Abstract
Objectives
To characterize the use of virtual visits, as well as compare the characteristics to in-person visits during the pandemic period.
Methods
This retrospective study included patients who had virtual and in-person ophthalmology visits from March 19, 2020, to July 31, 2020, in a large multispecialty ophthalmic center. Exclusion criteria included patients aged less than 18 years old; canceled, incomplete, mislabelled, and duplicated visits. 2943 virtual and 56,174 in-person visits were identified. A random sample of 3000 in-person visits was created. Each visit was analyzed as an individual data point.
Results
2,266 virtual visits (2,049 patients, 64.3% female, mean [SD] age 64.3 [16.6] years old) and 2590 in-person visits (2509 patients, 59.5% female, 65.9 [15.8] years old) were included. Most virtual visits were classified as comprehensive ophthalmology (34.6%), optometry-related (19.5%), and oculoplastics (13.0%). For in-person visits, the most common specialties were optometry (29.8%), comprehensive ophthalmology (23.9%), and retina and uveitis (17.3%). The most common diagnoses in the virtual group were from the eyelids, lacrimal system, and orbits group (26.9%), while in the in-person groups were choroid and retina conditions (19.3%).
Conclusions
Numerous ocular conditions were evaluated and managed through virtual visits, and external complaints and oculoplastic consults appear to be well-suited to the virtual format. Further studies focusing on visual outcomes and patient experience will be beneficial.
Similar content being viewed by others
Introduction
Telemedicine is defined as the provision of clinical services using communication technology between patient and provider. It has a variety of proposed uses in ophthalmology, including management of acute conditions such as red-eye and chronic conditions such as diabetic retinopathy, age-related macular degeneration, and glaucoma [1,2,3,4,5]. Adoption of tele-ophthalmology has been slowed by availability, cost, barriers to integrating visual assessment and imaging, and questions over diagnostic accuracy and privacy [6, 7].
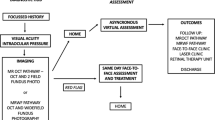
Tele-ophthalmology care is provided in one of two ways [8]. The asynchronous way uses a “store-and-forward” method, in which patient data is collected by trained personnel and uploaded to a server. The data is then examined by an ophthalmologist and a management decision is made without the need for patient-physician interaction. This model has been successfully used in retina clinics [2, 3]. In a synchronous way, real-time video conferencing may be used to simulate an in-person encounter. This model is most useful when ophthalmology specialists are not readily available [9,10,11].
As part of the recent coronavirus disease (COVID-19) pandemic, tele-ophthalmology emerged as a valuable asset to reduce unnecessary exposure and follow social distancing guidelines. Kilduff et al. described the creation of a virtual emergency tele-ophthalmology service in the UK and reported that 21.4% of the patients seen were determined to need in-person review at a hospital [12]. In France, Bourdon et al. found the use of telemedicine in a specialized ophthalmology emergency to be safe and accurate in diagnosing serious conditions [13]. In Chile, Arntz et al. piloted an open-access tele-ophthalmology clinic in which ocular surface and eyelid pathologies were the most common conditions seen [14]. Both Kilduff and Arntz reported good feedback from patients. While these studies show potential benefits of tele-ophthalmology during the (COVID-19) pandemic, they did not compare against a control group and had a limited number of cases.
On March 18, 2020, the American Academy of Ophthalmology (AAO) recommended the cessation of non-urgent and non-emergent office and/or surgical care [15]. In addition, Medicare and Medicaid relaxed regulation relating to the use of and reimbursement for telemedicine visits. Following these recommendations, institutions initiated and/or increased real-time virtual appointments for routine and urgent ophthalmic care in the United States. The purpose of this analysis is to determine the feasibility and characterize the virtual visits at a large multi-specialty ophthalmic center during the COVID-19 pandemic as well as to compare the characteristics of virtual and in-person visits during the same time period.
