Abstract
Background
The relationship between eating behaviour and current body weight has been described. However little is known about the effect of polyunsaturated fatty acids (PUFA) in this relationship. Genetic contribution to a certain condition is derived from a combination of small effects from many genetic variants, and polygenic risk scores (PRS) summarize these effects. A PRS based on a GWAS for plasma docosahexaenoic fatty acid (DHA) has been created, based on SNPs from 9 genes.
Objective
To analyze the interaction between the PRS for plasma DHA concentration, body composition and eating behaviour (using the Children Eating Behaviour Questionnaire) in childhood.
Subjects/Methods
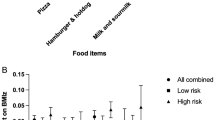
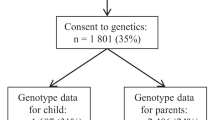
We analyzed a subsample of children from the Maternal, Adversity, Vulnerability and Neurodevelopment (MAVAN) cohort with PRS and measurements of eating behaviour performed at 4 years of age (n = 210), 6 y (n = 177), and body fat determined by bioelectric impedance at 4 y and 6 y or by air displacement plethysmography and dual-energy X-ray absorptiometry at 8 y (n = 42 and n = 37). PRS was based on the GWAS from Lemaitre et al. 2011 (p threshold = p < 5*10-6), and a median split created low and high PRS groups (high PRS = higher DHA level).
Results
In ALSPAC children, we observed an association between PRS and plasma DHA concentration (β = 0.100, p < 0.01) and proportion (β = 0.107, p < 0.01). In MAVAN, there were interactions between PRS and body fat on pro-intake scores in childhood, in which low PRS and higher body fat were linked to altered behaviour. There were also interactions between PRS and pro-intake scores early in childhood on body fat later in childhood, suggesting that the genetic profile and eating behaviour influence the development of adiposity at later ages.
Conclusions
A lower PRS (lower plasma PUFA) can be a risk factor for developing higher body fat associated with non-adaptive eating behaviour in childhood; it is possible that the higher PRS (higher plasma PUFA) is a protective feature.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Code availability
Code is available upon request to the corresponding author.
References
WHO. Report of the Commission on Ending Childhood Obesity: Geneva, Switzerland, 2016.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Albuquerque D, Nóbrega C, Manco L, Padez C. The contribution of genetics and environment to obesity. Br Med Bull. 2017;123:159–73.
Webber L, Hill C, Saxton J, Van Jaarsveld CH, Wardle J. Eating behaviour and weight in children. Int J Obes. 2009;33:21–8.
Carnell S, Wardle J. Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am J Clin Nutr. 2008;88:22–9.
Sanchez U, Weisstaub G, Santos JL, Corvalan C, Uauy R. GOCS cohort: children’s eating behavior scores and BMI. Eur J Clin Nutr. 2016;70:925–8.
Jansen A, Theunissen N, Slechten K, Nederkoorn C, Boon B, Mulkens S, et al. Overweight children overeat after exposure to food cues. Eat Behav. 2003;4:197–209.
Rui L. Brain regulation of energy balance and body weight. Rev Endocr Metab Disord. 2013;14:387–407.
Sastry PS. Lipids of nervous tissue: composition and metabolism. Prog Lipid Res. 1985;24:69–176.
Uauy R, Mena P. Long-chain polyunsaturated fatty acids supplementation in preterm infants. Curr Opin Pediatr. 2015;27:165–71.
Uauy R, Hoffman DR, Peirano P, Birch DG, Birch EE. Essential fatty acids in visual and brain development. Lipids. 2001;36:885–95.
Schoonjans K, Staels B, Auwerx J. Role of the peroxisome proliferator-activated receptor (PPAR) in mediating the effects of fibrates and fatty acids on gene expression. J Lipid Res. 1996;37:907–25.
Clarke SD. The multi-dimensional regulation of gene expression by fatty acids: polyunsaturated fats as nutrient sensors. Curr Opin Lipidol. 2004;15:13–8.
