Abstract
Purpose
To compare the outcomes of three techniques for removing internal angular dermoid cysts: lid crease, sub-brow, and direct mini-incision.
Methods
In this single-center trial, 47 children with internal angular dermoids were enrolled and randomly assigned to one of three surgical groups: group A, sub-brow, group B, lid crease, and group C, direct mini-incision. Outcome measures were operative time, postoperative scar quality using Stony Brook Scar Evaluation Scale (SBSES), scar visibility, and family satisfaction.
Results
In each group, fifteen patients completed follow-up and were analysed. The operation time (median/IQR) in Group C was significantly shorter (10/5 min) compared with group A (25/10 min) and B (35/20 min) (p < 0.001). Group B had the least visible scar at all follow-up visits. Both group B and C showed superior scar quality using SBSES compared with group A at 6 months (p < 0.001). All families in group B (100%) found the scar excellent compared to 11 families in group C (40%) and 6 families in group A (73.3%). Persistent postoperative inflammation was noticed in two patients in group C. No cases of recurrence were recorded.
Conclusions
Both the lid crease and direct mini-incision approaches result in superior scar quality with minimum visibility compared with the sub-brow technique, however, the lid crease technique shows a prolonged operation time particularly for cysts outside the rim.
Similar content being viewed by others
Introduction
Dermoid cysts are the most common periorbital masses in children [1]. These choristomatous lesions arise from aberrant ectodermal elements at suture lines and can be superficial or deep depending on their location [2, 3].
Superficial lesions typically present earlier in life as subcutaneous, slow growing masses and are found most commonly in the supero-temporal aspect of the orbit (external angular dermoid), arising from the frontozygomatic suture [4]. The supero-nasal lesions (internal angular dermoid) arising along the fronto-lacrimal suture represent the second most common type (10–46%) [3,4,5].
Internal angular dermoids pose unique diagnostic and therapeutic challenges compared to their external angular counterparts due to the broad differential diagnosis in this region [6,7,8]. Furthermore, their relation to the trochlea and superior oblique tendon [9], along with their increased risk of intraoperative rupture give rise to additional challenges [10].
Given the conspicuous location of this type of dermoid cyst, direct excisional techniques may leave visible cutaneous scars that could pose a psychological burden on children. Therefore, several approaches have been developed to minimize incision line visibility. Examples of such approaches include camouflaging the incision in the brow or the eyelid crease or using endoscopic excision through scalp incisions [11,12,13,14,15,16]. Attempting to minimize the length of skin incision, some authors recommend evacuation of the cyst contents before complete excision of its wall through a very small direct incision [17].
This study aims to compare the cosmetic and functional outcomes of three surgical techniques for removing of internal angular dermoid cysts including eyelid crease, sub-brow, and a direct mini-incision.
Methods and materials
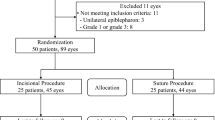
This randomized, parallel-controlled clinical trial was conducted at Fayoum University Hospitals from May 2020 to May 2021. This research adhered to the tenets of the Declaration of Helsinki and was approved by Fayoum University, Faculty of Medicine Scientific Research Ethics Committee (R114). Informed consent was obtained from parents/ guardians of all included children before enrollment in this study after discussing the different surgical options, benefits and risks. Written consent was obtained from parents/guardians for use of photograph(s) of their children in published media. Study population included children between 2 and 12 years old having internal angular dermoid cyst diagnosed both clinically and radiologically. Children with prior eyelid or orbital surgery, recurrent cases, cases with intracranial or nasal extension and cases with doubtful diagnosis were excluded from this study. Additionally, patients with <6 months follow-up were excluded from the statistical analysis.
The recruited patients were randomly assigned via computer-generated numbers to one of three parallel groups, in 1:1:1 ratio. Group A: underwent cyst excision through medial infra-brow incision (n = 15), group B: underwent cyst excision through medial lid crease incision (n = 15), and group C: underwent evacuation of the dermoid cyst through a direct mini-incision before complete removal of the wall (n = 15). Allocation sequence was concealed in sealed opaque envelops. Masking of the study participants and personnel was not possible.