Methods
This study is compliant with the Health Insurance Portability and Accountability Act and adhered to the tenets of the Declaration of Helsinki. It received approval from the Cleveland Clinic Foundation Institutional Review Board and informed consent was not required due to its retrospective, observational nature. The Cole Eye Institute (Cleveland Clinic, OH) started offering real-time virtual appointments for ophthalmology care on March 19, 2020, after the AAO recommended the cessation of non-urgent and non-emergent office and/or surgical care [15]. All patients with previously scheduled in-person appointments were contacted by either providers or scheduling office personnel and were offered virtual appointments. Patients attempting to schedule new appointments were offered virtual visits from this date on. Virtual and in-person appointments were billed in the same fashion. The decision for a virtual or in-person visit was made at the patient’s discretion. Phone and video visits were available through a secure channel and patients provided verbal consent before the visit. Virtual appointments are still offered even after AAO advocated resuming all care activities on April 17, 2020.
2,943 virtual and 56,174 in-person visits from March 19 to July 31, 2020, at Cole Eye Institute were identified for this study. Using a random number generator, a sample of 3,000 in-person visits was created. This sample size was selected to provide a 95% confidence level and a 2% margin of error. All virtual and sample in-person visits were screened for exclusion criteria: patients aged less than 18 years old; canceled, incomplete, mislabelled, and duplicated visits; and visits without patient-physician interaction (test patients, imaging only visits). Clinical data were extracted between October and November 2020 from electronic medical records (EMR).
Demographic characteristics (patient’s gender, age, race, insurance, and median household income), type of virtual visit (video, phone, or hybrid), presence of technical difficulties during the visit, patient status (new or established patient), diagnosis (recorded primary diagnosis grouped by ICD-10 or code for cosmetic conditions), diagnosis status (new or established) and medication prescription were recorded and analyzed. Median household income was calculated using data from the Census Bureau according to residential zip codes registered in EMR [16]. Hybrid visits were defined as any visit with both store-and-forward and real-time conferencing components. Established patients were considered to have one or more visits recorded in the EMR up to 3 years prior to the date of interest. Diagnoses were grouped into categories according to the ICD-10 root codes by location: eyelids, lacrimal system and orbits (ICD-10 H00-H06); conjunctiva (H10-H13); sclera, cornea, iris and ciliary body (H15-H22); lens (H25-H28); choroid and retina (H30-H36); glaucoma (H40-H42); vitreous body and globe (H43-H45); optic nerve and visual pathways (H46-H48); ocular muscles, binocular movement, accommodation and refraction (H49-H52); visual disturbances and blindness (H53-H59); other disorders of eye and adnexa (H55-H59); and intraocular lens-related conditions (Z96.1). The groups “systemic conditions” and “follow-up/postoperative check” were generated to encompass the eponymous visit reason. A diagnosis was considered new if it was not mentioned in any prior ophthalmology visit.
Disposition from the visit was categorized in the following groups: (1) follow-up visit within the same ophthalmology specialty, (2) provider-initiated discontinuation of care (PID), (3) referral to a different ophthalmology specialty, (4) referral to a primary care practitioner/clinical specialist, (5) scheduled outpatient surgery, and (6) ambulatory procedures (such as intravitreal injections and incision and drainage). PID was defined as the absence of a written plan for a follow-up or follow-up pro re nata (PRN) for a patient without any registered follow-up visit. The occurrence of a follow-up appointment and the time to follow-up that had occurred by the time of data collection were also recorded. “New” prescriptions were those prescribed for the first time and those resumed after prior discontinuation. When posology changed, the prescription was noted as “changed.” If multiple medications were prescribed and one was new, then the prescription was considered “new”. Artificial tears were not included in the prescription collection.
Each visit was analyzed as an individual data point. Continuous variables were summarized with mean and standard deviation and categorical variables with frequencies in percentages. T-test or ANOVA were used to assess relationships between continuous variables. Pearson’s chi-square test of independence or Fisher’s exact test and test of proportions were used to assess relationships between categorical variables. Significant variables (P value < 0.05) are in bold. Analysis was done in R (v3.4, Mass).
Results
After applying the exclusion criteria, 2266 virtual visits and 2590 in-person visits were included in the analysis. General demographics are summarized in Table 1. The majority of the virtual visits occurred in comprehensive ophthalmology (34.6%), followed by optometry (19.5%) and oculoplastics (13.0%). For in-person visits, the most common specialties were optometry (29.8%), comprehensive ophthalmology (23.9%), and retina and uveitis (17.3%). Visit characteristics can be found in Table 2.
