Abstract
New predictors that could boost early detection of preeclampsia (PE) and prognosticate its severity are urgently needed. We examined serum miR-17, miR-363, MALAT-1 and HOTAIR as potential biomarkers of PE risk, onset and severity. This prospective study included 160 pregnant females; 82 PE cases and 78 healthy pregnancies. Serum samples were collected between 20 to 40 weeks of gestation. Early-onset PE was defined as developing clinical manifestations at ≤ 34 gestational weeks. Severe PE was defined as systolic blood pressure ≥ 160 mmHg and/or diastolic blood pressure ≥ 110 mmHg and proteinuria (≥ 2 g/24 h or ≥ 2+ dipstick). Selection of PE-related non-coding RNAs and functional target gene analysis were conducted using bioinformatics analysis. Expression profiles were assessed by RT-qPCR. Serum miR-363 and MALAT-1 were downregulated, meanwhile miR-17 was upregulated, and HOTAIR was not significantly altered in PE compared with healthy pregnancies. miR-17 was elevated while miR-363 and MALAT-1 were reduced in severe versus mild PE. miR-363 was lower in early-onset versus late-onset PE. MALAT-1, miR-17 and miR-363 showed diagnostic potential and discriminated severe PE, whereas miR-363 distinguished early-onset PE in the receiver-operating-characteristic analysis. miR-363 and MALAT-1 were significantly associated with early and severe PE, respectively in multivariate logistic analysis. In PE, miR-17 and MALAT-1 were significantly correlated with gestational age (r = − 0.328 and r = 0.322, respectively) and albuminuria (r = 0.312, and r = − 0.35, respectively). We constructed the MALAT-1, miR-363, and miR-17-related protein–protein interaction networks linked to PE. Serum miR-17, miR-363 and MALAT-1 could have utility as new biomarkers of PE diagnosis. miR-363 may be associated with early-onset PE and MALAT-1 downregulation correlates with PE severity.
Similar content being viewed by others
Introduction
Preeclampsia (PE) is a multi-systemic pregnancy disorder that globally affects 2–10% of pregnancies, and currently is among the most common causes of maternal death1. PE mostly uncovers pre-existing endothelial dysfunction, metabolic and vascular diseases2, which necessitate long-term monitoring of women with prior exposure to PE, preterm birth, or delivery of an infant small for gestational age3. Thus, new biomarkers of PE risk, onset and severity are urgently needed.
The pathogenesis of PE includes inadequate trophoblastic invasion, developmental abnormalities of placental vasculature and placental underperfusion, however the exact pathophysiological mechanism remains unknown4. Thereby, recognizing the mechanistic insights underlying trophoblastic behavior and pathology in PE will clear up new biomarkers for its diagnosis and prognosis as well as novel therapeutic targets.
Non-coding RNAs (ncRNAs), including microRNAs (miRNAs; 18–22 nucleotides) and long ncRNAs (lncRNAs; > 200 nucleotides) are involved in several cellular paradigms in the placenta, including trophoblastic invasion, cell proliferation and endothelial function5,6. lncRNAs also act as competing endogenous RNAs (ceRNAs) for miRNAs, and this crosstalk was linked to PE pathology6. Deregulated miRNAs and lncRNAs are released into the circulation from the defective placenta in PE and have come out as potential biomarkers for its early screening and diagnosis and as novel targets for its prevention and treatment7,8,9.
Although several reports revealed the probable usefulness of measuring certain ncRNAs as circulating biomarkers of PE7,8,9, a study by luque et al. concluded that measurement of maternal serum miRNA at the first-trimester of pregnancy lacks any predictive value for early PE10. For this divergence, more investigations are needed to shed light on the precise role of PE-related ncRNAs and their possible cross-interaction in predicting its onset and severity. Accordingly, we have conducted a systematic bioinformatics approach to select PE-associated lncRNAs and miRNAs, and then examined candidate lncRNAs-miRNAs predicted and reported interactions. Herein, the lncRNAs metastasis associated lung adenocarcinoma transcript-1 (MALAT-1) and homeobox transcript antisense RNA (HOTAIR) as well as miR-17 and miR-363 were selected.
miR-17, a member of the miR-17-92 cluster, is a placental-specific miRNA which is largely located in various subtypes of trophoblasts, regulating important trophoblastic cell events, including differentiation, angiogenesis and apoptosis9. In particular, miR-17 regulates multiple steps during placental angiogenesis and its deregulation causes placental developmental defects11. Another placental-related miRNA is miR-363, a member of miR-106a-363 cluster, which is highly expressed during placental development in rapidly proliferating cytotrophoblasts (CTB), the most metabolically active cells in the placenta. Members of miR-17-92 and miR-106a-363 clusters are MYC-responsive targets, an important regulator of early placentation12, and were established to target several genes that are involved in CTB proliferation, differentiation, angiogenesis and metabolic reprogramming12. The lncRNA MALAT-1 regulates trophoblast invasion during placental development; its knockdown impaired trophoblast invasion and proliferation, suppressed the cell cycle progression and promoted apoptosis13. HOTAIR lncRNA regulates proliferation, invasion and apoptosis of placental trophoblasts; its overexpression decreased their invasive capacity and increased cell apoptosis14. However, the exact role of these ncRNAs, their crosstalk and clinical relevance in PE are not fully elucidated.
Thereby, the present study investigated the circulating expression profiles of miR-17, miR-363, MALAT-1 and HOTAIR in sera of PE patients and normal pregnancies, and evaluated their potential value as biomarkers of PE risk, onset and severity. We also explored the correlation between these ncRNAs and clinicopahological data of PE patients. Target gene analysis was also conducted using online softwares and databases to functionally relate these ncRNAs to PE pathogenesis through constructing the target protein–protein interaction (PPI) networks linked to PE.
Results
PE characteristics
Both PE patients and healthy pregnancies were comparable in terms of age, smoking status, body mass index (BMI), parity, abortion, gravidity, fasting blood sugar, liver function tests, serum urea and hematological parameters (P > 0.05). Patients with PE exhibited significantly higher systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), C-reactive protein (CRP) (P < 0.0001 for each), serum creatinine and uric acid levels (P = 0.0003 for each). PE patients showed low amniotic fluid (oligohydraminos), intrauterine growth restriction (IUGR), and abnormal Doppler (P < 0.0001 for each) more frequently than the control group. Moreover, PE patients had lower gestational age (GA) (P = 0.045) and fetal birth weight (FBW) (P < 0.0001), in addition to, more frequent caesarean delivery (P = 0.003) (Table 1).
