Abstract
Objective
To study the relationship of body fat distribution in patients with diabetes mellitus (DM), and its long-term complications like diabetic retinopathy (DR), in Indian population.
Methods
This was a prospective, cross-sectional observational study involving 1773 subjects diagnosed with DM and 1778 age and gender-matched individuals. The patients with DM were assessed for the presence and severity of DR. Severe non-proliferative DR and proliferative DR were categorised as sight threatening DR (STDR). Anthropometric parameters, i.e., neck circumference (NC); mid-upper arm circumference (MAC); waist circumference (WC); hip circumference (HC); mid-thigh circumference (MTC) and body mass index (BMI) were measured using standardised technique.
Results
The mean age was 59.33 ± 9.32 for DM group, and 66.03 ± 11.04 for non-DM group. DM group showed significantly greater NC, WC, and MTC and significantly reduced MAC and weight. HC and BMI were comparable between the groups. There was a significant positive correlation of MAC and WC (with any level of DR) and MAC, WC, and weight (for STDR); and a significant negative correlation of HC and MTC (with any level of DR) and NC, HC, MTC, and BMI (for STDR). Multiple logistic regression analysis confirmed that WC was the single most important predictor for any level of DR and STDR.
Conclusions
Association of body fat distribution with DM and DR appears multifactorial. However, central obesity signified by waist circumference appears to be the significant risk related to the development of DR and STDR in Indian population.
Similar content being viewed by others
Introduction
The increased prevalence of diabetes mellitus (DM) worldwide has lead diabetic retinopathy (DR) as the leading cause of visual impairment in working-age individuals [1,2,3]. The longer duration and poor glycaemic control along with blood pressure fluctuations have been established as primary risk factors responsible for the development and progression of DR in various population-based studies [4]. However, recent evidence indicates that proper glycaemic and blood pressure control may not be sufficient to reduce the risk of DR [5, 6]. Furthermore, as undiagnosed hyperglycaemia may precede the diagnosis of DM by many years, a significant number of patients already have lesions of DR in one or both eyes at the time of presentation [7, 8]. Hence it becomes imperative to understand the role of other modifiable risk factors in the development and progression of DR, and obesity is one such important factor [9].
There is adequate evidence in the literature suggesting the distribution of body fat as an important risk factor for the development of type 2 DM [10,11,12,13,14]. Body mass index (BMI) is generally used as an index to screen obesity, or to be specific, generalised obesity [15], whereas waist circumference (WC) are used as indicators of abdominal or central obesity [16]. Waist-line adipose tissue has been found to have a much higher correlation to metabolic syndrome as compared with BMI [17]. Subjects with greater mid-thigh circumference (MTC) are known to have better glucose tolerance, suggesting a protective role of fat accumulation in the thigh region [18,19,20]. Neck circumference (NC) with peripheral fat accumulation, on the other hand, has been reported to have a positive correlation with insulin resistance [21]. In diabetic patients, mid-arm circumference (MAC) has been shown to have a good correlation with central obesity and insulin resistance [22]. However, although BMI is known as the frontline obesity risk factor related to DM and its complications, investigators analysing the relationship between the BMI and DR have reported conflicting results, with some suggesting an increased risk of DR with higher BMI [23,24,25,26], whereas others suggest a protective role [27,28,29,30]. These differences may stem from the ethnic variations, inadequate sample size, or gender based variations [31]. Similarly, WC has been noted to increase the risk of DR [32].
South Asians have a predisposition for abdominal obesity characterised by increased WC in spite of low BMI [33, 34]. Man et al. reported a protective role of BMI for DR in the Singaporean population. However, they reported an increased risk of DR with higher waist-hip ratio (WHR) values in women [35]. WC is reported to signify central obesity better than WHR (being a ratio) [36], and studies have reported a higher risk of DR with higher WC [32]. A study by Hwang et al. in the Korean population showed that patients with higher BMI, larger WC, and higher total body fat were less likely to develop vision-threatening DR, signifying a possible protective role in that population [37]. This heterogeneity in the reported significance of these obesity parameters in different populations stems from various factors like ethnic variations, duration of DM, and gender variations.