Among the virtual visits, 48.5% occurred through video, 48.5% through telephone and 3.0% were hybrid visits. Table 3 summarizes the characteristics of each type of virtual visit. Only 27 (1.2%) of the virtual patients experienced technical difficulties with the causes as follows: 18 application malfunctions, 3 sign-in issues, 2 connection difficulties, 2 video failures, and 2 sound problems. 14 of the video visits with technical issues were converted to phone visits, with the remaining converted to a different video platform.
Table 4 shows all diagnoses for virtual and in-person visits. The most common diagnoses in the virtual group were from the eyelids, lacrimal system, and orbits group (26.9%), followed by sclera, cornea, iris, and ciliary body (12.3%) and glaucoma (12.1%). The most common diagnoses in the in-person groups were choroid and retina conditions (19.3%), followed by disorders of the lens (13.0%) and glaucoma (12.8%). A new diagnosis was made in 28.2% of the virtual and 30.8% of the in-person patients during the visit of interest (P = 0.47). Among newly diagnosed patients, 47.4% of the virtual diagnoses were from eyelids, lacrimal system, and orbits group compared to 12.8% of the in-person diagnoses (P < 0.001). The most common in-person new diagnosis was lens disorders, with a frequency of 15.1% compared to 1.7% virtual new diagnosis (P < 0.001). A list of the five unique most common diagnoses and new diagnoses of virtual and in-person visits is provided in Supplemental Table 1.
New prescriptions for medication were initiated in 24.3% of the virtual patients after their consults compared to 13.6% of in-person patients (P < 0.001). Existing prescriptions were modified in 4.5% of the virtual patients compared to 2.0% of the in-person patients (P < 0.001). Supplemental Table 2 shows the medication types and prescription frequency in both virtual and in-person visits.
Table 5 summarizes the patient disposition in both groups. Virtual visits resulted in a follow-up 72.4% of the time compared to 70.3% following an in-person visit. Virtual patients had a provider-initiated discontinuation of care in 15.9% of visits compared to 10.8% of in-person patients. Referrals to the patient’s primary care provider or clinical specialist occurred in 0.8% of virtual patients while none of the in-person patients were. Ambulatory procedures were scheduled for 0.2% of the virtual patients compared to 7.2% of in-person patients. 95.0% of the procedures after an in-person visit occurred on the same day of the visit. Intravitreal injections comprised 75.0 % of the ambulatory procedures in the virtual group and 70.6% in the in-person group. Referrals to a different ophthalmology specialty and outpatient surgeries were not significantly different between groups.
At the time of final data collection (October and November 2020), 73.5% of the follow-ups after virtual visits had occurred, compared to 46.6% after in-person visits. Among the completed follow-ups after a virtual visit, 15.4% were once again virtual with only 2.7% of the completed follow-ups after an in-person visit being virtual. Only 7 patients were determined to need an in-person follow-up visit on the same day after a virtual encounter. Next-day follow-ups occurred in 1.1% of the completed follow-ups following a virtual encounter and 1.1% following an in-person encounter, while 5.1% and 7.1% respectively occurred between 2 and 6 days. Patient-associated discontinuation of care occurred due to cancelations (4.6% and 3.5% in the virtual and in-person visits, respectively), no shows (2.8% and 2.1%) and failure to schedule a planned follow-up visit (10.4% and 2.4%). 8.7% of the follow-ups after virtual visits were due on a future date (i.e., had not occurred by the time of data collection), compared to 45.5% of the follow-ups after in-person visits.
Discussion
The ongoing COVID-19 pandemic created a demand for high-quality, efficient, tele-ophthalmology care. Many institutions around the world altered existing practices or established virtual platforms to provide medical assistance for patients with acute and chronic conditions [12,13,14, 17,18,19]. This study characterizes one ophthalmic center’s experience with virtual consultations.
Virtual visits were conducted across multiple ophthalmic specialties and addressed a variety of ocular complaints from new and established patients. Referrals and surgical planning were possible through the virtual setting. These metrics suggest providers can diagnose and even manage some ocular conditions virtually. Given the spectrum of ophthalmic conditions seen, not all conditions can feasibly be treated. However, in characterizing real-world experience with tele-ophthalmology, this study does highlight several conditions that lend themselves to tele-ophthalmology practice.