Thirty-four percent of patients were diagnosed with mild PE while the rest had severe PE. Thirty-nine percent of PE patients were early-onset cases while the others were late-onset cases.
Expression of studied ncRNAs in PE versus healthy pregnancies
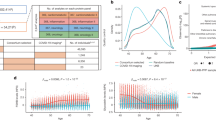
The studied ncRNAs were expressed in sera of PE cases and healthy pregnancies with varying levels (Fig. 1). Notably, serum miR-17 was upregulated by a median 3.5-fold (P = 0.003), while serum miR-363 and MALAT-1 were downregulated by median 4 and 2.1-fold, respectively (P = 0.001 and P = 0.005, respectively) in PE patients compared to controls. On the other hand, serum HOTAIR expression levels was not changed between PE patients and healthy pregnancies (P = 0.25) (Fig. 1 and Table 2).
Serum expression profiles of miR-17, miR-363, MALAT-1 and HOTAIR in PE patients. The box represents the 25–75% percentiles; the line inside the box represents the median and the upper and lower lines representing the 10%-90% percentiles of relative gene expression levels (2−∆Ct) of studied parameters in PE (n = 82) compared to healthy pregnancies (n = 78).
Expression of studied ncRNAs in PE patients regarding PE severity
Serum miR-17 levels were elevated in severe PE compared to mild cases (P = 0.002). Conversely, serum miR-363 (P = 0.005) and MALAT-1 (P = 0.0004) levels were reduced in severe PE compared to mild disease. Again, no changes were observed in serum HOTAIR levels between the two groups (P = 0.67) (Table 2).
Expression of studied ncRNAs in PE patients regarding PE onset
Only serum levels of miR-363 showed differential expression between early-onset and late-onset PE cases, with markedly lower levels in the early-onset PE group (P = 0.001) (Table 2). To further examine the role of studied ncRNAs with the risk of early- or late-onset PE, we conducted a stratification analysis comparing early- or late-onset PE vs early or late controls (with matched gestational weeks at delivery, P > 0.05), respectively (Table 2). We recorded a marked downregulation of serum miR-363 in early-onset PE compared with early controls (P < 0.0001), while levels of other studied ncRNAs were not significantly different in the same comparison. On the other hand, we observed serum miR-17 upregulation (P = 0.0003) as well as MALAT-1 downregulation (P < 0.0001) in the late-onset PE group when compared with the late controls, while miR-363 and HOTAIR levels were comparable among the two groups (P = 0.8 and 0.68, respectively).
Correlation of studied ncRNAs with each other in PE patients
In the whole PE group, we recorded many significant correlations between serum levels of the investigated ncRNAs where MALAT-1 was positively correlated with both miR-17 (r = 0.401, P = 0.017) and HOTAIR (r = 0.453, P = 0.0004) expression levels. Also, there was a positive correlation between miR-17 and miR-363 (r = 0.273, P = 0.015) (Table 3).
Correlation of studied ncRNAs with clinicopathological data of PE patients
In the whole PE group, we noticed many significant correlations between serum levels of the investigated ncRNAs and clinicopathological data (Table 3). MiR-17 showed positive correlations with BMI (r = 0.43, P = 0.002), IUGR (r = 0.3, P = 0.04), abnormal Doppler (r = 0.234, P = 0.046), low amniotic fluid (r = 0.245, P = 0.044), mode of delivery (MOD) (r = 0.441, P = 0.004) and albuminuria (r = 0.312, P = 0.04), while inversely correlated with GA (r = − 0.328, P = 0.036) and FBW (r = − 0.324, P = 0.039). miR-363 recorded negative correlations with BMI (r = − 0.315, P = 0.045) and abnormal Doppler (r = − 0.26, P = 0.04) and a positive correlation with GA (r = 0.412, P = 0.006). MALAT-1 was negatively correlated with maternal age (r = − 0.341, P = 0.029) and albuminuria (r = − 0.35, P = 0.025), while showed a positive correlation with GA (r = 0.322, P = 0.04). HOTAIR was positively correlated with albuminuria (r = 0.274, P = 0.039). This correlations link the deregulated levels of our studied ncRNAs with PE pathology.
Performance of investigated serum ncRNAs in PE diagnosis, onset and severity
Serum miR-17, miR-363, and MALAT-1 distinguished PE patients from the healthy controls in the ROC curve analysis with AUC = 0.67, P = 0.009, sensitivity (SN) = 73% and specificity (SP) = 62% at a cut off > 1.6 (fold, 2−∆∆Ct) for miR-17; AUC = 0.76, P < 0.0001, SN = 61% and SP = 95% at a cut off < 0.17-fold for miR-363, and AUC = 0.66, P = 0.01, SN = 80% and SP = 62% at a cut off < 0.62-fold for MALAT-1 (Fig. 2). By comparison, miR-363 was a potential discriminator and seems to have better diagnostic accuracy than miR-17 and MALAT-1, but differences between AUCs didn't reach statistical significance (difference = 0.09, P = 0.079, difference = 0.1, P = 0.11, respectively).
miR-17, miR-363 and MALAT-1 were potential discriminators of severe from mild PE cases with AUC = 0.71, P = 0.002, SN = 92.31% and SP = 57.14% at a cut off > 1.47-fold for miR-17; AUC = 0.7, P = 0.004, SN = 70.37% and SP = 71.43% at a cut off < 0.33-fold for miR-363, and AUC = 0.73, P = 0.0005, SN = 81.48% and SP = 71.43% at a cut off < 0.66-fold for MALAT-1 (Fig. 2).
Only miR-363 was a potential discriminator of early-onset from late-onset PE cases (AUC = 0.71, P = 0.001) with SN = 92% and SP = 56.25% at a cut off < 0.018-fold. Moreover, it was the only studied ncRNA that distinguished early-onset PE patients from early controls (AUC = 0.82, P < 0.0001) with SN = 75% and SP = 95% at a cut off < 0.14-fold. On the other hand, miR-17 (AUC = 0.72, P = 0.0004) and MALAT-1 (AUC = 0.77, P < 0.0001) were potential discriminators of late-onset PE patients from late controls with SN = 80% and SP = 68% at a cut off > 3.1-fold for miR-17, and SN = 72% and SP = 79% at a cut off < 0.52-fold for MALAT-1 (Fig. 3). All cutoff values were expressed as fold change (2−∆∆Ct) and determined as the value that maximized the sum of SN and SP.
