Until now, the connections between diabetes distress and psychological stress have been minimally researched.
In a UCI-led study published as the Feature Article in Diabetes Spectrum on Jan. 7, researchers found that people with type II diabetes who reported any measure of unmet psychological needs were at a high risk of negative health outcomes.
Type II diabetes patients with psychological stress encountered a 20-percent higher risk of incurring annual medical expenditures more than $7,000, a 73-percent increased risk of visiting the emergency department for any reason, and they were 58-percent more likely to report diabetes-related complications. The patients were also 2.45 times more likely to experience an inpatient stay and seven times more likely to experience all-cause mortality compared to those not reporting unmet psychological distress.
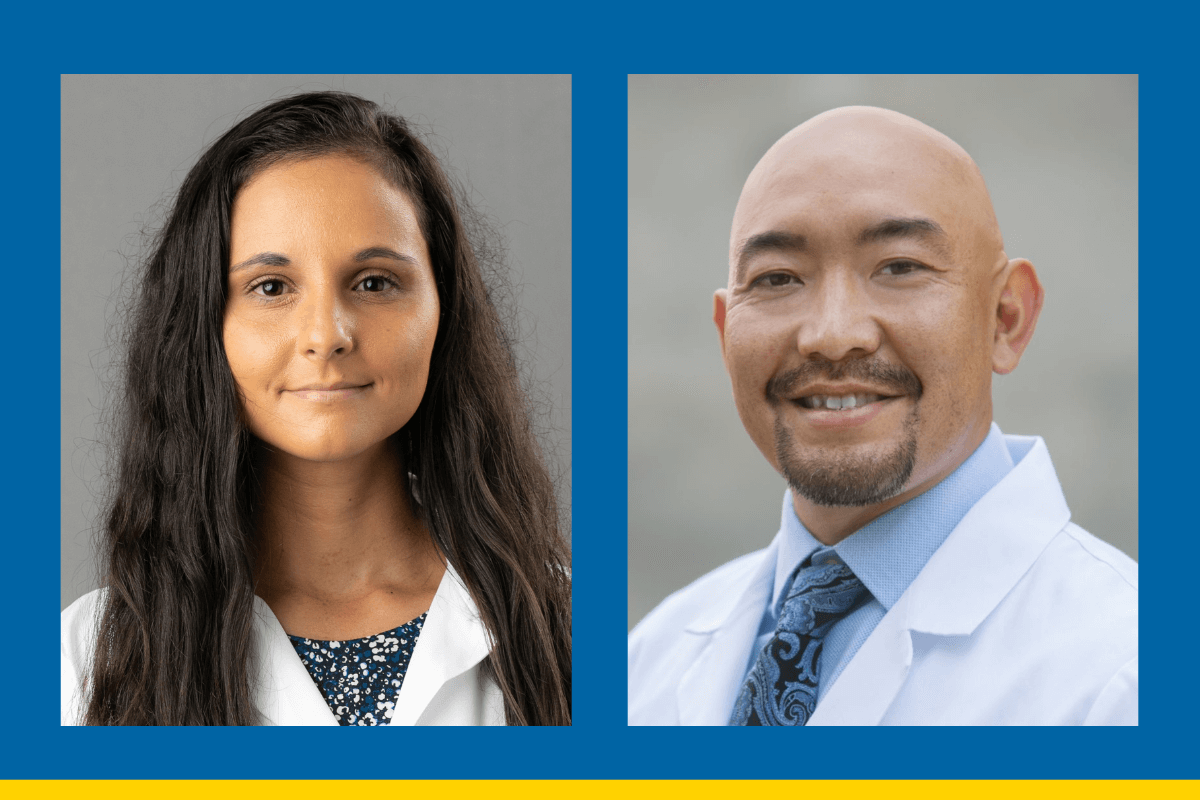
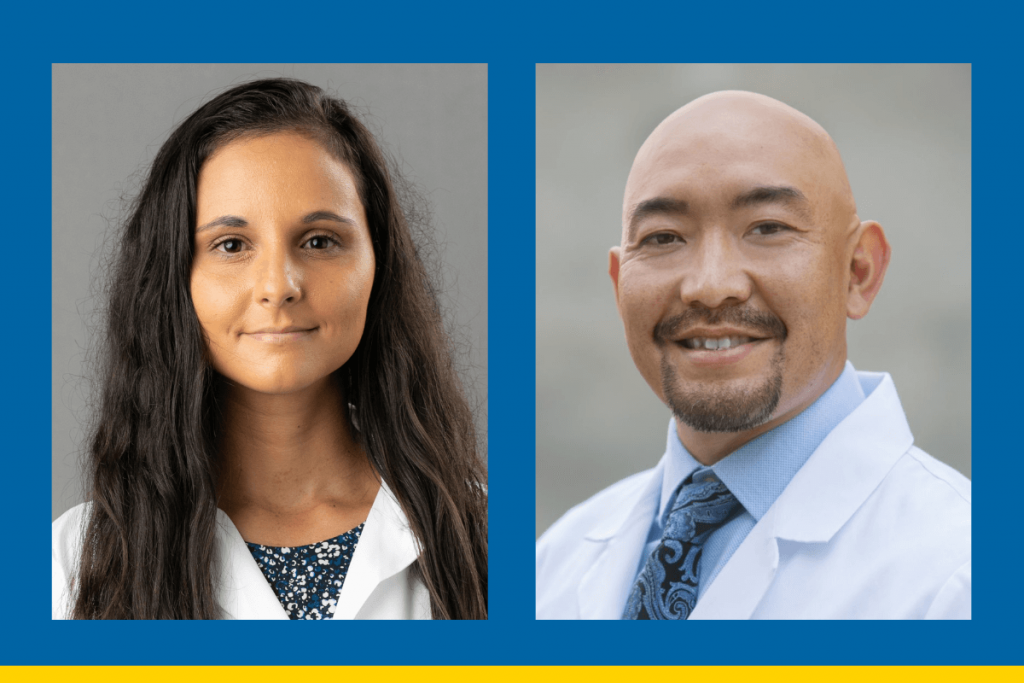
The research study was a culmination of a robust, interdisciplinary project involving UCI and UC San Diego faculty, including lead author UCI Assistant Professor of Clinical Pharmacy Aryana Sepassi, PharmD, and senior author UCI Professor of Clinical Pharmacy Jonathan Watanabe, PharmD, PhD.
“Diabetes distress and psychological stress placed on people with type II diabetes has important ramifications on well-being and healthcare resource utilization,” Sepassi said. “Being able to identify and address psychological needs regularly is of crucial importance in people with type II diabetes. In doing so, as healthcare providers, we might be able to mitigate some of these debilitating outcomes using cost-effective methods.”
For Sepassi and the research team, the next step is to develop and implement interventions that better facilitate communication between people with type II diabetes and their primary care providers regarding mental health is of the utmost importance.
A member of the research team, UC San Diego’s Renu Singh, PharmD, is the co-founder of the Diabetes Management and Education Clinic at UCSD Health primary care clinics and she provides direct care to patients with diabetes.
“If we – as healthcare professionals – are able to establish these interventions,” Sepassi said, “we might be able to prevent significant morbidity and mortality in our patients.”
In addition to Sepassi, Watanabe, and Singh, the research team also included UCSD faculty Mark Bounthavong, PharmD, PhD, and Kristin Beizai, MD, along with Mark Heyman, PhD, from the Center for Diabetes & Mental Health.
“This collaborative research effort shed light on an understudied, but immensely important aspect of diabetes care that succeeded because of its interdisciplinary, team-science approach,” Watanabe said.