Alsaleh A, Maniou Z, Lewis FJ, Hall WL, Sanders TA, O’Dell SD. ELOVL2 gene polymorphisms are associated with increases in plasma eicosapentaenoic and docosahexaenoic acid proportions after fish oil supplement. Genes Nutr. 2014;9:362.
Koletzko B, Lattka E, Zeilinger S, Illig T, Steer C. Genetic variants of the fatty acid desaturase gene cluster predict amounts of red blood cell docosahexaenoic and other polyunsaturated fatty acids in pregnant women: findings from the Avon Longitudinal Study of Parents and Children. Am J Clin Nutr. 2011;93:211–9.
Burrin DG, Marsmann HJ (eds). Biology of metabolism in growing animals. Vol. 3. Elsevier, Edinburgh & New York, 2005.
Balanza-Martinez V, Fries GR, Colpo GD, Silveira PP, Portella AK, Tabares-Seisdedos R, et al. Therapeutic use of omega-3 fatty acids in bipolar disorder. Expert Rev Neurother. 2011;11:1029–47.
Muhlhausler BS, Gibson RA, Makrides M. The effect of maternal omega-3 long-chain polyunsaturated fatty acid (n-3 LCPUFA) supplementation during pregnancy and/or lactation on body fat mass in the offspring: a systematic review of animal studies. Prostaglandins Leukot Essent Fatty Acids. 2011;85:83–8.
Lemaitre RN, Tanaka T, Tang W, Manichaikul A, Foy M, Kabagambe EK, et al. Genetic loci associated with plasma phospholipid n-3 fatty acids: a meta-analysis of genome-wide association studies from the CHARGE Consortium. PLoS Genetics. 2011;7:e1002193.
O’Donnell KA, Gaudreau H, Colalillo S, Steiner M, Atkinson L, Moss E, et al. The maternal adversity, vulnerability and neurodevelopment project: theory and methodology. Can J Psychiatry. Revue Canadienne de Psychiatrie. 2014;59:497–508.
Golding Pembrey, Jones TeamTAS. ALSPAC–The Avon Longitudinal Study of Parents and Children. Paediatr Perinatal Epidemiol. 2001;15:74–87.
Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, et al. Cohort Profile: the ‘children of the 90s’-the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–27.
McCarthy S, Das S, Kretzschmar W, Delaneau O, Wood AR, Teumer A, et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat Genet. 2016;48:1279–83.
Gaunt TR, Shihab HA, Hemani G, Min JL, Woodward G, Lyttleton O, et al. Systematic identification of genetic influences on methylation across the human life course. Genome Biol. 2016;17:61–61.
Chen LM, Yao N, Garg E, Zhu Y, Nguyen TTT, Pokhvisneva I, et al. PRS-on-Spark (PRSoS): a novel, efficient and flexible approach for generating polygenic risk scores. BMC Bioinform. 2018;19:295.
Wray NR, Lee SH, Mehta D, Vinkhuyzen AA, Dudbridge F, Middeldorp CM. Research review: polygenic methods and their application to psychiatric traits. J Child Psychol Psychiatry Allied Discip. 2014;55:1068–87.
Dudbridge F. Power and predictive accuracy of polygenic risk scores. PLoS Genet. 2013;9:e1003348.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children’s eating behaviour questionnaire. J Child Psychol Psychiatry Allied Discip. 2001;42:963–70.
Miller SA, Taveras EM, Rifas-Shiman SL, Gillman MW. Association between television viewing and poor diet quality in young children. Int J Pediatr Obes: IJPO: Off J Int Assoc Study Obes. 2008;3:168–76.
Québec. OPDDD. Manuel de nutrition clinique, vol. 3ième édition. Quèbec, 2000.
Katamay SW, Esslinger KA, Vigneault M, Johnston JL, Junkins BA, Robbins LG, et al. Eating well with Canada’s Food Guide (2007): development of the food intake pattern. Nutr Rev. 2007;65:155–66.