Association of studied parameters with early PE and PE severity using logistic regression analysis
The variables associated with early PE (early-onset PE vs early controls) (Table 4) and its severity (severe vs mild PE) (Table 5) were identified using univariate and multivariate logistic regression analyses. miR-363 along with clinical parameters; SBP, DBP, MAP, CRP, creatinine, IUGR, abnormal Doppler and low amniotic fluid come out to be associated with early PE (P < 0.05) in the univariate analysis. miR-363 together with SBP come out as the final independent variables associated with early PE in the multivariate analysis with adjustment by maternal age and GA as cofounders. Additionally, MALAT-1 along with clinical data; SBP, DBP, MAP, creatinine, uric acid, IUGR and abnormal Doppler were shown to associate with PE severity in the univariate analysis for (P < 0.05). Then, MALAT-1 together with SBP and serum uric acid turned out as the final independent variables associated with the severity of PE in the multivariate analysis with adjustment by maternal age.
Results of functional analysis
We listed the selected target genes of miR-17, miR-363 and MALAT-1 most functionally linked to PE, their protein–protein interaction (PPI) P value, gene ontology (GO) biological process and KEGG pathways of the PPI in Table 6. The PPI network construction for miR-17, miR-363 and MALAT-1 is visualized in Fig. 4.
Construction of non-coding RNA-related PPI networks linked to PE. (A) miR-17, (B) miR-363 and (C) MALAT-1. Pathway Studio online software was used. Data relevant to KEGG software http://www.kegg.jp/kegg/kegg1.html.
Discussion
New molecular biomarkers that give mechanistic insights in PE and could boost its screening, early detection and prognosis are urgently needed to reduce PE-associated maternal death. In this exploratory study, we have conducted a systematic bioinformatics analysis and selected 4 PE-related ncRNAs for our biomarker study. Results showed that serum miR-17, miR-363 and MALAT-1 expression profiles were surrogate biomarkers of PE risk and severity. Furthermore, we are the first to show an association between serum miR-363 and early-onset PE, and between serum MALAT-1 downregulation and PE progression.
In PE patients, we observed serum MALAT-1 downregulation with miR-17 upregulation, which verify their cross-interaction in PE development and progression. To explain, miR-17, MALAT-1 and also HOTAIR commonly regulate vascular endothelial growth factor A (VEGFA)15,16, through which they could presumably crosstalk to regulate angiogenesis. Taking into account that MALAT-1 and HOTAIR were shown to act as ceRNAs for miR-1717,18, thus MALAT-1 underexpression could elevate miR-17 with concomitant downregulation of miR-17 target genes, including VEGFA resulting in impaired placental angiogenesis. On the other hand, both MALAT-1 and HOTAIR are estrogen receptor α (ERα) and hypoxia inducible factor-1α (HIF1A) transcriptional targets19,20,21. As HIF1A is a predicted target for miR-17 (Table 6) and ERα is a known target of miR-17-92 family12, one may speculate that miR-17 upregulation could possibly affect HIF1A and ERα expression and hence the transcription of MALAT-1 gene. However, this relation should be further investigated.
Although several target genes and biological pathways have been previously identified for our selected ncRNAs and were linked to PE pathogenesis, we have conducted target gene analysis and PPI network analysis to further explain the role of miR-17, MALAT-1 and miR-363 in PE pathogenesis (Table 6 and Fig. 4). We found several common targets and biological pathways for miR-17, miR-363 and MALAT-1 which are involved in VEGF signaling pathway, HIF signaling, ephrin receptor signaling, transforming growth factor (TGF)-β/SMAD signaling as well as epidermal growth factor receptor (EGFR), MAPK, PI3K/Akt, JAK/STAT and canonical Wnt signaling pathways. Notably, these pathways are known to regulate many trophoblastic cell activities4,5. Together, these data clarify that these miRNAs could interplay in PE development and progression.
The observed elevation of serum miR-17-5p in PE coincides with previously reported in whole maternal peripheral blood22 and placenta9,11,23 among PE patients. Indeed, circulating miRNAs in pregnant women mainly originate from the placenta. Conversely, miR-17 was not altered in plasma9, whole maternal blood or placenta of PE patients24,25. Mechanistically, miR-17 targets a set of genes including, VEGFA, ephrin type-B receptor 4 (EPHB4), EPHA4, EPHA5, ephrin-B2 (EFNB2), and matrix metalloproteinases (Table 6, Fig. 4). These genes are cardinal for vascular remodeling and CTB invasion during placentation11. In early placental development low levels of miR-17 maintains trophoblastic differentiation by upregulating EFNB2 and EPHB4, but in PE miR-17 overexpression suppresses these genes causing inhibition of trophoblastic invasion and defective placental vasculature11,23. Moreover, miR-17 promotes oxidative stress-induced apoptosis via targeting STAT3 which interfere with PE development26.
We observed elevated serum miR-17 in severe PE as well as in late-onset PE patients vs late controls, but not among early and late gestational stages of PE. Similarly, miR-17 was upregulated in severe PE placentas9 and in whole maternal peripheral blood in severe PE22. Conversely, higher postpartum expression of miR-17-5p was observed within late PE patients compared to those with early PE22. However, placental, plasma and whole maternal blood miR-17 were not correlated with either PE severity or onset in other studies9,24,25. Our target gene analysis could justify the link between miR-17 and PE severity on the basis that miR-17 is predicted to target TGFBR2, SMAD6/SMAD7 and SMAD4/SMAD5 thus could modulate TGF-β signaling. Indeed, this pathway was shown to be central to PE pathogenesis27.