All included children underwent complete preoperative eye examination and orbital imaging. The side, the size, and the site of the cyst (outside or inside the rim) were recorded (Fig. 1A–D).
Surgical technique
All surgical procedures were performed under general anesthesia under complete aseptic condition by the first author (Fig. 1E, F). In group A, a skin incision of about 15 mm long, is made below the medial eyebrow. Dissection continues through the orbicularis muscle to expose the entire anterior surface of the cyst. A Freer periosteal elevator is used to dissect the cyst from the underlying bone aiming for intact excision.
In group B, a skin incision, 15 to 20 mm in length, is made along the medial upper eyelid crease. Dissection continues through the orbicularis muscle to the orbital septum. For cysts laying inside the orbital rim, dissection is continued within the orbital septum using Westcott scissors in order to identify the cyst (Supplementary Fig. S1A–E). At this point, the cyst can be easily separated from the surrounding orbital fat and levator muscle/aponeurosis. For cysts outside the orbital rim, dissection is made in the sub-orbicularis plane keeping the orbital septum intact. The cyst is fully exposed by retracting the wound medially (Supplementary Fig. S1F–H). While grasping the cyst with fine forceps, any attachments to periosteum were further dissected from the lesion with a Freer periosteal elevator aiming for intact excision.
In group C, a small horizontal skin incision, 4 to 5 mm in length, is made directly over the cyst using a scalpel no. 15 within relaxed skin tension lines in the thin lid skin. After exposure of the anterior portion of the cyst, a small incision is made in the of the cyst through which complete aspiration of the cyst contents is performed using a suction catheter. The cyst capsule is then completely excised using scissors. The surgical site is irrigated with triamcinolone acetonide solution (Supplementary Fig. S2).
Skin is then closed using interrupted polyglactin 910 6/0 sutures.
Any intraoperative complications were recorded and operative time for each procedure was documented. Topical antibiotic/steroid ointment was prescribed to each patient. Ice packs were recommended in the first 48 h followed by hot foment until resolution of the oedema. The skin suture was removed at 5 days postoperatively to avoid tissue reaction.
Postoperative evaluation and scar assessment
Patients were asked to return for follow-up at 5 days, 1, 3, and 6 months following surgery. All postoperative assessments and grading were carried out by two independent observers, not involved in the surgery or the study (in person). The main outcome measures were operative time, scar visibility with eyes open and scar quality using SBSES with eyes closed. Secondary outcome measures were parenteral satisfaction.
Scar evaluation
With eyes open, scar visibility was assessed by direct visualization in the same room and under the same light conditions from 1 m distance. If the observers were unable to detect the side of surgery it was assessed as invisible = grade 1. If the scar was appreciable, it was graded as minimally visible = grade 2, moderately visible = grade 3, and easily visible = grade 4 [18].
With eyes closed, the scar was evaluated using the Stony Brook Scar Evaluation Scale (SBSES) [19]. The scar was assigned zero or one point each for the presence or absence of a width more than 2 mm, elevation or depression, discoloration, hatch marks, and overall poor appearance. The individual scores were summed to obtain a total score ranging from 0 (the worst) to 5 (the best).
Family’s questionnaire; at the last follow-up visit, the family members were given a questionnaire to evaluate scar visibility, to score their satisfaction of the skin incision appearance, and to state some social factors related to the scar appearance [13].
Statistical analysis
Descriptive statistics for the variables were presented in the form of median, interquartile range for numeric variables. While frequencies and percentages are used for categorical variables. Comparison of the characteristics and outcome in the three groups was performed using the Chi-square test for categorical variables while the Kruskal–Wallis test was used for numeric variables with Bonferroni post hoc adjustment. A p value of <0.05 was considered significant. Sample size calculation was based upon previous publications.
Results
Demographic data
A total of 47 patients were recruited, and 45 patients (median age/IQR = 4 years/3.5) completed 6 months of follow-up with 15 patients in each group. Two patients were lost to follow-up after surgery. 25 (55.6%) were females. 29 (64.4%) were on the right side. There was no statistically significant difference between the three groups regarding age, gender, side of operation, the size of the cyst, or the site of the cyst. The demographic data and baseline characteristics are shown in Table 1.