Proportionally, oculoplastics had the highest number of virtual visits. When grouped together, chalazion, external and internal hordeolum were the most common diagnoses in the virtual group. This observation would be expected as this specialty and diagnosis group does not require many specialized instruments, visual assessment, imaging, or exam maneuvers. Other studies have also found oculoplastics transitions well to the virtual format [20, 21]. Conversely, glaucoma, cornea, and retina evaluation require detailed exam maneuvers, supplemental imaging, and other steps which are not as appropriately addressed during virtual consultations. Accordingly, the adjusted proportion of virtual retina consultations in this study is low, which supports this observation. Though a high proportion of glaucoma and cornea consultations occurred virtually, they were related to uncomplicated complaints such as medication reconciliation. Hybrid visits and home monitoring devices might bridge this gap. However, this study found providers did not gravitate to the hybrid model and home monitoring devices were not studied here. Finally, only 4 (0.2%) ambulatory procedures were observed in the virtual setting compared to 186 (7.2% in the in-person setting), suggesting that virtual encounters may interfere with management decisions.
The higher prevalence of oculoplastic and external eye-related visits in the virtual setting may be tied to the high rate of provider-initiated discontinuation of care and patient failure to schedule a follow-up visit. Many of these conditions were seen post-operatively or for a check into the status of a self-limited or easily treatable disease. For this reason, a provider might be inclined to discontinue follow-up, or a patient to not schedule a follow-up visit when the problem is resolved. However, this observation also raises the possibility that virtual visits are prone to loss to follow-up. Combined with a low ambulatory procedure rate after virtual visits, it is possible that virtual visits may constitute a barrier to care when concerned with a very time-sensitive visits or chronic ones. Although long-term data is needed, in the meantime it may be prudent to dedicate resources to at-risk patients.
A follow-up visit took place after 72.4% of the virtual visits in this study, which conflicts with previous research in real-time tele-ophthalmology during the COVID-19 pandemic. Kilduff et al. reported that only 21.4% of the patients in an emergency tele-ophthalmology setting required in-person review [12]. In a similar study, Bourdon et al. stated that 27.0% of teleconsultations were followed in-person review [13]. Given that visits in the present study ranged from acute to chronic conditions, the higher rate of follow-up is expected. Indeed, only 7 (0.6%) virtual visits required same-day in-person examination, reinforcing this observation. Notably, virtual follow-ups were carried out more often after virtual visits as compared to in-person visits, which suggests a positive first virtual visit might lead to a second. Given high levels of patient satisfaction with real-time virtual encounters and increasing acceptance of this setting, the idea is plausible [12, 14]. However, some of these visits may have also been scheduled to reduce the risk of COVID-19 exposure. Although a similar follow-up rate in the virtual and in-person settings was observed (72.4% and 70.3% respectively), the comparisons between groups are confounded by differing demographic characteristics, ophthalmology specialties, and diagnoses.
With respect to demographics, most patients for both virtual and in-person visits were female, which is consistent with previous observations [14, 22]. Virtual patients were younger and of higher socioeconomic status (SES), which coincides with the demographic most likely to handle technology according to a recent Pew Research poll [23]. Video patients were the youngest group, as noticed by Hammersley et al. [24]. Additionally, our study observed that 1.0 % of virtual visits were with uninsured patients versus none in-person. Given the small number of these patients, both results may be due to the sample of the population itself. The predilection of uninsured patients for the virtual format may be ascribed to multiple factors, which are beyond this discussion.
The young, female, and high SES cohort raises a question of paradoxical inaccessibility to a format that is, in part, meant to equalize patient access [25]. Part of this might be due to technology. Video visits do require basic infrastructure and are susceptible to technical difficulties, especially due to reliance on internet connection. Conversely, phone appointments are widely available and may be more time-efficient, but the lack of visual clues interferes with the diagnostic process. A 2016 US Census Bureau report found that 49.0% of households with annual family incomes lower than $20,000 have internet in the home, compared to 90.0% of households with incomes higher than $100,000 [26]. The same report found that 96.0% of households have telephone access and the lower-income household is much more likely to have telephone access as compared to internet access at home. Mobile internet is an alternative, however, 59.0% to 72.0% of all households have subscriptions to mobile plans. This is the setting of 78.0 to 87.0% of all households with cellular phone plan alone. Such findings suggest phone – landline or cellular – remains a reliable modality of reaching a patient when a video fails. However, this leaves the provider and patient in a situation no different than before the video era.
