Abstract
Appropriate biomarkers may help distinguish the biological behavior of different types of lymphoma and their response to traditional chemotherapy. Extranodal natural killer/T-cell lymphoma (ENKTL) and diffuse large B-cell lymphoma (DLBCL) belong to different subtypes of non-Hodgkin's lymphoma, the biological behavior and prognosis of them are very different, programmed cell death receptor 1 (PD-1) and its ligand (PD-L1) have been investigated in these two types of diseases. However, few studies addressed the difference of PD-1/PD-L1 levels between ENKTL and DLBCL, in order to find out the difference and related clinical application value, the clinical data and tumor tissue paraffin sections of 24 newly diagnosed ENKTL patients and 42 newly diagnosed diffuse large B-cell lymphoma (DLBCL) were collected. PD-1/PD-L1 levels in tumor tissues were detected by immunohistochemical staining. The relationship between the PD-1/PD-L1 levels and clinical data of patients with ENKTL patients was analyzed. Both patient groups showed PD-1 level in tumor tissue of ENKTL patients was significantly lower than that of DLBCL patients (P < 0.05), while the PD-L1 level in tumor tissues of ENKTL patients was not different from DLBCL (P < 0.05). In addition, the ENKTL patients with B symptoms, elevated lactate dehydrogenase (LDH) levels and decreased hemoglobin (HGB) concentrations had lower level of PD-1 in tumor tissue. PD-L1 level in tumor tissues, the LDH level, Epstein-Barr genome (EBV-DNA) copy and Ki-67 index may affect the outcomes of ENKTL patients (P < 0.05), but they were not independent factors. PD-L1 levels in tumor tissues has clinical significance in ENKTL patients, which suggested that the PD-1/PD-L1 signal pathway may be involved in the immune escape of ENKTL and play different roles in different lymphoma subtypes.
Similar content being viewed by others
Introduction
Extranodal NK/T-cell lymphoma, nasal type (ENKTL) is an aggressive non-Hodgkin lymphoma which originates from T cell or NK-like cell, it often involve the nasal cavity, face and upper respiratory tract. Compared to diffuse large B-cell lymphoma (DLBCL), this disease is characterized by more difficult diagnosis, higher malignant, rapider progress, and easier to be resistant to traditional chemotherapy. Therefore, there is currently no standard treatment plan for ENKTL1. The above characteristics are probably related to tumor cells evading the immune response of the body, the signaling pathway involving programmed cell death receptor 1 (PD-1) is likely one mechanisms of immune evasion2,3.
Existing studies have shown that PD-1 is mainly expressed on CD4+ or CD8+ T cell membranes, and it has two types of ligands, which are PD-L1 and PD-L2. PD-L1 is the main ligand of PD-1 in the human body, PD-L1 is expressed in not only immune cells such as activated lymphocytes, NK cells and macrophages, but also tissue cells such as lung and vascular endothelium2. What is more, it is expressed at high levels in tumor cells, such as melanoma4, gastric cancer5, kidney cancer6, high levels of PD-L1 expressed on tumor cells can inhibit the proliferation and activation of lymphocytes by interacting with PD-1 on lymphocytes to achieve the immune escape of tumor cells2. Recent studies have shown that PD-L1 level in nasal biopsy tissues of ENKTL patients is much higher than that of rhinitis patients7. At present, the clinical trials of PD-1 monoclonal antibody are already underway. PD-1 monoclonal antibody has achieved very good outcomes in ENKTL8, but it didn’t achieve good outcomes in DLBCL9. Therefore, we hope to explore the reasons by comparing the expression differences of PD-1/PD-L1 level in these two diseases. Based on the above background, we used a retrospective case–control study to analyze the differences in PD-1/PD-L1 levels in tumor tissues of between ENKTL and DLBCL patients.
Therefore we examined PD-1/PD-L1 in tumor tissues of ENKTL and DLBCL patients. Our results show that PD-1/PD-L1 level in tumor tissues of ENKTL patients are useful for staging and prediction of treatment response in ENKTL. The same results were not obtained for patients with DLBCL, another type of lymphoma, suggesting that the biomarker may show some clinical significance for ENKTL.
Materials and methods
Study population and treatment
This retrospective study included 24 cases of ENKTL (18 males, median age 49.5 years) diagnosed in West China Hospital of Sichuan University from December 2017 to December 2018 and 42 cases of DLBCL patients, and pathological paraffin sections of all 66 patients have been obtained from the Department of Pathology, West China Hospital, Sichuan University. The diagnostic criteria are based on the 2008 WHO classification criteria for hematopoietic and lymphoid tissue tumors10. The outcomes evaluation after two courses of chemotherapy follows the "Evaluation Criteria for the outcomes of Malignant Lymphoma", including complete remission (CR), partial remission (PR), stable disease (SD) and disease progression (PD)11. We have signed an informed consent form with all research subjects, and have been approved by the Ethics Committee of West China Hospital of Sichuan University. All methods are performed in accordance with the relevant guidelines and regulations.