Recent population-based studies on multiple ethnicities in Asian (including Indian) populations have reported a protective role of BMI on DR, as well as sight-threatening DR (STDR) [38, 39]. A study by Raman et al. suggested a protective role of high BMI and combined obesity for any level of DR in the Indian population [29]. Rajalakshmi et al. reported an increased risk of developing DR with high WC in type 1 DM [40]. Similarly, Sen et al. concluded a high risk of developing DR with elevated C-reactive protein levels, but not with BMI [41]. In short, even though ethnicity is an important factor in associating obesity with DR, there is a great deal of disparity in the results even within the same populations. Our study was conducted to explore the association of obesity pattern with DM and to further explore the association with STDR in the Indian population.
Methods
Study population
This was a cross-sectional, observational, institutional review board approved study conducted at Military hospitals (Jammu, Yol and Pathankot) over a period of 5 years from January 2015 through December 2019. All the patients with type 2 DM coming to our clinics for ophthalmic evaluation were included in this study. Age and gender-matched patients with no history of diabetes or other systemic diseases were included as a control group. Written informed consent was acquired prior to enrolment into the study. This study adhered to the tenets of the Declaration of Helsinki.
All the patients were diagnosed with DM based on the history, fasting blood sugar (≥126 mg/dl) and post-prandial (≥200 mg/dl); and glycosylated haemoglobin (HbA1c ≥ 6.5%) [42]. The data about the duration of DM and the presence and/or severity of DR was also acquired as detailed later.
Major exclusion criteria
All patients who had other concomitant systemic diseases, like hypertension and coronary artery disease, were excluded. We also excluded patients with endocrine disorders, malnutrition, and history of steroid intake and outside of the 18–90 years age range. Any patient with congenital or accidental limb/muscle deformity was excluded. We also excluded all patients who have had ophthalmic treatment in the form of laser, intravitreal injections, or vitrectomy.
Ophthalmic evaluation
After a detailed general and ophthalmic history, a thorough ophthalmic evaluation was performed. Best-corrected visual acuity was estimated using Snellen’s chart. A slit lamp evaluation of the anterior segment, followed by intraocular pressure measurement with Goldmann applanation tonometry, and dilated fundus evaluation with indirect ophthalmoscope to assess the DR staging (using Diabetic Retinopathy Severity Scale) was done. Any grade which was severe non-proliferative DR or beyond was considered as STDR.
Anthropometric measurements
The following anthropometric measurements were obtained using standardised techniques: [23, 43] NC; mid-upper arm circumference (MAC); WC; hip circumference (HC); MTC; height; weight; and BMI. These measurements were acquired following WHO standards by the same investigator three times, and an average value was considered for analysis. Weight was measured with a digital scale kept on a firm horizontal surface, recorded to the nearest 100 gm, with subjects wearing light clothing and no footwear. Remaining measurements were recorded using a non-stretchable measuring tape. Height was measured to the nearest 1 cm with subjects standing without shoes with their back against the wall using stadiometer, heels together and eyes directed forward. BMI was calculated by using the formula: weight (kg)/height (m)2. WC was measured at the mid-point between lowest palpable rib and iliac crest in standing position at the end of tidal expiration. HC was taken as the greatest circumference of the buttocks. NC (cm) was measured to the nearest 1 mm and was measured from the level just below the laryngeal prominence perpendicular to the long axis of the neck with the head positioned in the horizontal plane. MAC was measured in the dominant upper arm, measured at the mid-point between the tip of the shoulder and the tip of the elbow (olecranon process and the acromion). Mid-thigh was designated as the mid-point of the distance between the anterior superior iliac spine of the hip bone and the medial condyle of the femur in both legs, and average values were recorded.