Villar J, Ismail LC, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Group. WMGRS. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development, World Health Organization: Geneva, 2006.
Santos Ferreira DL, Hübel C, Herle M, Abdulkadir M, Loos RJF, Bryant-Waugh R, et al. Associations between blood metabolic profile at 7 years old and eating disorders in adolescence: findings from the Avon longitudinal study of parents and children. Metabolites. 2019;9:191.
Soininen P, Kangas AJ, Würtz P, Suna T, Ala-Korpela M. Quantitative serum nuclear magnetic resonance metabolomics in cardiovascular epidemiology and genetics. Circ: Cardiovasc Genet. 2015;8:192–206.
Rump P, Mensink RP, Kester AD, Hornstra G. Essential fatty acid composition of plasma phospholipids and birth weight: a study in term neonates. Am J Clin Nutr. 2001;73:797–806.
Grootendorst-van Mil NH, Tiemeier H, Steenweg-de Graaff J, Koletzko B, Demmelmair H, Jaddoe VWV, et al. Maternal plasma n-3 and n-6 polyunsaturated fatty acids during pregnancy and features of fetal health: fetal growth velocity, birth weight and duration of pregnancy. Clin Nutr. 2018;37:1367–74.
Vlaardingerbroek H, Hornstra G. Essential fatty acids in erythrocyte phospholipids during pregnancy and at delivery in mothers and their neonates: comparison with plasma phospholipids. Prostaglandins Leukot Essent Fatty Acids. 2004;71:363–74.
Brouwer-Brolsma EM, van de Rest O, Godschalk R, Zeegers MPA, Gielen M, de Groot RHM. Associations between maternal long-chain polyunsaturated fatty acid concentrations and child cognition at 7 years of age: the MEFAB birth cohort. Prostaglandins Leukot Essent Fatty Acids. 2017;126:92–7.
de Jong C, Kikkert HK, Seggers J, Boehm G, Decsi T, Hadders-Algra M. Neonatal fatty acid status and neurodevelopmental outcome at 9 years. Early Hum Dev. 2015;91:587–91.
Tay CW, Chin YS, Lee ST, Khouw I, Poh BK, Group SMS. Association of eating behavior with nutritional status and body composition in primary school-aged children. Asia Pac J Public Health. 2016;28:47S–58S. 5 Suppl
Passos DRD, Gigante DP, Maciel FV, Matijasevich A. Children’s eating behavior: comparison between normal and overweight children from a school in Pelotas, Rio Grande do Sul, Brazil. Revista Paulista de Pediatria. 2015;33:42–9.
Lombardo YB, Chicco AG. Effects of dietary polyunsaturated n-3 fatty acids on dyslipidemia and insulin resistance in rodents and humans. A review. J Nutr Biochem. 2006;17:1–13.
Semple RK, Chatterjee VK, O’Rahilly S. PPAR gamma and human metabolic disease. J Clin Invest. 2006;116:581–9.
Simopoulos AP. Essential fatty acids in health and chronic disease. Am J Clin Nutr. 1999;70:560S–569S. 3 Suppl
Cifre M, Díaz-Rúa R, Varela-Calviño R, Reynés B, Pericás-Beltrán J, Palou A, et al. Human peripheral blood mononuclear cell in vitro system to test the efficacy of food bioactive compounds: effects of polyunsaturated fatty acids and their relation with BMI. Mol Nutr Food Res. 2017;61:1600353.
Galmés S, Cifre M, Palou A, Oliver P, Serra F. A Genetic score of predisposition to low-grade inflammation associated with obesity may contribute to discern population at risk for metabolic syndrome. Nutrients. 2019;11:298.
Bondi CO, Taha AY, Tock JL, Totah NK, Cheon Y, Torres GE, et al. Adolescent behavior and dopamine availability are uniquely sensitive to dietary omega-3 fatty acid deficiency. Biol Psychiatry. 2014;75:38–46.