The observed association of miR-17 with BMI is consistent with its adipogenesis-promoting actions28, confirming that obesity is a risk factor for PE, with many common mechanisms interplay to link obesity with a higher risk of PE29. The negative correlation between miR-17 and GA is consistent with that miR-17 expression was altered in porcine placenta of different GAs, proposing that miR-17 declines as GA advances30. miR-17 downregulation was also reported in third trimester placentas compared with first trimester ones31. This correlation is attributed to that miR-17 targets VEGFA which is responsible for increasing the growth of placental vasculature as GA increases32. Although previous reports were discrepant33,34, the negative correlation between miR-17 and FBW intensifies that miR-17 can be used as a prognostic biomarker for maternal diseases affecting birth weight35. Despite controversial reports24,25, our results might link dysregulated miR-17 and IUGR, a well-known risk factor of PE especially the severe form.
The observed serum miR-363 downregulation mimics prior reports of placental miR-363 underexpression in PE9,36,37. Conversely, plasma and serum miR-363 expression did not alter in PE throughout the 3 trimesters9,38. miR-363 is an anti-apoptotic miRNA; its downregulation leads to excessive placental trophoblast apoptosis exhibited in PE38. Furthermore, inhibition of trophoblast cell differentiation and invasion was associated with decline of placental miR-363 expression39. To explain, we showed that miR-363 is predicted to target several genes, among them integrin-A6 (ITGA6), a receptor for cell-extracellular matrix interaction important for trophobalst migration and invasion; and Kruppel-like factor 4 (KLF4), a transcription factor which regulates angiogenesis.
The observed decline of serum miR-363 in severe and early-onset PE coincided with previously reported in PE placenta9,36,37. However, plasma miR-363 was not correlated with PE severity9 or onset38 in other studies. miR-363 deregulation associates with PE severity by targeting placental sodium coupled neutral amino acid transporters causing variation in amino acids transport and nutrient transfer, ultimately leading to PE pathology39. Moreover, aberrantly expressed miR-363 together with EZH2 and nudix hydrolase 21 were shown to influence CTBs growth and migration40. The observed miR-363 downregulation in both early-onset and severe PE supports the notion that early-onset PE is often more severe than late-onset PE and largely originates from poor placentation in the first trimester41. Both PE phenotypes exhibit intensified systemic inflammatory responses exposing vessels and cells to overwhelming oxidative stress, with consequent apoptosis37.
The recorded negative correlation between miR-363 and BMI is consistent with its anti-adipogenic properties42. The positive correlation between serum miR-363 and GA coincides with placental miR-363 upregulation in third versus first trimester31. However, serum miR-363 was not correlated with GA throughout the three trimesters in PE37.
The observed downregulation of serum MALAT-1 in PE matches the previously reported data in placenta, umbilical cords and mesenchymal stem cells (MSCs) derived from PE patients13,15,43. Using a bioinformatics approach, we identified a MALAT-1-related PPI network linked to PE, including PTEN, SMAD4, MMP2, MMP9, E-cadherin, N-cadherin, β-catenin, Elavl1, CTHRC1, CCT4, HMMR, MCL-1, BCl-2, PTBP3, PFKFB3 and C-FOS. This PPI was enriched in extracellular matrix organization, cell migration, embryo development, cellular response to oxidative stress and apoptosis and is involved in platelet-derived growth factor receptor signaling, TGF-β/SMAD signaling, ephrin receptor signaling, EGFR signaling, HIF signaling and estrogen signaling as well as PI3K/Akt and Wnt/β-catenin signaling pathways. To put this in context, placental MALAT-1 is important for trophoblast invasion; its silencing in placental trophoblastic cells suppressed invasion, migration and motility through influencing CTHRC1 and CCT4 expression13,44,45. Interestingly, MALAT-1 is required for capillary formation and angiogenesis46,47,48; its knockdown markedly reduced angiogenesis by regulating VEGF, TGF-β, fibroblast growth factor-2 and tumour necrosis factor-α expressions19,46,48. Moreover, MALAT-1 modulates cell proliferation by acting as a ceRNA via interactions with miRNAs during the recurrent abortion occurrence47.
We further showed a decline in serum MALAT-1 in severe PE as well as in late-onset PE patients vs late controls, but not among early- and late-onset PE cases. Similarly, MALAT-1 underexpression was involved in severe PE within umbilical cords and MSCs from PE patients through affecting MSCs proliferation, angiogenesis, apoptosis, migration, invasion and immunosuppressive properties15. Conversely, MALAT-1 was not correlated with the onset of PE in placenta, umbilical cord and MSCs from PE patients13,15.
Interestingly, we found negative associations of MALAT-1 with maternal age and albuminuria which were in contrast with previous findings13,49,50. In fact, PE is more common in women who become pregnant at advanced maternal age51. Therefore, the decline in MALAT-1 with advanced maternal age presumably contributes to PE. Moreover, the inverse correlation between MALAT-1 and albuminuria could exacerbate PE pathology presumably through a dysregulated β-catenin/MALAT-1 axis which promotes podocyte malfunction, albuminuria and finally kidney fibrosis52. Although the correlation between MALAT-1 and GA was discrepant49,50, we found a positive correlation.
We reported a lack of association between serum HOTAIR and PE risk. Conversely, HOTAIR was upregulated in PE placenta, where it reduced cell proliferation and enhanced apoptosis by increasing caspase-314. HOTAIR was also elevated in severe PE, and altered HOTAIR was implicated in PE development53. This matches with our observed positive correlation between HOTAIR and albuminuria.
There are several limitations in our study. First, this was a case–control study in which the included patients and controls were recruited only from one hospital. Second, a modest sample size was used; however, cases were extremely filtered due to our rigorous inclusion and exclusion criteria. Third, no samples were collected before the onset of PE, and the lack of longitudinal follow up may limit the certainty of prognosis of PE from mild to severe. Finally, larger-scale predictive studies are warranted to replicate our results. Nevertheless, our data provide new clinical tools that might be implicated in genomic analysis in individualized testing with the wide availability and the technical ease of ncRNAs measurement. Future work would include establishing a normal range of the expression levels rather than using fold change to facilitate clinical application.
Conclusion
Our study accentuates miR-17, miR-363 and MALAT-1 as potential new biomarkers for PE and its severity. miR-363 was associated with early PE and MALAT-1 was associated with severe PE. By functional analysis, miR-17, miR-363 and MALAT-1 could interplay in PE pathogenesis through common targets and signaling pathways. Our data appraise the progresses in finding new biomarkers for diagnosing PE and evaluating severity and onset of PE, and also highlights areas for future research.