Sample size calculation
Sample size was calculated by using mean and standard deviation (SD) of WC from the previous hospital data for diabetic and non-diabetic patients:
n is the sample size (for BWT comparison); Zα is the standard normal variate for α = 0.05 (95% CI) = 1.96; Z1−β is the standard normal variate for 1 − β = 0.80 (80%) = 0.84; SD = 8.80; Effective size = d = 0.85.
Using this, the minimum required sample size calculated was 1680 per group.
Over the duration of study period, we selected 1773 patients in the study group and 1778 patients in the control group.
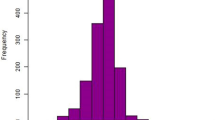
Statistical analysis
Data analysis was performed by using SPSS (Statistical Package for social Sciences) version 25.0. Qualitative data variables were expressed as frequency and percentage (%), whereas quantitative data variables were expressed as mean ± SD. The normality of the data was checked by one-sample Kolmogorov–Smirnov test. As the data were normally distributed, independent sample t-test was performed to test the difference between DM and control groups as well as males and females in the group with DM. Binary logistic regression analysis was used to obtain the association between different obesity indices and DR, after adjusting for age, gender, HbA1c, and diabetes duration. A p value < 0.05 was considered statistically significant.
Results
This study included 1773 consecutive subjects of Indian ethnicity with type 2 DM coming to our clinic for ophthalmic evaluation. An additional age and gender-matched 1778 patients with no history of diabetes were included as a control group. Out of these, 806 (45.5%) were females. The age range (mean ± SD) of the study cohort was 66 ± 11 years. The duration of diabetes ranged from 8.05 ± 5.6 years. HbA1c ranged from 6.8 ± 1.7%. The distribution of severity of DR in the study cohort was as follows: No DR (N = 894, 50.5%); mild NPDR (N = 243, 13.7%), moderate NPDR (N = 201, 11.3%), severe NPDR (N = 222, 12.5%), PDR (N = 213, 12%). We also included 1778 age and gender-matched subjects with no history of diabetes over the same duration as a control group.
Table 1 compares the characteristics and the anthropometric data between the DM and the control group. The patients with DM showed significantly greater NC, WC, and MTC and significantly reduced MAC and weight. HC and BMI were comparable between the groups. The anthropometric data which were significantly associated with any DR are summarised in Table 2: it shows that mid-arm and WC were significantly greater, and hip and MTC were significantly reduced between the group with any level of DR (N = 879) and the group without (N = 894). Rest of the data were comparable between the two groups. Table 3 summarises the factors significantly associated with STDR, which were: MAC, WC, and weight (positive association); and NC, HC, MTC, and BMI (negative association).
Multiple logistic regression analysis confirmed that WC was the single most important predictor for any level of DR and STDR in our study population (when adjusted for age, gender, duration, and HbA1c levels).
Discussion
The results in our study showed that patients with diabetes showed a significantly greater NC, WC, and MTC, and reduced MAC as well as weight as compared to the control group. BMI and HC, however, were comparable between the two groups. Distribution of body fat and obesity are known as a powerful and modifiable risk factors for DM [44]. BMI, in particular, has been associated with increased risk of DM in various population-based studies [45]. But this may not hold true in all studies as apart from gender [46] and ethnic [47] variations, researchers have shown that the effect of BMI on DM diminishes with age [48]. Moreover, some researchers have questioned the significance of BMI alone as an indicator of obesity, and therefore, other parameters need to be analysed [49]. Our results are in agreement with various studies, which suggest that it is not only BMI, but an interplay of various metabolic factors, including weight loss, which is more important in determining the risk of DM progression [50,51,52,53]. As other studies have reported WC to be an important predictor for DM development even in patients with normal or low BMI, the results of our study become significant [16, 54, 55]. MTC was strongly associated with DM in our study, in contrast to various others where it has been reported to have a negative correlation to the development of DM [55, 56]. The authors advocate caution at this juncture that although it is the distribution of body fat in various organs resulting in multiple parameters being significant in different studies, WC has been proposed as the single most crucial factor predicting obesity and its relation to metabolic diseases, including DM, and as a measure of central obesity, especially in the Asian population, should be considered significant when assessing the risk analysis for such diseases [57].