The strengths of this study include a large and diverse population, derived from a multispecialty clinic. Complaints ranged from urgent complaints to the monitoring of chronic conditions and medication checking. In addition, this study offers a control group for comparison in the form of a randomly selected in-person cohort from the same time period. Additionally, the study took on quantitative aspects of virtual versus in-person ophthalmology visits, an approach that is especially salient as the virtual format requires further development.
Limitations in this study include its retrospective, observational nature. The selection of a random sample of in-person visits for comparison may have introduced a sampling bias. Since visits rely on phone or internet connection, a selection bias could have been introduced if only those with a successful response to technical problems were charted. In this case, visits that were not completed might not have been fully characterized. Moreover, this study tracked virtual visits from the program’s implementation through its early development, so it is likely that operational changes occurred as inefficiencies in the system were identified and remediated. These development-related changes are beyond the scope of this study’s capabilities to track and report on, however, they likely did not influence the conclusion. Regarding disposition after visits, a comparison between virtual and in-person could not be performed reliably due to the reasons discussed earlier. Strictly speaking, this study’s conclusions apply to Cole Eye Institute and have limited external generalizability. Furthermore, conclusions regarding the feasibility of ophthalmic care are limited to the most prevalent conditions. By the nature of this study, definitive conclusions regarding the feasibility of virtual visits are not possible however, these findings may guide future, randomized trials comparing the success of virtual format in meeting the care needs of multiple conditions including imaging use and surgical planning.
In conclusion, patients and providers are using tele-ophthalmology in routine practice during the COVID-19 pandemic despite its limitations. Virtual visits may be well suited to oculoplastic and external eye complaints. Discontinuation of care occurred more often among virtual patients, pointing to an improvement opportunity in terms of scheduling follow-up. Future studies oriented to visual outcomes, long-term follow-up, and patient experience are needed.
Supplementary information is available at Eye’s website.
Summary Table
What was known before
-
The COVID-19 pandemic challenged health care.
-
Ophthalmology virtual visits implementation has been slowed by availability, cost, barriers to integrating visual assessment and imaging, and questions over diagnostic accuracy and privacy.
What this study adds
-
Numerous ocular conditions were evaluated and managed through virtual visits.
-
Virtual visits may be well suited to oculoplastic and external eye complaints.
-
Discontinuation of care occurred more often among virtual patients, pointing to an improvement opportunity in terms of scheduling follow-up.
References
Ribeiro AG, Rodrigues RAM, Guerreiro AM, Regatieri CVS. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol. 2014;77:214–8.
Kern C, Kortuem K, Hamilton R, Fasolo S, Cai Y, Balaskas K, et al. Clinical outcomes of a hospital-based teleophthalmology service: what happens to patients in a virtual clinic? Ophthalmol Retin. 2019;3:422–8.
Lee JX, Manjunath V, Talks SJ. Expanding the role of medical retina virtual clinics using multimodal ultra-widefield and optical coherence tomography imaging. Clin Ophthalmol. 2018;12:2337–45.
Tsaousis KT, Empeslidis T, Konidaris VE, Kapoor B, Deane J. The concept of virtual clinics in monitoring patients with age-related macular degeneration. Acta Ophthalmol. 2016;94:e353–5.
Barrett C, O’Brien C, Loughman J. Glaucoma referral refinement in Ireland: managing the sensitivity-specificity paradox in optometric practice. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt. 2018;38:400–10.
Sharma M, Jain N, Ranganathan S, Sharma N, Honavar SG, Sharma N, et al. Tele-ophthalmology: need of the hour. Indian J Ophthalmol. 2020;68:1328–38.
Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124:1729–34.
Ting DS, Gunasekeran DV, Wickham L, Wong TY. Next generation telemedicine platforms to screen and triage. Br J Ophthalmol. 2020;104:299–300.
Johnson KA, Meyer J, Yazar S, Turner AW. Real-time teleophthalmology in rural Western Australia. Aust J Rural Health. 2015;23:142–9.
Sommer AC, Blumenthal EZ. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefe’s Arch Clin Exp Ophthalmol. 2020;258:2341–52.