Operative time
Median/IQR operative time for Group C was significantly shorter (10/5 min) compared with group A (25/10 min), and B (35/20 min) (p < 0.001) (Table 1). For cysts inside the rim, operative time was comparable in groups B (15/0 min) and C (15/5 min) and significantly longer in group A (25/14 min). For cysts outside the rim, duration of surgery was significantly longer in Group B (40/10 min) compared with group A (20/10 min) and C (10/5 min).
Within group B, operative time for cysts outside the rim (median/IQR; 40/10 min) was significantly longer compared to that of cysts inside the rim (median/IQR; 15/5 min) (p = 0.003).
Objective scar visibility (patient’s eyes open)
Kappa test was utilized to check the agreement of scar visibility grading between the two observers, which showed the following: at 1 month (0.444), 3 months (0.748), and 12 months (0.638). Median (IQR) scar visibility grade of group A by the 2 observers at 1, 3, and 6 months was 3.0 (0), 2.5 (1), and 2.0 (0.5) respectively. Median (IQR) scar visibility grade of group B by the 2 observers at 1, 3, and 6 months was 1.0 (0.5), 1.0 (0), and 1.0 (0) respectively. Median (IQR) scar grade of group C by the two observers at 1, 3, and 6 months was 2.5 (0), 2.0 (0), and 1 (0.5) respectively. The scar visibility grades were compared between the three groups at 1, 3, and 6 months using Kruskal-Wallis test and showed that group A had significantly more visible scars compared with the other two groups at each follow-up (Table 2). The scars in group C were significantly more visible when compared with those in group B at 1 and 3 months (p value < 0.05), however this difference was not present at 6 months.
At the sixth month postoperatively, both observers were not able to recognize the side of surgery in all patients in group B. A significant improvement in scar visibility was noticed by the two observers in all groups at 3 months with no further improvement noticed among group A at 6 months (p value > 0.05).
Stony Brook Scar evaluation (patient’s eyes closed)
Kappa test was utilized to check the agreement of scar grading between the two observers, which showed the following agreement between them: at 1 month (0.554), 3 months (0.499), and 12 months (0.430) respectively.
Median (IQR) scar grade of group A by the 2 observers at 1, 3, and 6 months was 3.0 (1.5), 3.5 (1.5), and 4 (0.5) respectively. Median (IQR) scar grade of group B by the two observers at 1, 3, and 6 months was 5.0 (0.5), 5.0 (0.5), and 5.0 (1) respectively. Median (IQR) scar grade of group C by the two observers at 1, 3, and 6 months was 5.0 (1), 5.0 (1) and 5.0 (0.5) respectively. The scar grades were compared between the three groups at 1, 3, and 6 months using Kruskal-Wallis test. SBES was significantly worse in group C compared with the other two groups at each follow-up (p value < 0.05) with no significant difference detected between group B and C. There was a significant improvement in scar score among group A at 3 (both observers) and 6 (2nd observer) months, while there was no significant change in scar score among groups B and C at 3 and 6 months (p value > 0.05) (Table 2) (Fig. 2A–D).
A Left-sided sub-brow incision in a 4-year-old girl. The scar is moderately visible with hypopigmentaion and missing brow hair. B Right-sided sub-brow incision. The scar shows persistent erythema at 3 months. C, D Left-sided upper lid crease incision. At 3 months, the scar is invisible when the eye is open; still inconspicuous with the eye closed. E, F Direct mini-incision in two different patients. The scar is minimally visible at 1 (E) and 3 months (F).
Family’s questionnaire
In response to the first question regarding do you notice any scar at site of surgery from 2-foot distance, all families in group A (100%) answered yes compared to one family in group B (6.7%) and 10 families in group C (66.7%). This statistically significant difference was present at 4 and 6-foot distance as well. All families in group B (100%) found the scar excellent compared to 11 families in group C (40%) and six families in group A (73.3%). No family in group B stated that the scar was unacceptable, while four families in group A (26.7%) and one family in group C (6.7) did. To the question of whether the patient was bullied because of the scar, yes response was obtained from two families (13.3%) in group A compared to none in the other two groups (Table 3).