Our study showed that mid-arm and WC were significantly greater, and hip and MTC were significantly reduced between the group with any level of DR (N = 879) and the group without (N = 894). BMI as well as NC were noted to be comparable in both groups. As BMI has been reported to have positive as well as negative correlation with DR in various studies, it is important to scrutinise this aspect here. Studies analysing the association of BMI with DR have reported confounding results [9, 58,59,60]. Studies on Indian subjects have also reported either a protective role or no role of BMI on DR [29, 40, 41]. WC has been shown to correlate well with DR in Asian populations [32, 37]. This again highlights the importance of understanding the role of central obesity. These results demonstrate that apart from the distribution of body fat based on geographic locales and ethnicities, various other factors play a role in determining the risk of development of complications like DR. Nonetheless, central obesity indicating greater proportion of fat accumulation in the abdominal area, and a lower fat accumulation in hips and thighs, should be considered when treatment strategies for these blinding diseases are being planned.
Furthermore, our study confirmed the association of multiple anthropometric data with STDR, and similar factors as associated with any level of DR were observed. In addition, a significant negative correlation with NC and BMI was identified. The conflicting reports as noted in the literature must be evaluated with caution [9, 37]. As seen with the discussion so far, anthropometric data alone may not dictate the onset and development of DM and DR [41, 49,50,51,52]. The protective role of BMI in STDR in this and other studies as mentioned previously may stem from the fact that STDR is usually seen in long-standing DM, and lipolysis is known to increase in patients with DM especially in long standing disease [61]. The long-term diabetic sequelae like neuropathy and diabetic amyotrophy with fat and muscle atrophy in peripheral limbs, especially with well controlled DM, may also result in remnant central obesity with thin extremities [62]. Our finding of increased WC as the factor most significantly associated with DR and STDR suggests that it is the central or the abdominal obesity in the Indian population which guides the risks of DR and STDR. Again, as BMI showed a protective role in STDR, it indicates that generalised obesity alone may be insufficient when analysing the risks of such metabolic diseases. We should take into consideration a multitude of factors when assessing the possible development of STDR and other complications in long-standing DM, even within similar ethnic groups [63].
This study has various strengths. The large sample size, strict exclusion criteria, standardised methods of measuring the anthropometric data are noteworthy. However, there are certain limitations. We have not considered other biochemical factors like serum leptins and C reactive proteins, which have been found to have a role in the development of DR. Also, the subjects recruited were those visiting the hospital and may not represent the whole population, with some ambiguity in results. We excluded the effect of ratios like WHR in the final analysis as, being a ratio, the results may vary depending upon the numerator or the denominator, or both. Also, as mentioned previously, WC is reported to signify central obesity better than WHR, which becomes important when assessing the obesity factors in Indian population.
To conclude, various anthropometric parameters affect the incidence of DM and its related complications like DR. Ethnic variations may not be sufficient to justify the association, as various other factors may have a role to play. Nonetheless, central obesity seems to be a substantial risk factor for the development of DR and STDR in Indian population.
Summary
What was known before
-
Obesity and distribution of body fat is an important predictor for the development of DM.
-
Very few studies have explored the role of anthropometric parameters on diabetic retinopathy.
What this study adds
-
Association of body fat distribution with the risk of developing DM and related complications like DR appears multifactorial.
-
Central obesity signified by waist circumference appears to be the significant risk related to the development of DR and STDR in Indian population.
References
Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med. 2012;366:1227–39.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pr. 2014;103:137–49.