Mueller KJ, Potter AJ, MacKinney AC, Ward MM. Lessons from tele-emergency: improving care quality and health outcomes by expanding support for rural care systems. Health Aff. 2014;33:228–34.
Kilduff CLS, Thomas AAP, Dugdill J, Casswell EJ, Dabrowski M, Lovegrove C, et al. Creating the Moorfields’ virtual eye casualty: Video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Heal Care Inform. 2020;27:1–5.
Bourdon H, Jaillant R, Ballino A, El Kaim P, Debillon L, Bodin S, et al. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: experience with 500 patients in March and April 2020. J Fr Ophtalmol. 2020;43:577–85.
Arntz A, Khaliliyeh D, Cruzat A, Rao X, Rocha G, Grau A, et al. Open-care telemedicine in ophthalmology during the COVID-19 pandemic: a pilot study. Arch Soc Esp Oftalmol. 2020;95:586–90.
David W, Parke II M. Recommendations for urgent and nonurgent patient care. American Academy of Ophthalmology. 2020. https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care
Bureau USC 2010, American Community Survey, Median Household Income. 2010. https://data.census.gov/cedsci
Patel S, Hamdan S, Donahue S. Optimising telemedicine in ophthalmology during the COVID-19 pandemic. J Telemed Telecare. 2020. https://doi.org/10.1177/1357633X20949796. Online ahead of print.
Khor WB, Yip L, Zhao P, Foo VHX, Lim L, Ting DSW, et al. Evolving practice patterns in Singapore’s Public Sector Ophthalmology Centers during the COVID-19 pandemic. Asia-Pacific. J Ophthalmol. 2020;9:285–90.
Lai KE, Ko MW, Rucker JC, Odel JG, Sun LD, Winges KM, et al. Tele-neuro-ophthalmology during the age of COVID-19. J Neuroophthalmol. 2020;40:292–304.
Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye. 2020;34:1193–5.
Jamison A, Diaper C, Drummond S, Tejwani D, Gregory ME, Cauchi P, et al., Telemedicine in oculoplastics: the real-life application of video consultation clinics. Ophthalmic Plast Reconstr Surg. (2020)
Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pr. 2000;49:147–52.
Vogels EA, Millennials stand out for their technology use, but older generations also embrace digital life. 2019. https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/
Hammersley V, Donaghy E, Parker R, McNeilly H, Atherton H, Bikker A, et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pr. 2019;69:E595–E604.
Annaswamy TM, Verduzco-Gutierrez M, Frieden L. Telemedicine barriers and challenges for persons with disabilities: COVID-19 and beyond. Disabil Health J. 2020;13:100973.
Turner SD, Digital denied: the impact of systemic racial discrimination on home-internet adoption. 2016. https://www.freepress.net/sites/default/files/legacy-policy/digital_denied_free_press_report_december_2016.pdf
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
CCSV was responsible for extracting and analyzing data, managing the project, interpreting results, updating references, and writing the manuscript. JCM was responsible for extracting and analyzing data, interpreting results, updating references, and writing the manuscript. AII was responsible for extracting and analyzing data. MK was responsible for designing the review protocol and extracting data. AK was responsible for extracting data and managing the project. SG contributed to extracting data and creating tables. MO contributed to extracting data. AR was responsible for designing the research project and reviewing the manuscript. RPS was responsible for designing the research project, administering the project, and reviewing the manuscript. KET was responsible for designing the research project, administering the project, interpreting results, and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
CSV, JCM, AII, MAK, AK, SWG, and MO report no conflicting interests. AR reports personal fees from Alcon, personal fees from Allergan, research and personal fees from Genentech, research and personal fees from Novartis, personal fees from Regeneron, personal fees from Samsara, and personal fees from Zeiss. RPS reports personal fees from Genentech/Roche, personal fees from Alcon/Novartis, grants from Apellis, grants from Graybug, personal fees from Zeiss, personal fees from Bausch+Lomb, and personal fees from Regeneron Pharmaceuticals, Inc. KET reports research fees from Zeiss and personal fees from Genentech/Roche.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valentim, C.C.S., Muste, J.C., Iyer, A.I. et al. Characterization of ophthalmology virtual visits during the COVID-19 pandemic. Eye 37, 332–337 (2023). https://doi.org/10.1038/s41433-022-01938-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01938-2