Johnson booster.
Heffel: You mentioned that the Johnson & Johnson vaccine had a lower efficacy than the mRNA vaccines. Was there a thought that the lower efficacy wouldn't really matter because the other two vaccines were widely available?
Mehta: It was not that the lower efficacy wouldn't matter, it's that the efficacy at preventing hospitalization was very similar and that's an important thing. When we think about vaccine efficacy, we can talk about preventing any infection or we can talk about preventing severe disease and hospitalization. The original data from Johnson & Johnson suggested that while preventing any infection was slightly lower [than the mRNA vaccines], there was really good protection against severe disease and hospitalization.
Obviously, times have changed. We've gone through delta and now we're into omicron. What we're seeing is that there continues to be really good protection against hospitalization for those who are eligible and get a booster.
Heffel: For someone who got the Johnson & Johnson vaccine at first and decides to get an mRNA booster, which one is preferred: Moderna or Pfizer?
Mehta: [Based on the data,] the mRNA vaccines seem to generate a higher antibody level against COVID following an initial dose with Johnson & Johnson. That being said, this latest data from last week coming out of South Africa suggests that two doses of Johnson & Johnson are really effective at keeping you out of the hospital and developing severe disease. So it's hard to compare that data head-to-head.
I do think that trying to aim for higher antibody levels may make a lot of sense, but some people may only have access to Johnson & Johnson or they may have a preference for Johnson & Johnson as their second dose. I think that's completely acceptable.
Heffel: Just to note that last year both the FDA and the CDC paused Johnson & Johnson distribution because of the possibility of rare blood clots, and last month, the recommended use for Johnson & Johnson was narrowed again, specifically saying not to get the vaccine if mRNA vaccines were available. But you’re saying that it still is a valuable vaccine in the toolbox. I know for some, Johnson & Johnson is the only option because of adverse reactions to other vaccines.
Mehta: That's entirely correct. The CDC and the FDA have modified their recommendations and suggest an mRNA vaccine over Johnson & Johnson, if possible. There is a side effect profile with Johnson & Johnson that you don't see with the mRNAs, and that's the rare blood clotting issue. If somebody has a strong preference or if they have had a bad reaction to an mRNA vaccine, Johnson & Johnson remains a viable option.
But again, I do agree with the recommendation that if you can get an mRNA booster, because it does look like it leads to higher antibody levels, that may be a preference, but it's not a mandate.
Heffel: From your perspective, how should the state and other institutions view Johnson & Johnson-vaccinated people based on the data that we have today. Is one shot fully vaccinated?
Mehta: For Johnson & Johnson, one shot [does not provide] a great deal of protection against omicron. That being said, I think two doses of the mRNA vaccine, while definitely good at preventing severe disease, [are not one hundred percent effective]. We're seeing breakthrough cases in people who are eligible for a booster and haven't sought one out.
A single dose of Johnson & Johnson is not sufficient for protection. If you're more than two months out from [the first dose], you should get a booster. I say the same thing for people that have had two doses of the mRNA vaccines and are now five or six months out: they should also seek out a booster.
Heffel: Do you think those recommendations will change what it means to be fully vaccinated?
Mehta: I think how we define fully vaccinated is going to evolve over time. And eventually, when this becomes endemic, it may not even be important anymore.
Heffel: Is there a light at the end of the tunnel here? We are hearing that case numbers nationwide are going down and Colorado Governor Jared Polis says he expects the same to happen here. It’s tough with the pandemic to say anything definitive about the future, but what can you tell us about later this spring and summer from your perspective for the everyday Coloradan?
Mehta: There is a potential light at the end of the tunnel for the everyday Coloradan. I think we will see case members go down. I think we will see decreases in transmission. Given the number of patients that have been infected with mostly mild [symptoms], there will be a little bit of immunity in the community for a while.
I am terrified of new variants emerging because we continue to do a very poor job on global vaccination plans. That's really the driver of variants: the fact that we have such large populations around the world that are not vaccinated. Beyond the emergence of a new variant, I'm worried about the status of our health care system now, and I'm very worried about the status of our health care system long term.