Trento M, Passera P, Trevisan M, Schellino F, Sitia E, Albani S, et al. Quality of life, impaired vision and social role in people with diabetes: a multicenter observational study. Acta Diabetol. 2013;50:873–7.
Klein R, Klein BE. Blood pressure control and diabetic retinopathy. Br J Ophthalmol. 2002;86:365–7.
Beulens JWJ, Patel A, Vingerling JR, Cruickshank JK, Hughes AD, Stanton A, et al. Effects of blood pressure lowering and intensive glucose control on the incidence and progression of retinopathy in patients with type 2 diabetes mellitus: a randomised controlled trial. Diabetologia. 2009;52:2027–36.
Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419–30.
Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care. 1992;15:815–9.
Turner R, Cull C, Holman R. United Kingdom prospective diabetes study 17: a 9-year update of a randomized, controlled trial on the effect of improved metabolic control on complications in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996;124:136–45.
Dirani M, Xie J, Fenwick E, Benarous R, Rees G, Wong TY, et al. Are obesity and anthropometry risk factors for diabetic retinopathy? The diabetes management project. Invest Ophthalmol Vis Sci. 2011;52:4416–21.
Guasch-Ferre M, Bullo M, Martinez-Gonzalez MÁ, Corella D, Estruch R, Covas MI, et al. Waist-to-height ratio and cardiovascular risk factors in elderly individuals at high cardiovascular risk. PLoS ONE. 2012;7:e43275.
Lundgren H, Bengtsson C, Blohme G, Lapidus L, Sjostrom L. Adiposity and adipose tissue distribution in relation to incidence of diabetes in women: results from a prospective population study in Gothenburg, Sweden. Int J Obes. 1989;13:413–23.
Warne DK, Charles MA, Hanson RL, Jacobsson LTH, McCance DR, Knowler WC, et al. Comparison of body size measurements as predictors of NIDDM in Pima Indians. Diabetes Care. 1995;18:435–9.
Tulloch-Reid MK, Williams DE, Looker HC, Hanson RL, Knowler WC. Do measures of body fat distribution provide information on the risk of type 2 diabetes in addition to measures of general obesity? Comparison of anthropometric predictors of type 2 diabetes in Pima Indians. Diabetes Care. 2003;26:2556–61.
Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81:555–63.
Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117–28.
Deepa M, Farooq S, Deepa R, Manjula D, Mohan V. Prevalence and significance of generalized and central body obesity in an urban Asian Indian population in Chennai, India (CURES: 47). Eur J Clin Nutr. 2009;63:259–67.
Smith SC Jr, Haslam D. Abdominal obesity, waist circumference and cardio-metabolic risk: awareness among primary care physicians, the general population and patients at risk-the Shape of the Nations survey. Curr Med Res Opin. 2007;23:29–47.
Terry RB, Stefanick ML, Haskell WL, Wood PD. Contributions of regional adipose tissue depots to plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat. Metabolism. 1991;40:733–40.
Seidell JC, Pérusse L, Després JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr. 2001;74:315–21.
Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: the AusDiab Study. Int J Obes Relat Metab Disord. 2004;28:402–9.
Cho NH, Oh TJ, Kim KM, Choi SH, Lee JH, Park KS, et al. Neck circumference and incidence of diabetes mellitus over 10 years in the Korean Genome and Epidemiology Study (KoGES). Sci Rep. 2015;5:18565.
Zhu Y, Lin Q, Zhang Y, Deng H, Hu X, Yang X, et al. Mid-upper arm circumference as a simple tool for identifying central obesity and insulin resistance in type 2 diabetes. PLoS ONE. 2020;15:e0231308.
Katusić D, Tomić M, Jukić T, Kordić R, Sikić J, Vukojević N, et al. Obesity-a risk factor for diabetic retinopathy in type 2 diabetes? Coll Antropol. 2005;29(Suppl 1):47–50.