Subjects and methods
Patients
This prospective study involved 160 Egyptian pregnant females who received routine obstetric examination at the Department of Obstetrics and Gynecology, Kasr Al-Ainy hospital, Cairo University. The study included eligible 82 pregnant females diagnosed with PE and 78 healthy normotensive age-matched pregnant women without proteinuria or any complications as the control group.
Full history taking, physical and clinical examination were done for all participants. The medical records of each participant were revised and all relevant data were used in the study, including information on risk factors, pregnancy history and perinatal outcome. PE was diagnosed as new-onset of hypertension (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg on at least 2 occasions 4 h apart after the 20th gestational week combined with new-onset proteinuria according to the guidelines of the American College of Obstetricians and Gynecologists (ACOG 2013)54. Significant protein excretion was defined as ≥ 300 mg protein/24 h-urine sample or ≥ 1+ urine dipstick testing of two random urine samples collected at least 4 h apart. Blood samples were collected after diagnosis of PE for preeclamptic women, and from normal pregnant women at admission to the maternity ward at Kasr Al-Ainy hospital between October 2017 and March 2018. Blood pressure (BP) was measured and PE was diagnosed before blood sampling. Patients with PE were subdivided based on severity of clinical symptoms to mild and severe cases. Severe PE was defined as SBP ≥ 160 mmHg and/or DBP ≥ 110 mmHg on 2 different occasions, accompanied with proteinuria (≥ 2 g/24 h or ≥ 2+ dipstick) and the presence of persistent headache, epigastric right upper quadrant abdominal pain, vomiting, elevation of uric acid, increased serum creatinine and liver enzymes, thrombocytopenia, red cell breakdown, visual impairment, swelling, shortness of breath due to pulmonary edema and IUGR54. Mild PE was defined as SBP ≥ 140 to 159 or DBP ≥ 90 to 109 mmHg in 2 different occasions, accompanied with proteinuria (≥ 300 mg to 1.99 g/24 h or ≥ 1+ dipstick)54. Early-onset PE was defined as developing clinical manifestations of PE at ≤ 34 weeks of gestation whereas cases regarded as late-onset PE if occurred > 34 gestational weeks10.
BP was measured at admission for controls and PE patients. We expressed gestational weeks as gestational age (GA) to define the pregnancy weeks using ultrasound imaging for fetal measurements. GA was measured and recorded for every patient at admission and before blood sampling. IUGR was defined as weight below the 10th percentile for the GA as measured by an ultrasound device. BMI was defined as the body mass divided by the square of the body height, and was expressed in units of kg/m2. BMI was determined using the mother’s body weight at the time of inclusion. Blood samples were collected between 20 and 40 weeks of gestation.
Inclusion criteria were pregnant females from 20 to 40 gestational weeks and none of these subjects had any invasive procedure. Women with pre-existing hypertension, hemostatic abnormalities, cancer, twin pregnancy, intrauterine fetal death, gestational diabetes, and cardiovascular, autoimmune, renal and hepatic diseases were excluded.
All participants signed an informed consent and all experiments were approved by the ethical committee of the Faculty of Pharmacy, Cairo University, Cairo, Egypt (BC2074). All methods were carried out in accordance with guidelines and regulations in Helsinki declaration.
Sample collection for RNA assay
About 5 mL maternal venous blood was drawn from each participant by vein puncture and collected in a plain tube. Blood was left to clot at room temperature for 30 min and then centrifuged at 2000g for 15 min. Sediment- and hemolysis-free supernatants were quickly removed and aliquoted. Aliquots were immediately frozen at – 80 °C until RNA extraction. For analysis, serum samples were thawed once on ice and centrifuged at 3000g for 5 min to avoid the presence of any traces of red blood cells and other cellular debris which could affect the miRNAs and lncRNAs profile.
RNA extraction
Total RNA was isolated from 200 µL serum using the miRNeasy Serum/Plasma kit (Qiagen, Germany) following the manufacturer's instructions. Total RNA concentration and purity were analyzed using Bioanalyzer Agilent RNA 6000 picoassay. RNA was used for detection of miRNAs and lncRNAs.
miRNAs assay using RT-qPCR
Briefly, 0.1 μg of total RNA was reverse transcribed using the miScript II RT kit (Qiagen) in a total 20 µL reaction volume according to the manufacturer's instructions. The thermal parameters were 60 min at 37 °C and 5 min at 95 °C. Quantitative real-time PCR was then performed in a total 20 µL reaction volume on Rotorgene Q system (Qiagen) using the miScript SYBR Green PCR kit (Qiagen) and the provided miScript Universal Primer (reverse primer) and specific primers (forward primers) for hsa-miR-17-5p, hsa-miR-363-3p as well as SNORD68 as the internal control according to the manufacturer’s instructions. Briefly, real-time PCR was conducted in 20 µL reaction mixtures where 2.5 μL of appropriately diluted cDNA template was mixed with 5.5 μL RNase free water, 10 μL miScript SYBR Green PCR Master Mix and 2 μL miScript forward and reverse primers. The PCR thermal conditions were 15 min at 95 °C, 40 cycles of 15 s at 94 °C followed by 30 s at 55 °C and 30 s at 70 °C.
lncRNAs assay using RT-qPCR
Reverse transcription (RT) was conducted on 0.1 μg of total RNA in a 20 µL RT reaction with the high capacity cDNA Reverse Transcriptase kit (Applied Biosystems, USA) following the manufacturer’s instructions. The thermal cycler conditions were as follows: 10 min at 25 °C, 110 min at 37 °C, and 5 s at 95 °C. Expression levels of HOTAIR and MALAT-1 were evaluated by qPCR using GAPDH as the housekeeping gene. Customized primers and the Maxima SYBR Green PCR kit (ThermoFischer, USA) were used to prepare the PCR master mixture following the manufacturer’s protocol. The primer sequences were HOTAIR-forward 5′-GGTAGAAAAAGCAACCACGAAGC-3′, HOTAIR-reverse 5′-ACATAAACCTCTGTCTGTGAGTGCC-3′, MALAT-1-forward 5′-AAAGCAAGGT-CTCCCCACAAG-3′, MALAT-1-reverse 5′-GGTCTGTGCTAGATCAAAAGGCA-3′, GAPDH-forward 5′-GAAGGTCGGAGTCAACGGATT-3′, and GAPDH-reverse 5′-CGCTCCTGGAAGATGGTGAT-3′. Primer specificity was checked using the NCBI Primer-BLAST tool (https://www.ncbi.nlm.nih.gov/tools/primer-blast/). Real-time PCR was performed on Rotorgene Q system (Qiagen) in 20 µL reaction mixtures with the following conditions: 95 °C for 10 min, followed by 40 cycles at 95 °C for 15 s and 60 °C for 60 s.