Immunohistochemical staining (IHC) for PD-1/PD-L1
Paraffin-embedded sections (3 µm) were used for immunohistochemical staining (IHC). After being dewaxed and hydrated, antigen retrieval (citric acid with PH = 9) and inactivation of endogenous peroxidase, the primary antibody [PD-L1 antibody [28-8] (Abcam, Cambridge, UK)/PD-1 antibody (Zhongshan Jinqiao, Beijing, China), dilution 1:75] and general secondary antibody for antibody incubation, after washing with running water, DAB is added dropwise to develop color, after the color is developed, hematoxylin counterstaining is carried out, and then dehydrated and mounted. Observe the slices under a microscope and collect images, IHC was accomplished by avidin–biotin peroxidase complex detection system. The percentage of PD-1/PD-L1 expression (the number of cells stained with membranes in the total number of tumor cells) was analyzed by Image J software. The percentage > 30% was defined as PD-L1 (+), while the percentage > 5% was considered PD-1 (+)12.
Statistical analyses
PD-1/PD-L1 level in tumor tissues are presented as the median and interquartile range [M(IQR)]. The Kruskal–Wallis test was used to analyze the differences between groups, and the Mann–Whitney U test and Spearman rank correlation analysis were used to analyze the relationship between PD-1/PD-L1 level in tumor and the clinical data of patients. Fish test and Logistic regression were used to conduct univariate and multivariate analysis of predictors of treatment response in ENKTL patients. We set P value < 0.05 as the significant difference.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of West China Hospital of Sichuan University. Participants provided written consent for their anonymized clinical data to be used and published for research purposes.
Results
Baseline clinical characteristics of patients
Baseline clinical characteristics of 24 patients with ENKTL and 42 ones with DLBCL are summarized in Table 1. In the ENKTL group, 7 (29%) was in stage III-IV, and 8 (33%) had LDH > 250 U/L. 23 (88%) patients accepted anthracycline-containing chemotherapy regimens. All patients received at least two cycles of chemotherapy before radiotherapy. After two courses of chemotherapy, 8 patients (33%) achieved CR.
PD-1 and PD-L1 levels in tumor tissues and relationships with clinical variables
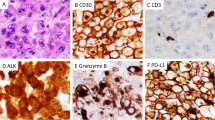
The distribution and expression of PD-1/PD-L1 in tumor tissues were investigated by immunohistochemical staining. Membranes of positive cells in tumor tissues from ENKTL and DLBCL patients were stained brown (Fig. 1). PD-L1 (+) was defined as positive cells proportion > 30% and PD-1 (+) as > 5%12. In 24 ENKTL patients, 19 (79%) were PD-L1 (+) and 9 (38%) were PD-1(+) (Fig. 2A). In 42 DLBCL patients, 25 (60%) were PD-L1 (+) and 29 (69%) were PD-1 (+) (Fig. 2B). PD-1 level in tumor tissues in ENKTL patients [3.50(0.00–9.75)] was significantly lower than in DLBCL patients [21.00(1.75–44.00), P = 0.0021] (Fig. 2C), while PD-L1 level was not statistically different between ENKTL [49.50(35.25–80.00)] and DLBCL [50.50(2.50–77.00)] groups (Fig. 2D). In ENKTL patients, PD-1 level in tumor tissues were significantly lower with B symptoms#, higher levels of LDH (P < 0.05, Fig. 3A), and lower hemoglobin level (Spearman r = 0.6131, P = 0.0014, Fig. 3B).
Details and correlation analysis of PD-1/PD-L1 expression in tumor tissues of ENKTL (A) and DLBCL (B) patients. No correlation was found between PD-1 and PD-L1 level from tumor tissues of ENKTL and DLBCL patients. Scatter plot of PD-1 (C) and PD-L1 (D) expression showed that PD-1 level in tumor tissues from ENKTL patients was lower than DLBCL.**P < 0.01.
(A,B) In ENKTL patients, PD-1 level in tumor tissues varied with (A) B symptoms#, (A) lactate dehydrogenase (LDH) concentration, (B) hemoglobin. *P < 0.05. #The B symptoms of lymphoma mainly refer to systemic symptoms, which usually include three aspects: (1) Fever, with a body temperature above 38 °C, usually for more than 3 consecutive days, but there is no clear clinical cause of infection. (2) The weight loss reached more than 10% within 6 months. (3) Night sweats. The so-called night sweats refer to the sweating of the patient after falling asleep.