Zhang L, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in diabetes control and complications trial type 1 diabetic patients with good or poor metabolic control. Diabetes Care. 2001;24:1275–9.
Li X, Wang Z. Prevalence and incidence of retinopathy in elderly diabetic patients receiving early diagnosis and treatment. Exp Ther Med. 2013;5:1393–6.
De Block CE, De Leeuw IH, Van, Gaal LF. Impact of overweight on chronic microvascular complications in type 1 diabetic patients. Diabetes Care. 2005;28:1649–55.
Klein R, Klein BE, Moss SE. Is obesity related to microvascular and macrovascular complications in diabetes? The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Arch Intern Med. 1997;157:650–6.
Lim LS, Tai ES, Mitchell P, Wang JJ, Tay WT, Lamoureux E, et al. C-reactive protein, body mass index, and diabetic retinopathy. Invest Ophthalmol Vis Sci. 2010;51:4458–63.
Raman R, Rani PK, Gnanamoorthy P, Sudhir RR, Kumaramanikavel G, Sharma T. Association of obesity with diabetic retinopathy: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study (SN-DREAMS Report no. 8). Acta Diabetol. 2010;47:209–15.
Dowse GK, Humphrey ARG, Collins VR, Plehwe W, Gareeboo H, Fareed D, et al. Prevalence and risk factors for diabetic retinopathy in the multiethnic population of Mauritius. Am J Epidemiol. 1998;147:448–57.
Wang J, Heymsfield SB, Aulet M, Thornton JC, Pierson RN Jr. Body fat from body density: underwater weighing vs. dual-photon absorptiometry. Am J Physiol. 1989;256:E829–834.
Zhou JB, Yuan J, Tang XY, Zhao W, Luo FQ, Bai L, et al. Is central obesity associated with diabetic retinopathy in Chinese individuals? An exploratory study. J Int Med Res. 2019;47:5601–12.
Banerji MA, Faridi N, Atluri R, Chaiken RL, Lebovitz HE. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:137–44.
Fang H, Berg E, Cheng X, Shen W. How to best assess abdominal obesity. Curr Opin Clin Nutr Metab Care. 2018;21:360–5.
Man REK, Sabanayagam C, Chiang PPC, Li LJ, Noonan JE, Wang JJ, et al. Differential association of generalized and abdominal obesity with diabetic retinopathy in Asian patients with type 2 diabetes. JAMA Ophthalmol. 2016;134:251–7.
Pu YF, He HB, Zhao ZG, Chen J, Ni YX, Zhong J, et al. Evaluation of visceral adipose in abdominal obesity and its clinical application. Zhonghua Yi Xue Za Zhi. 2008;88:2391–4.
Hwang IC, Bae JH, Kim JM. Relationship between body fat and diabetic retinopathy in patients with type 2 diabetes: a nationwide survey in Korea. Eye. 2019;33:980–7.
Sabanayagam C, Sultana R, Banu R, Rim T, Tham YC, Mohan S, et al. Association between body mass index and diabetic retinopathy in Asians: the Asian Eye Epidemiology Consortium (AEEC) study. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2020-318208.
Rooney D, Lye WK, Tan G, Lamoureux EL, Ikram MK, Cheng CY, et al. Body mass index and retinopathy in Asian populations with diabetes mellitus. Acta Diabetol. 2015;52:73–80.
Rajalakshmi R, Amutha A, Ranjani H, Ali MK, Unnikrishnan R, Anjana RM, et al. Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset type 1 and type 2 diabetes. J Diabetes Complications. 2014;28:291–7.
Sen D, Ghosh S, Roy D. Correlation of C-reactive protein and body mass index with diabetic retinopathy in Indian population. Diabetes Metab Syndr. 2015;9:28–9.
Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2019. American Diabetes Association. Diabetes Care. 2019;42(Suppl 1):S13–28.