Expression analysis of miRNAs and lncRNAs relative to internal control were done using 2−ΔCt method, where ΔCt = Ctgene − Ctinternal control. Fold change was calculated with the formula 2−∆∆Ct, where ∆∆Ct = ΔCtpatient − ΔCtcontrol group.
Selection of lncRNAs and miRNAs using bioinformatics analysis
Selection of PE-associated lncRNAs
We used the lncRNA disease database (http://www.cuilab.cn/lncrnadisease) to screen for PE-associated lncRNAs. Seven candidate lncRNAs were revealed (H19, MALAT-1, HOTAIR, LOC391533, LOC284100, CEACAMP8 and SPRY4-IT1) (Supplementary Table S1). Using PubMed search (http://www.ncbi.nlm.nih.gov/pubmed/), MALAT-1 and HOTAIR were selected for this study based on their biological relevance to PE13,14.
Selection of PE-associated miRNAs
PE-associated miRNAs were screened using the Human microRNA Disease Database (HMDD) v3.2 (https://www.cuilab.cn/hmdd). More than 95 different miRNAs were recorded in relation with PE. Members of miR-17-92 family, namely miR-17, miR-18a and miR-20a and members of its paralog 106a-363 cluster, namely miR-106a, miR-18b, miR-20b and miR-363 were PE candidates (Supplementary Table S2).
miRNA-lncRNA interaction analysis
The starBase platform (http://starbase.sysu.edu.cn/) was used to check the interaction between candidate miRNAs and the lncRNAs; MALAT-1 and HOTAIR. Some of the results are shown in supplementary Table S3. The database reported interactions of HOTAIR with miR-17-5p, miR-20a-5p, miR-20b-5p and miR-106a-5p as well as interactions of MALAT-1 with miR-17-5p, miR-20a-5p, miR-363-3p, miR-20b-5p and miR-106a-5p. To filter these data, we searched the PubMed for experimentally validated lncRNA-miRNAs interactions. We found previously reported direct interactions between MALAT-1 and miR-17-5p17, MALAT-1 and miR-363-3p55, and HOTAIR and miR-17-5p18 based on a reporter assay. Thus, MALAT-1, HOTAIR, miR-17-5p and miR-363-3p were selected for this study.
Target gene analysis and construction of protein–protein interaction networks
For miRNAs, the online databases, TargetScan (http://www.targetscan.org/vert_72/) and miRDB (http://mirdb.org/), were used to find the predicted target genes for the miR-17 and miR-363. For lncRNAs, the starBase platform (http://starbase.sysu.edu.cn/) was used to screen the candidate lncRNA-RNA interactions. We filtered the output by selecting protein-coding genes.
Target genes were then analyzed using CapitalBio Molecule Annotation System 3.0 software to determine the biological roles of the lncRNA and miRNA-target protein-coding genes. Finally, the genes most related to PE pathogenesis in terms of biological process, molecular function and KEGG pathways were selected. The cutoff P value was 0.05.
We analyzed the relationships between the proteins (protein–protein interaction, PPI) encoded by the genes related to the selected ncRNAs (miR-17, miR-363 and MALAT-1) using STRING online software. We also used the STRING online software to conduct functional enrichments; GO and KEGG pathways to determine the involvement of each PPI in different biological pathways related to PE. The Pathway Studio Online Software was used to visualize the PPI network related to each selected placental-related ncRNA.
Statistical analysis
Values are presented as mean ± SD, median (25%–75% percentiles), or number (percentage) when appropriate. Shapiro Wilk and Klomogrov Simirnov normality tests were used to check data normality. Data were compared using the parametric Student’s t test or the non-parametric Mann—Whitney U test when appropriate. The examined miRNAs, lncRNAs and CRP data were not normally distributed and their levels were compared by applying the Mann—Whitney U test. Fischer exact test was used to compare the categorical data. Receiver-operating-characteristic (ROC) analysis was carried out to evaluate the diagnostic and prognostic accuracy of molecular data. Area under the curve (AUC) < 0.6 was considered as non-significant, AUC ≥ 0.6 and < 0.7 as significant discriminator, AUC ≥ 0.7 and < 0.9 as potential discriminator, and AUC ≥ 0.9 as excellent discriminator. The associations between the biomarkers, early PE risk and PE severity were investigated using univariate followed by stepwise forward multivariate logistic regression analyses. Correlations between parameters were identified using Spearman correlation. Statistical significance was considered at P < 0.05. Statistical analyses were carried out using SPSS software v15 for Microsoft Windows (SPSS, Chicago, IL) and GraphPad Prism 7.0 (GraphPad Software, CA, USA).
Ethics approval
(a) All experiments were approved by the ethical committee of the Faculty of Pharmacy, Cairo University, Cairo, Egypt (BC2074). (b) All methods were carried out in accordance with guidelines and regulations in Helsinki declaration.
Data availability
The data that supports the findings of this study are available in the manuscript and in the supplementary material of this article.
References
Mayrink, J., Costa, M. L. & Cecatti, J. G. Preeclampsia in 2018: Revisiting concepts, physiopathology and prediction. Sci. World J. 2018, 6268276 (2018).
Kaaja, R. J. & Greer, I. A. Manifestations of chronic disease during pregnancy. JAMA 294, 2751–2757 (2005).
Mosca, L. et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women-2011 update: A guideline from the American Heart Association. Circulation 123, 1243–1262 (2011).
Young, B. C., Levine, R. J. & Karumanchi, S. A. Pathogenesis of preeclampsia. Annu. Rev. Pathol. 5, 173–192 (2010).
Bounds, K. R., Chiasson, V. L., Pan, L. J., Gupta, S. & Chatterjee, P. MicroRNAs: New players in the pathobiology of preeclampsia. Front. Cardiovasc. Med. 4, 60 (2017).