Complications
Intraoperative dermoid rupture occurred while dissecting them from periosteum in one patient in group A (6.7%) and two patients in group B (13.4%). After complete removal of the cyst wall, the site of the surgery was irrigated with steroid and antibiotic solution with no postoperative sequelae. Medial ptosis was noticed in one patient in group B (6.7%) that markedly improved at 6-month visit. Postoperative inflammation was noticed in two patients in group C, yet complete resolution occurred at 4 weeks with topical steroids. A persistent residual small mass without inflammation was present in one patient in group C at the end of follow-up; the parents refused any further intervention.
Discussion
In an esthetically oriented world, having an imperceptible skin scar is a major goal in all facial procedures. Prominent facial scars can seriously jeopardize the quality of life of many patients [20]. This applies to the conspicuous periocular area where scars are easily appreciated. It is well known that poor scar formation tends to occur in younger populations, areas of thick skin, and incisions perpendicular to relaxed skin tension lines [21]. Therefore, periorbital dermoid cyst surgery is a matter of substantial concern. Internal angular dermoid cysts pose added management challenges when compared to the more common external angular type. With a broad differential diagnosis for lesions in this region, including encephalocele, meningocele, haemangioma, lipoma and sebaceous cyst, multiple disease processes must first be ruled out [6,7,8]. Furthermore, important structures in the supero-medial quadrant of the orbit, such as the trochlea and superior oblique tendon may be at risk during the surgery [9]. Moreover, there is a higher risk of intraoperative rupture [10]. Finally, given its more conspicuous location, direct incisions inevitably leave significantly noticeable skin scars.
Several surgical techniques have been described for removing internal angular dermoid cysts [22]. An ideal technique allows optimum exposure while leaving minimal skin scarring. Traditionally, these cysts have been approached by incisions directly over the cyst, along the orbito-nasal groove (Lynch incision) or at the lower border of medial eyebrow [13, 22]. These direct techniques provide good surgical exposure and allow complete excision of the dermoid cyst. However, the cosmetic outcome may be unsatisfactory due to the resultant poor skin scars, possible webbing and brow hair loss [12, 14, 23]. Therefore, different surgical approaches have been developed to manage these esthetic concerns particularly in children [24]. An endoscopic assisted technique may be employed to avoid any facial scar [25,26,27]. Disadvantages of this procedure include the need for expensive devices, slow learning curve, relatively longer operative times, and unfamiliarity to oculoplastic surgeons [27,28,29,30,31]. Naik et al. [32] treated periorbital dermoids with foam sclerotherapy using sodium tetradecyl sulfate. Although their technique appears to be minimally invasive, postoperative residual mass and related asymmetry noticed in their photographs may be more objectionable than a skin scar. Moreover, recurrence, risk of malignant transformation, and the lack of histopathological confirmation remain of concern. Other authors [17] described evacuation of the dermoid cyst contents through a direct small wound followed by excision of its wall with resultant small scar.
An upper lid crease approach is not a new concept in periorbital dermoid surgery [33], however it is well reported in lateral cysts with scarce publications on its use for internal angular lesions. One main advantage is its familiarity to the oculoplastic surgeons with the ability to perform the dissection between the cyst and the vital lid structures safely [12, 33].
In this study, we compared three techniques for removing internal angular dermoid cysts; the sub-brow, the lid crease, and the direct mini-incision. In terms of cosmetic outcomes, the lid crease and direct mini-incision approaches showed superior scar quality by SBSES when compared with the sub-brow approach. Both the lid crease and the direct incisions were made in the thin eyelid skin parallel to the relaxed skin tension lines, which are known to heal rapidly, leaving fine final scars. On the other hand, in the sub-brow group, the incisions were made in the thick brow skin leaving depressed scars with prolonged discoloration [11, 16, 22, 34].