Association of PD-1 or PD-L1 biomarkers with treatment response
As shown in Table 2, Univariate analysis showed that ENKTL patients with higher levels of PD-L1 in tumor tissues (P = 0.0218) were more difficult to achieve CR, as were patients with high levels of LDH (P = 0.0222), Ki-67 index (P = 0.0304) and EBV-DNA copies (P = 0.0087). In multivariate analysis, the covariates we chose are LDH, EBV-DNA copies, Ki-67 index, PD-L1 level in tumor tissues, however, no one varied significantly with treatment response.
Correlation among PD-1/PD-L1 level in tumor tissues, PD-L1mRNA level in PBMCs and sPD-L1 level
Early research by our research group detected expressions of PD-1/PD-L1 in peripheral blood mononuclear cells (PBMCs) and plasma. We used the same cohort of patients as before, however, pathological specimens of some patients are not available, so the number of patients included in this article has decreased. We made a correlation analysis of PD-1/PD-L1 level between tumor tissue and peripheral blood, our results showed PD-1 level in tissues was correlated with PD-L1mRNA level in PBMCs (P = 0.0109, Spearman r = − 0.5097, Fig. 4A) and sPD-L1 level (P = 0.0086, Spearman r = − 0.5237, Fig. 4B), Unfortunately, we didn’t find a correlation between PD-L1 level in tumor tissues and soluble PD-L1 level in peripheral blood.
Discussion
Studies have found that in patients with follicular lymphoma, PD-1 is mainly expressed on CD4+ T lymphocytes in lymph node follicles13. Roncador G, García Verdes-Montenegro JF found that PD-1 is abnormally highly expressed in tissues of patients with angioimmunoblastic lymphoma (AITL)14. Jo et al. have reported the low level of PD-1 in tumor tissues of ENKTL patients15, and Muhamad et al. also found that PD-1 was positive in 20.5% of stroma, but undetectable on lymphoma cells16. Similarly, this study found that PD-1 level in tumor tissues of ENKTL patients was significantly lower than that of DLBCL patients, and that PD-1 level in tumor tissues of ENKTL patients with B symptoms, increased LDH levels, and decreased hemoglobin concentration was lower. We believe that the low level of PD-1(+) infiltrating lymphocytes constitutes the immunosuppressive effect of lymphoma cells in tumor microenvironment and promotes tumor immune escape, from this perspective, the lower PD-1 level in ENKTL tumor tissue may be one of the possible reasons why ENKTL progresses faster than DLBCL.
In addition, Chen BJ, Chapuy B and other scholars have found that PD-L1 is expressed in HL, DLBCL, ENKTL and other lymphoma tissues, but no expression has been detected in Burkitt lymphoma17, similar to this, this study is also found that PD-L1 is highly expressed in tumor tissues of ENKTL and DLBCL patients, it is suggested that the increased expression of PD-L1 is one of the possible reasons for the defect of cellular immune function in patients.
The outcomes-related analysis in ENKTL patients found that the LDH level, EBV-DNA copy number, Ki-67 index and PD-L1 level in tumor tissues will affect the outcomes of ENKTL patients, but are not independent factors. Li et al. also found that Persistent peripheral blood EBV-DNA positive with high expression of PD-L1 and upregulation of CD4 + CD25 + T cell ratio in early stage NK/T cell lymphoma patients may predict worse outcome18. Similarly, we also found high levels of EBV-DNA copies were more difficult to achieve CR.
Bi et al. found that Patients with a high concentration of serum soluble PD-L1 or with a high percentage of PD-L1 expression in tumor specimens exhibited significantly lower response rate to treatment and remarkably worse survival, compared with their counterparts19. Wang et al. also found that Patients with high pretreatment had shorter progression-free survival and overall survival20. However, Kim found that PD-L1 expression was the only significant independent predictor for longer OS in patients with advanced stage (III/IV) ENKTL21. For this contradictory result, We analyzed the patient staging of three articles, We found that the patients studied in the first two articles are all classified as stage I–II patients, the third article was for patients with stage III–IV. We believed that PD-L1-mediated inhibition may lead to local depletion of cytokines involved in the survival and growth of cancer cells, resulting in anti-tumor effects in patients with advanced stage (III/IV) ENKTL, This also showed that PD-L1 played different roles in ENKTL patients of different stages.
These suggest that the PD-1/PD-L1 signaling pathway may be involved in the disease progression of ENKTL patients, and is closely related to the patient's response to traditional chemotherapy.
In summary, the results of this study showed that the expression of PD-1/PD-L1 in the tumor tissues of patients is different in ENKTL and DLBCL patients, suggesting that the PD-1/PD-L1 signaling pathway has different roles in different lymphoma subtypes.