McAninch, D., Roberts, C. T. & Bianco-Miotto, T. Mechanistic insight into long noncoding RNAs and the placenta. Int. J. Mol. Sci. 18, 1731 (2017).
Sandrim, V. C., Luizon, M. R., Palei, A. C., Tanus-Santos, J. E. & Cavallie, R. C. Circulating microRNA expression profiles in pre-eclampsia: Evidence of increased miR-885-5p levels. BJOG. Int. J. Obstet. Gynaecol. 123, 2120–2128 (2016).
He, X. et al. LncRNAs expression in preeclampsia placenta reveals the potential role of lncRNAs contributing to preeclampsia pathogenesis. PLoS ONE 8, 1–6 (2013).
Xu, P. et al. Variations of microRNAs in human placentas and plasma from preeclamptic pregnancy. Hypertension 63, 1276–1284 (2014).
Luque, A. et al. Usefulness of circulating microRNAs for the prediction of early preeclampsia at first-trimester of pregnancy. Sci. Rep. 4, 1–8 (2014).
Wang, W. et al. Preeclampsia up-regulates angiogenesis-associated microRNA (i.e., miR-17, -20a, and -20b) that target ephrin-B2 and EPHB4 in human placenta. J. Clin. Endocrinol. Metab. 97, 1051–1059 (2012).
Kumar, P., Luo, Y., Tudela, C., Alexander, J. M. & Mendelson, C. R. The c-Myc-regulated microRNA-17∼92 (miR-17∼92) and miR-106a∼363 clusters target hCYP19A1 and hGCM1 to inhibit human trophoblast differentiation. Mol. Cell Biol. 33, 1782–1796 (2013).
Chen, H. et al. Long non-coding RNA MALAT-1 is downregulated in preeclampsia and regulates proliferation, apoptosis, migration and invasion of JEG-3 trophoblast cells. Int. J. Clin. Exp. Pathol. 8, 12718–12727 (2015).
Zou, Y. F. & Sun, L. Z. Long noncoding RNA HOTAIR modulates the function of trophoblast cells in pre-eclampsia. Sichuan Da Xue Xue Bao Yi Xue Ban. 46, 113–117, 122 (2015).
Li, X. et al. Long non-coding RNA MALAT1 promotes proliferation, angiogenesis and immunosuppressive properties of mesenchymal stem cells by inducing VEGF and IDO. J. Cell Biochem. 118, 2780–2791 (2017).
Kim, H. J. et al. Long non-coding RNA HOTAIR is associated with human cervical cancer progression. Int. J. Oncol. 46, 521–530 (2015).
Xu, Y. et al. Casiopeina II-gly acts on lncRNA MALAT1 by miR-17-5p to inhibit FZD2 expression via the Wnt signaling pathway during the treatment of cervical carcinoma. Oncol. Rep. 42, 1365–1379 (2019).
Wei, B., Wei, W., Zhao, B., Guo, X. & Liu, S. Long non-coding RNA HOTAIR inhibits mir-17-5p to regulate osteogenic differentiation and proliferation in nontraumatic osteonecrosis of femoral head. PLoS ONE 12, 1–14 (2017).
Aiello, A. et al. MALAT1 and HOTAIR long non-coding RNAs play opposite role in estrogen-mediated transcriptional regulation in prostate cancer cells. Sci. Rep. 6, 1–11 (2016).
Liu, H. et al. Long non-coding RNA MALAT1 mediates hypoxia-induced pro-survival autophagy of endometrial stromal cells in endometriosis. J. Cell Mol. Med. 23, 439–452 (2019).
Hong, Q. et al. LncRNA HOTAIR regulates HIF-1alpha;/AXL signaling through inhibition of miR-217 in renal cell carcinoma. Cell Death Dis. 8, 1–9 (2017).
Hromadnikova, I., Kotlabova, K., Dvorakova, L. & Krofta, L. Postpartum profiling of microRNAs involved in pathogenesis of cardiovascular/cerebrovascular diseases in women exposed to pregnancy-related complications. Int. J. Cardiol. 291, 158–167 (2019).
Wang, Y. et al. Aberrantly up-regulated miR-20a in pre-eclampsic placenta compromised the proliferative and invasive behaviors of trophoblast cells by targeting forkhead box protein A1. Int. J. Biol. Sci. 10, 973–982 (2014).
Hromadnikova, I., Kotlabova, K., Hympanova, L. & Krofta, L. Cardiovascular and cerebrovascular disease associated microRNAS are dysregulated in placental tissues affected with gestational hypertension, preeclampsia and intrauterine growth restriction. PLoS ONE 10, 1–27 (2015).
Hromadnikova, I., Kotlabova, K., Hympanova, L. & Krofta, L. Gestational hypertension, preeclampsia and intrauterine growth restriction induce dysregulation of cardiovascular and cerebrovascular disease associated microRNAs in maternal whole peripheral blood. Thromb. Res. 137, 126–140 (2016).
Du, W. et al. By targeting Stat3 microRNA-17-5p promotes cardiomyocyte apoptosis in response to ischemia followed by reperfusion. Cell Physiol. Biochem. 34, 955–965 (2014).
Mendell, J. T. MiRiad roles for the miR-17-92 cluster in development and disease. Cell 133, 217–222 (2008).
Wang, Q. et al. MiR-17-92 cluster accelerates adipocyte differentiation by negatively regulating tumor-suppressor Rb2/p130. Proc. Natl. Acad. Sci. USA. 105, 2889–2894 (2008).
Spradley, F. T., Palei, A. C. & Granger, J. P. Increased risk for the development of preeclampsia in obese pregnancies: Weighing in on the mechanisms. Am. J. Physiol. Regul. Integr. Comp. Physiol. 309, R1326–R1343 (2015).
Su, L., Zhao, S., Zhu, M. & Yu, M. Differential expression of microRNAs in porcine placentas on days 30 and 90 of gestation. Reprod. Fertil. Dev. 22, 1175–1182 (2010).
Gu, Y., Sun, J., Groome, L. J. & Wang, Y. Differential miRNA expression profiles between the first and third trimester human placentas. Am. J. Physiol. Endocrinol. Metab. 304, 836–843 (2013).