With the patients’ eyes open, the lid crease group had the least visible scar. The reason for this is that the upper lid fold overlaps the lid crease concealing the incision site [11, 12]. In the direct mini-incision group, the minimum length of the incision makes the scar inconspicuous over time [34]. Conversely, the sub-brow group experienced the most noticeable scar which can be attributed to the poor scar quality, missing brow hair in the scar area and the conspicuous location of the incision.
Köse and Okur [23] compared the lid crease approach with direct excision for lateral dermoid cysts. The cosmetic results were comparable for adults, however, the lid crease showed better results in children. Cozzi et al. [14] reported better scar quality with the lid crease approach in a study comparing 26 patients, who underwent a trans-brow incision, with eight patients, who underwent lid crease incision for lateral angular dermoid cysts. In contrast to our results, Gur et al. [13] reported good esthetic outcomes following excision of angular dermoid cysts through incisions camouflaged in the eyebrow. It is thought that lateral brow incisions can leave an acceptable scar, although when the incision is carried more medially the scar can become considerably more noticeable.
With regards to the operative time, the lid crease group had the longest operation time, and the direct mini-incision technique was associated with the shortest time. The majority of the cysts encountered in the present study were located anteriorly outside the rim, for which we experienced some difficulties with the lid crease approach with resultant increase of the operative time. Cyst exposure is hindered by the limited distensibility of the medial lid caused by the deep attachment of the orbicularis muscle at the medial canthus and the immobility of the cysts. Additionally, cyst dissection can be tricky as the cyst is found to be adherent to the overlying dermis in addition to the deep periosteal attachment along with the increased distance between the cyst and the incision. However, the lid crease incision provides a more direct approach for more posterior cysts lying inside the rim and minimal dissection. In addition, the cysts can be easily dissected from the surrounding orbital fat and adjacent levator aponeurosis [11, 12, 35].
The duration of surgery in the sub-brow group was relatively longer than previously reported for lateral dermoid cysts [23]. This can be explained by the fact that the medial sub-brow incision is less direct to the inferiorly located medial cysts when compared to the frontozygomatic dermoid cysts located closer to the eyebrow. Therefore, more dissection is required for adequate exposure with increased operative time.
In the mini-incision group, the technique allows direct access to the cyst and no much time is needed for careful dissection around the cyst. Dissection was only needed to remove the wall, therefore minimizing operation duration.
Nelson et al. [15] report their average operating time for excision through the lid crease as 30 min. Gur et al. [13] report 25 min for direct excision through eyebrow incision [13]. The average time in Köse and Okur [23] was 20 min for direct excision versus 24 min for the lid crease. Steele et al. [29] report 50.5 min for endoscopic excision. Lee et al. [30] described an endoscopic approach for nasoglabellar dermoid cysts with a much longer operative time (1.5 to 2 h).
In our study, only six families in the sub-brow group graded the scar as excellent compared with 11 families in the direct mini-incision group and all families in the lid crease group. Additionally, no family in the three groups reported any negative social impact on their child. In contrast, a high proportion of the families in the Gur et al. study [13], describing the results of the conventional techniques for lateral dermoid cysts, reported the scar as excellent and no family stated that the scar was unacceptable. All parents in the Köse and Okur [23] study were satisfied with the cosmetic results in the lid crease and the direct incision group, although scars were more noticeable in children compared to adults. In the Cozzi et al. [14] study, comparing the lid crease approach with the direct technique for lateral brow dermoid cysts, all families of the 34 study patients reported great satisfaction and an excellent scar. This discrepancy between the previous results and our results can be explained by the assumption that medial brow scars are more conspicuous than lateral ones.
Intraoperative cyst rupture occurred inadvertently in a minority of cases in the lid crease and the sub-brow groups (aiming for excision in-toto) with no sequelae during the follow-up period.
The postoperative follow-up period passed uneventfully for the majority of patients in the direct mini-incision group, except for three patients. Two patients experienced prolonged postoperative inflammation that resolved completely at the third follow-up visit with topical medications only. This is may be related to keratin dispersed into the surgical field. Residual mass occurred in one patient that has shrunk to a small size at the end of the follow-up, for which the parents declined any further intervention. The exact pathology of this mass was not identified, as no histopathology was performed.