Ferreira CF, Bernardi JR, Krolow R, Arcego DM, Fries GR, de Aguiar BW, et al. Vulnerability to dietary n-3 polyunsaturated fatty acid deficiency after exposure to early stress in rats. Pharmacol Biochem Behav. 2013;107:11–9.
Mathieu G, Oualian C, Denis I, Lavialle M, Gisquet-Verrier P, Vancassel S. Dietary n-3 polyunsaturated fatty acid deprivation together with early maternal separation increases anxiety and vulnerability to stress in adult rats. Prostaglandins Leukot Essent Fatty Acids. 2011;85:129–36.
Frances H, Drai P, Smirnova M, Carrie I, Debray M, Bourre JM. Nutritional (n-3) polyunsaturated fatty acids influence the behavioral responses to positive events in mice. Neurosci Lett. 2000;285:223–7.
Suzuki H, Park SJ, Tamura M, Ando S. Effect of the long-term feeding of dietary lipids on the learning ability, fatty acid composition of brain stem phospholipids and synaptic membrane fluidity in adult mice: a comparison of sardine oil diet with palm oil diet. Mech Ageing Dev. 1998;101:119–28.
Chalon S. Omega-3 fatty acids and monoamine neurotransmission. Prostaglandins Leukot Essent Fatty Acids. 2006;75:259–69.
Kitajka K, Sinclair AJ, Weisinger RS, Weisinger HS, Mathai M, Jayasooriya AP, et al. Effects of dietary omega-3 polyunsaturated fatty acids on brain gene expression. Proc Natl Acad Sci USA. 2004;101:10931–6.
Kitajka K, Puskás LG, Zvara A, Hackler L Jr, Barceló-Coblijn G, Yeo YK, et al. The role of n-3 polyunsaturated fatty acids in brain: modulation of rat brain gene expression by dietary n-3 fatty acids. Proc Natl Acad Sci USA. 2002;99:2619–24.
Kuperstein F, Yakubov E, Dinerman P, Gil S, Eylam R, Salem N Jr, et al. Overexpression of dopamine receptor genes and their products in the postnatal rat brain following maternal n-3 fatty acid dietary deficiency. J Neurochem. 2005;95:1550–62.
Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–13.
Acknowledgements
We thank the mothers and their children who participated in this study. We thank Irina Pokhvisneva and Sachin Patel for their technical support.
Funding
This work was supported by National Commission for Scientific and Technological Research (CONICYT-PCHA/Doctorado Nacional/2014-63140222) (AJ), Proyecto de Consolidación de la internacionalización de la investigación y postgrado de la Universidad de Chile UCH-1566 (AJ), Canadian Institutes of Health Research (CIHR) [PJT-166066, PPS] and the JPB Foundation through a grant to the JPB Research Network on Toxic Stress: A Project of the Center on the Developing Child at Harvard University. Dr. Levitan acknowledges support from the Cameron Holcombe Wilson Chair in Depression Studies, CAMH and University of Toronto.
Author information
Authors and Affiliations
Contributions
All authors contributed to this work. Conceptualization PPS, AMJO, MJM; data curation AMJO; formal analysis AMJO; funding acquisition PPS, MJM, RDL; investigation PPS, RDL, RA; methodology PPS, RDL, RA, MJM; project administration PPS; resources MJM, PPS, RDL; supervision PPS, MLG, PC; validation AMJO; visualization AMJO, writing–original draft AMJO, PPS, MLG, PC; writing–review & editing AMJO, PPS, MLG, PC.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jaramillo-Ospina, A., Casanello, P., Garmendia, M.L. et al. Interactions between a polygenic risk score for plasma docosahexaenoic fatty acid concentration, eating behaviour, and body composition in children. Int J Obes 46, 977–985 (2022). https://doi.org/10.1038/s41366-022-01067-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01067-6