Roy, H., Bhardwaj, S. & Ylä-Herttuala, S. Biology of vascular endothelial growth factors. FEBS Lett. 580(12), 2879–2887 (2006).
Li, J. et al. The role, mechanism and potentially novel biomarker of microRNA-17-92 cluster in macrosomia. Sci. Rep. 5, 1–11 (2015).
Wommack, J. C., Trzeciakowski, J. P., Miranda, R. C., Stowe, R. P. & Ruiz, R. J. Micro RNA clusters in maternal plasma are associated with preterm birth and infant outcomes. PLoS ONE 13, 1–13 (2018).
Zhu, Y. et al. Profiling maternal plasma microRNA expression in early pregnancy to predict gestational diabetes mellitus. Int. J. Gynecol. Obstet. 130, 49–53 (2015).
Zhu, X., Han, T., Sargent, I. L., Yin, G. & Yao, Y. Differential expression profile of microRNAs in human placentas from preeclamptic pregnancies vs normal pregnancies. Am. J. Obstet. Gynecol. 200(661), e1-661.e7 (2009).
Zhang, C. et al. Placental miR-106a∼363 cluster is dysregulated in preeclamptic placenta. Placenta 36, 250–252 (2015).
Li, Q. et al. Quantification of preeclampsia-related microRNAs in maternal serum. Biomed. Rep. 3, 792–796 (2015).
Thamotharan, S. et al. Differential microRNA expression in human placentas of term intra-uterine growth restriction that regulates target genes mediating angiogenesis and amino acid transport. PLoS ONE 12, 1–26 (2017).
Lang, X. et al. The role of NUDT21 in microRNA-binging sites of EZH2 gene increases the of risk preeclampsia. J. Cell Mol. Med. 23, 3202–3213 (2019).
Herzog, E. M. et al. Impact of early- and late-onset preeclampsia on features of placental and newborn vascular health. Placenta 49, 72–79 (2017).
Chen, L. et al. A novel negative regulator of adipogenesis: MicroRNA-363. Stem Cells. 32, 510–520 (2014).
Yang, X. & Meng, T. Long noncoding RNA in preeclampsia: Transcriptional noise or innovative Indicators?. Biomed. Res. Int. 2019, 5437621 (2019).
Tseng, J. J., Hsieh, Y. T., Hsu, S. L. & Chou, M. M. Metastasis associated lung adenocarcinoma transcript 1 is up-regulated in placenta previa increta/percreta and strongly associated with trophoblast-like cell invasion in vitro. Mol. Hum. Reprod. 15, 725–731 (2009).
Tano, K. et al. MALAT-1 enhances cell motility of lung adenocarcinoma cells by influencing the expression of motility-related genes. FEBS Lett. 584, 4575–4580 (2010).
Singh, K. K. et al. Investigation of TGF beta1-induced long noncoding RNAs in endothelial cells. Int. J. Vasc. Med. 2016, 2459687 (2016).
Wang, Y. et al. Downregulated MALAT1 relates to recurrent pregnancy loss via sponging miRNAs. Kaohsiung J. Med. Sci. 34, 503–510 (2018).
Liu, J. Y. et al. Pathogenic role of lncRNA-MALAT1 in endothelial cell dysfunction in diabetes mellitus. Cell Death Dis. 5, e1506 (2014).
Fouad, N. A. et al. Diagnostic potential of metastasis-associated-lung-adenocarcinoma-transcript-1 (MALAT-1) and TNFα and hnRNPL related immunoregulatory long non-coding RNA (THRIL) in systemic lupus erythematosus patients: Relation to disease activity. Egypt Rheumatol. 41, 197–201 (2019).
Azari, I. et al. Expression of long non-coding RNAs in placentas of intrauterine growth restriction (IUGR) pregnancies. Rep. Biochem. Mol. Biol. 8, 25–31 (2019).
Arulkumaran, N. & Lightstone, L. Severe pre-eclampsia and hypertensive crises. Best Pract. Res. Clin. Obstet. Gynaecol. 27, 877–884 (2013).
Hu, M. et al. LncRNA MALAT1 is dysregulated in diabetic nephropathy and involved in high glucose-induced podocyte injury via its interplay with β-catenin. J. Cell Mol. Med. 21, 2732–2747 (2013).
Mohammadpour-Gharehbagh, A. et al. Impact of HOTAIR variants on preeclampsia susceptibility based on blood and placenta and in silico analysis. IUBMB Life 71, 1367–1381 (2019).
American College of Obstetricians and Gynecologists, Task Force on hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on hypertension in pregnancy. Obstet. Gynecol. 122(5), 1122–1131 (2013).
Wang, S. H. et al. The lncRNA MALAT1 functions as a competing endogenous RNA to regulate MCL-1 expression by sponging miR-363-3p in gallbladder cancer. J. Cell Mol. Med. 20, 2299–2308 (2016).
Acknowledgements
We acknowledge Dr. Eman A. Hussein, MD, Obstetrics and Gynecology for her help in samples collection and Dr. Ahmed A. Hussein, MD, Urology for his guidance in references management.
Funding
This work was partially supported by the research fund of the Faculty of Pharmacy, Cairo University. We didn’t receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
S.A.A. conceived and supervised the study. S.A.A., O.G.S. and M.A.S. designed the study. O.G.S., M.A.S. and Y.A.H.A. conducted the practical experiments. Y.A.H.A. collected the samples and provided the analysis tools. M.A.S. and Y.A.H.A. carried out the statistical and data analysis and wrote the paper. All authors revised and approved the final paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelazim, S.A., Shaker, O.G., Aly, Y.A.H. et al. Uncovering serum placental-related non-coding RNAs as possible biomarkers of preeclampsia risk, onset and severity revealed MALAT-1, miR-363 and miR-17. Sci Rep 12, 1249 (2022). https://doi.org/10.1038/s41598-022-05119-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05119-9
This article is cited by
-
Are Vascular Endothelium and Angiogenesis Effective MicroRNA Biomarkers Associated with the Prediction of Early-Onset Preeclampsia (EOPE) and Adverse Perinatal Outcomes?
Reproductive Sciences (2024)
-
Association of LncRNA-PAX8-AS1 and LAIR-2 polymorphisms along with their expression with clinical and subclinical hypothyroidism
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.