Data availability
The datasets generated and analyzed in the current study are available from the corresponding author on reasonable request.
References
Kwong, Y. L. et al. CD56+ NK lymphomas: Clinicopathological features and prognosis. Br. J. Haematol. 97(4), 821–829 (1997).
Keir, M. E. et al. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 26, 677–704 (2008).
Rong, Q. X. et al. GM-CSF mediates immune evasion via upregulation of PD-L1 expression in extranodal natural killer/T cell lymphoma. Mol. Cancer 20(1), 80 (2021).
Chen, G. et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature 560(7718), 382–386 (2018).
Wu, C. et al. Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in gastric carcinoma and its clinical significance. Acta Histochem. 108(1), 19–24 (2006).
Thompson, R. H. et al. Tumor B7–H1 is associated with poor prognosis in renal cell carcinoma patients with long-term follow-up. Cancer Res. 66(7), 3381–3385 (2006).
Han, L. et al. Role of programmed death ligands in effective T-cell interactions in extranodal natural killer/T-cell lymphoma. Oncol. Lett. 8(4), 1461–1469 (2014).
Lv, K. et al. Selection of new immunotherapy targets for NK/T cell lymphoma. Am. J. Transl. Res. 12(11), 7034–7047 (2020).
Lesokhin, A. M. et al. Nivolumab in patients with relapsed or refractory hematologic malignancy: Preliminary results of a phase Ib study. J. Clin. Oncol. 34(23), 2698–2704 (2016).
Sabattini, E. et al. WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: An overview. Pathologica 102(3), 83–87 (2010).
Cheson, B. D. et al. International Harmonization Project on Lymphoma. Revised response criteria for malignant lymphoma. J. Clin. Oncol. 25(5), 579–586 (2007).
Kiyasu, J. et al. Expression of programmed cell death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. Blood 126(19), 2193–2201 (2015).
Yang, Z. Z. et al. PD-1 expression defines two distinct T-cell sub-populations in follicular lymphoma that differentially impact patient survival. Blood Cancer J. 5, e281 (2015).
Roncador, G. et al. Expression of two markers of germinal center T cells (SAP and PD-1) in angioimmunoblastic T-cell lymphoma. Haematologica 92(8), 1059–1066 (2007).
Jo, J. C. et al. Expression of programmed cell death 1 and programmed cell death ligand 1 in extranodal NK/T-cell lymphoma, nasal type. Ann. Hematol. 96(1), 25–31 (2017).
Muhamad, H. et al. Programmed cell death 1 and programmed cell death ligands in extranodal natural killer/T cell lymphoma: Expression pattern and potential prognostic relevance. Acta Haematol. 143, 78–88 (2020).
Chen, B. J. et al. PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin. Cancer Res. 19(13), 3462–3473 (2013).
Li, P. et al. Persistent peripheral blood EBV-DNA positive with high expression of PD-L1 and upregulation of CD4 + CD25 + T cell ratio in early stage NK/T cell lymphoma patients may predict worse outcome. Ann. Hematol. 97, 2381–2389 (2018).
Bi, X. W. et al. PD-L1 is upregulated by EBV-driven LMP1 through NF-κB pathway and correlates with poor prognosis in natural killer/T-cell lymphoma. J. Hematol. Oncol. 9(1), 109 (2016).
Wang, H. et al. High post-treatment serum levels of soluble programmed cell death ligand 1 predict early relapse and poor prognosis in extranodal NK/T cell lymphoma patients. Oncotarget 7(22), 33035–33045 (2016).
Kim, W. Y. et al. Expression of programmed cell death ligand 1 (PD-L1) in advanced stage EBV-associated extranodal NK/T cell lymphoma is associated with better prognosis. Virchows Arch. 469, 581–590 (2016).
Funding
This research was supported by a grant to C.X. from the Sichuan Science and Technology Program (2019YFS0027).
Author information
Authors and Affiliations
Contributions
C.X. initiated the project and designed the research. Y.F. and X.F. performed most experiments, analyzed the data, and drafted the manuscript. X.F. assisted in collecting clinical specimens. C.J., X.C., X.Y., X.F. and Y.Z. performed some experiments and provided critical suggestions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, Y., Feng, X., Jing, C. et al. The expression and clinical significance of programmed cell death receptor 1 and its ligand in tumor tissues of patients with extranodal nasal NK/T cell lymphoma. Sci Rep 12, 36 (2022). https://doi.org/10.1038/s41598-021-02515-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02515-5
This article is cited by
-
Elevated serum IL-6 and total IgEAb are associated with poor survival in natural killer/T-cell lymphoma
Annals of Hematology (2024)
-
Novel target and treatment agents for natural killer/T-cell lymphoma
Journal of Hematology & Oncology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.