Limitations of the study include the small numbers in each group. Furthermore, longer follow-up period is needed to watch for any recurrence in the direct mini-incision technique.
Conclusion
The sub-brow approach is associated with the poorest esthetic outcome while both the eyelid crease and the direct mini-incision are associated with far better cosmetic results. Moreover, the direct mini-incision has the shortest operative time, whereas the eyelid crease approach has the longest operative time particularly for cysts outside the rim.
Summary
What was known before
-
Angular dermoid cysts can be removed through an incision camouflaged in the lid crease or along the brow hair.
What this study adds
-
Internal angular dermoid cysts can be separated into cysts inside and outside the orbital rim by location.
-
Internal angular dermoids can be safely removed through a direct minimum incision after evacuation of its contents.
-
Both the lid crease and the direct mini-incision approaches have superior scar quality with minimum visibility compared with the sub-brow technique.
-
The lid crease approach is associated with a prolonged operation time particularly for cysts outside the rim, while the direct mini-incision has the shortest operative time.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
19 January 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41433-021-01915-1
References
Shields JA, Shields CL. Orbital cysts of childhood-classification, clinical features, and management. Surv Ophthalmol. 2004;49:281–99.
Sherman RP, Rootman J, Lapointe JS. Orbital dermoids: clinical presentation and management. Br J Ophthalmol. 1984;68:642–52.
Cavazza S, Laffi GL, Lodi L, Gasparrini E, Tassinari G. Orbital dermoid cyst of childhood: clinical pathologic findings, classification and management. Int Ophthalmol. 2011;31:93–7.
Bajric J, Griepentrog GJ, Mohney BG. Pediatric periocular dermoid cysts: incidence, clinical characteristics, and surgical outcomes. Ophthalmic Epidemiol. 2019;26:117–20.
Shields JA, Kaden IH, Eagle RC Jr, Shields CL. Orbital dermoid cysts: clinicopathologic correlations, classification, and management. The 1997 Josephine E. Schueler Lecture. Ophthalmic Plast Reconstr Surg. 1997;13:265–76.
Sekaran P, Brindley N. B2 External and internal angular dermoid cyst. In Basic techniques in pediatric surgery: 125–7. Heidelberg: Springer, Berlin; 2013.
Al-Muhaylib A, Alkatan HM, Al-Faky YH, Alsuhaibani AH. Periorbital lesions misdiagnosed as dermoid cysts. J AAPOS. 2017;21:509–11.
Pushker N, Meel R, Kumar A, Kashyap S, Sen S, Bajaj MS. Orbital and periorbital dermoid/epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol. 2020;55:167–71.
Kushner BJ, Jethani JN. Superior oblique tendon damage resulting from eyelid surgery. Am J Ophthalmol. 2007;144:943–8.
Lenci LT, Shams P, Shriver EM, Allen RC. Dermoid cysts: clinical predictors of complex lesions and surgical complications. J AAPOS. 2017;21:44–7.
Ruszkowski A, Caouette-Laberge L, Bortoluzzi P, Egerszegi EP. Superior eyelid incision: an alternative approach for frontozygomatic dermoid cyst excision. Ann Plast Surg. 2000;44:591–4.
Kersten RC. The eyelid crease approach to superficial lateral dermoid cysts. J Pediatr Ophthalmol Strabismus. 1988;25:48–51.
Gur E, Drielsma R, Thomson HG. Angular dermoid cysts in the endoscopic era: retrospective analysis of aesthetic results using the direct, classic method. Plast Reconstr Surg. 2004;113:1324–9.
Cozzi DA, Mele E, d’Ambrosio G, Totonelli G, Frediani S, Spagnol L. The eyelid crease approach to angular dermoid cysts in pediatric general surgery. J Pediatr Surg. 2008;43:1502–6.
Nelson KE, Mishra A, Duncan C. Upper blepharoplasty approach to frontozygomatic dermoid cysts. J Craniofac Surg. 2011;22:e41–4.
Hachach-Haram N, Benyon S, Shanmugarajah K, Kirkpatrick WN. Back to basics: a case series of angular dermoid cyst excision. J Plast Reconstr Aesthet Surg. 2013;66:57–60.