World Health Organization. Measuring obesity—classification and description of anthropometric data. Report on a WHO consultation of the epidemiology of obesity. Warsaw 21–23 October 1987. Copenhagen: WHO; 1989. (Nutrition Unit document, EUR/ICP/NUT 123).
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes prevention program research group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Bays HE, Chapman RH, Grandy S, SHIELD Investigators’ Group. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int J Clin Pr. 2007;61:737–47.
Gray N, Picone G, Sloan F, Yashkin A. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med J. 2015;108:29–36.
Maskarinec G, Grandinetti A, Matsuura G, Sharma S, Mau M, Henderson BE, et al. Diabetes prevalence and body mass index differ by ethnicity: the multiethnic cohort. Ethn Dis. 2009;19:49–55.
Narayan KM, Boyle JP, Thompson TJ, Gregg EW, Williamson DF. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes Care. 2007;30:1562–6.
Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S. The metabolically obese, normal-weight individual revisited. Diabetes. 1998;47:699–713.
Kim ES, Jeong JS, Han K, Kim MK, Lee SH, Park YM, et al. Impact of weight changes on the incidence of diabetes mellitus: a Korean nationwide cohort study. Sci Rep. 2018;8:3735.
Kim JA, Kim DH, Kim SM, Park YG, Kim NH, Baik SH, et al. Impact of the dynamic change of metabolic health status on the incident type 2 diabetes: a nationwide population-based cohort study. Endocrinol Metab. 2019;34:406–14.
Preis SR, Massaro JM, Hoffmann U, D'Agostino RB, Levy D, Robins SJ, et al. Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart study. J Clin Endocrinol Metab. 2010;95:3701–10.
Afarid M, Attarzadeh A, Farvardin M, Ashraf H. The association of serum leptin level and anthropometric measures with the severity of diabetic retinopathy in type 2 diabetes mellitus. Med Hypothesis Disco Innov Ophthalmol. 2018;7:156–62.
Feller S, Boeing H, Pischon T. Body mass index, waist circumference, and the risk of type 2 diabetes mellitus: implications for routine clinical practice. Dtsch Arztebl Int. 2010;107:470–6.
Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Kostense PJ, et al. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn Study. Am J Clin Nutr. 2003;77:1192–7.
Jung KJ, Kimm H, Yun JE, Jee SH. Thigh circumference and diabetes: obesity as a potential effect modifier. J Epidemiol. 2013;23:329–36.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177–89.
van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter LM, et al. Blood pressure, lipids, and obesity are associated with retinopathy: the hoorn study. Diabetes Care. 2002;25:1320–5.
Diabetes Prevention Program Research Group. The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the Diabetes Prevention Program. Diabet Med J Br Diabet Assoc. 2007;24:137–44.
Looker HC, Nyangoma SO, Cromie D, Olson JA, Leese GP, Black M, et al. Diabetic retinopathy at diagnosis of type 2 diabetes in Scotland. Diabetologia. 2012;55:2335–42.
Goldberg IJ. Clinical review 124: diabetic dyslipidemia: causes and consequences. J Clin Endocrinol Metab. 2001;86:965–71.
Davidson RA, Travis MT, Bernier RM. Bruns-Garland syndrome (diabetic amyotrophy). Orthopedics. 2003;26:87–8.
Sasongko MB, Widyaputri F, Sulistyoningrum DC, Wardhana FS, Widayanti TW, Supanji S, et al. Estimated resting metabolic rate and body composition measures are strongly associated with diabetic retinopathy in Indonesian adults with type 2 diabetes. Diabetes Care. 2018;41:2377–84.
Author information
Authors and Affiliations
Contributions
AV, AJ, and ARA were equally responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists. RS was instrumental in data collection and analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Verma, A., Jha, A., Alagorie, A.R. et al. Association of anthropometric parameters as a risk factor for development of diabetic retinopathy in patients with diabetes mellitus. Eye 37, 303–308 (2023). https://doi.org/10.1038/s41433-022-01934-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01934-6