El-Ghafar AA, ElKhair HA. Evacuation of dermoid cysts before excision. J Egypt Ophthalmol Soc. 2013;106:235.
Devoto MH, Zaffaroni MC, Bernardini FP, de Conciliis C. Postoperative evaluation of skin incision in external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2004;20:358–61.
Singer AJ, Arora B, Dagum A, Valentine S, Hollander JE. Development and validation of a novel scar evaluation scale. Plast Reconstr Surg. 2007;120:1892–7.
Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg. 2008;61:1049–58.
Carswell L, Borger J. Hypertrophic SCARRING KELoids. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020.
Kronish JW, Dortzbach RK. Upper eyelid crease surgical approach to dermoid and epidermoid cysts in children. Arch Ophthalmol. 1988;106:1625–7.
Kose R, Okur MI. Comparison of superior eyelid incision and directly over the lesion incision to brow dermoid cyst excision. Eur J Plast Surg. 2009;32:83–5.
Montolío-Marzo S, González-Valdivia H, Casas-Gimeno E, Sebastian-Chapman L, Prat-Bartomeu J. Dermoid cyst: outcome analysis in a pediatric referral hospital. Ophthalmic Plast Reconstr Surg. 2020;36:478–80.
Guerrissi JO. Endoscopic excision of frontozygomatic dermoid cysts. J Craniofac Surg. 2004;15:618–22.
Lopez M, Vermersch S, Varlet F. Endoscopic excision of forehead and eyebrow benign tumors in children. J Laparoendosc Adv Surg Tech A. 2016;26:226–30.
Kashkouli MB, Maleki M, Khademi B, Karimi N, Hamami P, Nadjafi-Semnani F. Endoscopic-assisted lateral orbitotomy for large orbital roof dermoid cysts with dural invasion. Ophthalmic Plast Reconstr Surg. 2020;36:508–11.
Huang MH, Cohen SR, Burstein FD, Simms CA. Endoscopic pediatric plastic surgery. Ann Plast Surg. 1997;38:1–8.
Steele MH, Suskind DL, Moses M, Kluka E, Liu DC. Orbitofacial masses in children: an endoscopic approach. Arch Otolaryngol Head Neck Surg. 2002;128:409–13.
Lee S, Taban M, Mancini R, Chong K, Goldberg RA, Douglas RS. Endoscopic removal of nasoglabellar dermoid cysts. Ophthalmic Plast Reconstr Surg. 2010;26:136–9.
Kose R. Excision of orbital dermoid cysts via upper eyelid incision: a review of 24 cases. J Curr Surg. 2014;4:110–2.
Naik MN, Batra J, Nair AG, Ali MJ, Kaliki S, Mishra DK. Foam sclerotherapy for periorbital dermoid cysts. Ophthalmic Plast Reconstr Surg. 2014;30:267–70.
Wolfley DE. The lid crease approach to the superomedial orbit. Ophthalmic Surg. 1985;16:652–6.
Dortzbach R, Woog JJ. Small-incision techniques in ophthalmic plastic surgery. Ophthalmic Surg. 1990;21:615–22.
Eldesouky MA, Elbakary MA. Orbital dermoid cyst: classification and its impact on surgical management. Semin Ophthalmol. 2018;33:170–4.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: DMM, EKB, ARC, AGAE; data collection: DMM, EKB; analysis and interpretation of results: DMM, EKB, ARC, AGAE; draft paper preparation: DMM, EKB. All authors reviewed the results and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: In part Objective scar visibility (patient’s eyes open) and part Stony Brook Scar evaluation (patient’s eyes closed) the Kruskal-Wallis test was named incorrectly as chi-square test.
Supplementary information
Rights and permissions
About this article
Cite this article
Diab, M.M., Allen, R.C., Abdel Ghafar, A.E. et al. Comparison of three surgical techniques for internal angular dermoid cysts: a randomized controlled trial. Eye 36, 2253–2259 (2022). https://doi.org/10.1038/s41433-021-01851-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01851-0