Running and exercise might be two of the best things women who have been diagnosed with PCOS—polycystic ovary syndrome—can do to improve symptoms.
PCOS is a common condition that affects 10 percent of women who are of childbearing age; they have a hormonal imbalance and metabolism problems that can lead to issues with overall health, fertility, and physical appearance, explains Christopher Morosky, M.D., M.S., associate professor of obstetrics and gynecology at the University of Connecticut School of Medicine.
Morosky, who has dubbed himself the Running Obstetrician, acknowledges that there is a lot of debate around how to diagnose PCOS, depending on which school of thought to which physicians subscribe, but he points out that the main hallmarks include irregular or absent periods, elevated androgen levels (like testosterone), and polycystic ovaries.
Join Runner's World+ for unlimited access to the best training tips for runners
Symptoms of PCOS
Morosky says that when patients make an appointment to see him it’s usually because of irregular or very heavy periods. The most common symptoms, according to the U.S. Department of Health and Human Services, of PCOS include:
- Irregular menstrual cycle, including fewer than eight periods per year or periods every 21 days or more frequently
- Amenorrhea (the absence of a period)
- Excessive hair growth on the face, chin, or parts of the body where men tend to have hair, also called hirsutism
- Acne on the face, chest, and upper back
- Thinning hair or hair loss; male-pattern baldness
- Weight gain or difficulty with weight loss
- Darkening of skin
- Excess flaps of skin in the armpit or neck, called skin tags
- Infertility
Causes and Risk Factors of PCOS
Like many medical conditions, it’s unclear the specific cause of PCOS, Morosky says.
“We know what causes a urinary tract infection and how to treat it,” he says. “Even in some cancers, like breast cancer, we know how it develops. But PCOS is a little harder to understand.”
What experts do know is there’s a problem with a woman’s hormones and ovaries—that problem is linked because hormones send signals to the ovaries for ovulation—as well as metabolism.
“We also know there is a strong relationship between PCOS and metabolic syndrome,” Morosky says.
Metabolic syndrome includes insulin resistance, prediabetes, borderline or high blood pressure, elevated triglycerides and cholesterol, and obesity.
“While the majority of people with PCOS are obese, it’s really important to point out that 20 percent of people with PCOS are not. But they still might be at risk for things like insulin resistance and cardiovascular complications,” he says.
PCOS, Morosky says, is a chicken-and-egg situation.
“Can they not lose weight with exercise because of PCOS or is the weight causing PCOS?” he says, pointing out there is an overlap between reproductive and metabolic hormones. “It’s hard to know where the problem lies.”
The same can be said for risk factors. Physicians often see patients with PCOS who also are at risk of or have type 2 diabetes, high blood pressure, obesity, excessive abdominal fat, and in some cases a family history of PCOS—there is no specific gene or genetic identification for the condition, however.
Diagnosis and Treatment
There isn’t one specific test for diagnosing PCOS, and some physicians use a different combination of symptoms or test results than others, Morosky explains, which can delay diagnosis and make things confusing.
Morosky will diagnose a person with PCOS if she checks two of three boxes, including irregular menstruation, elevated androgen levels (the most common being testosterone), and polycystic ovaries, which can be seen on an ultrasound.
“All criteria for diagnosing talk about the same thing, but who requires what can be confusing,” he says. “It all comes back to those three symptoms. If you have one of those things it doesn’t necessarily mean you have PCOS. If you have all three, it’s classic PCOS.”
PCOS is 100 percent treatable, Morosky says. Although he wouldn’t call it curable.
“Because it’s not well known what it is, how to diagnose it, and what causes it, we can’t say you’re cured,” he says. But there are treatments that can mitigate and even eradicate symptoms.
The first thing Morosky will advise his patients to do is start (or continue) exercising.
“Lifestyle modifications are the first treatments,” he says.
He doesn’t want to scare off patients who might not regularly exercise, so he sets the bar low, just to get them moving.
“For someone who’s doing nothing, 20 to 30 minutes three times a week is a lot to ask, and a patient might say, ‘I can’t meet that bar so I won’t,’” he says. “But one day of fitness is better than none, two is better than one, three is better than two.”
Adjusting eating habits is also an important and effective treatment, he says. He recommends people with PCOS substitute simple carbohydrates with complex ones, like beans and whole grains. And he emphasizes the importance of portion control and mindful eating, pointing out that runners with PCOS still need to fuel their activity.
PCOS and Running
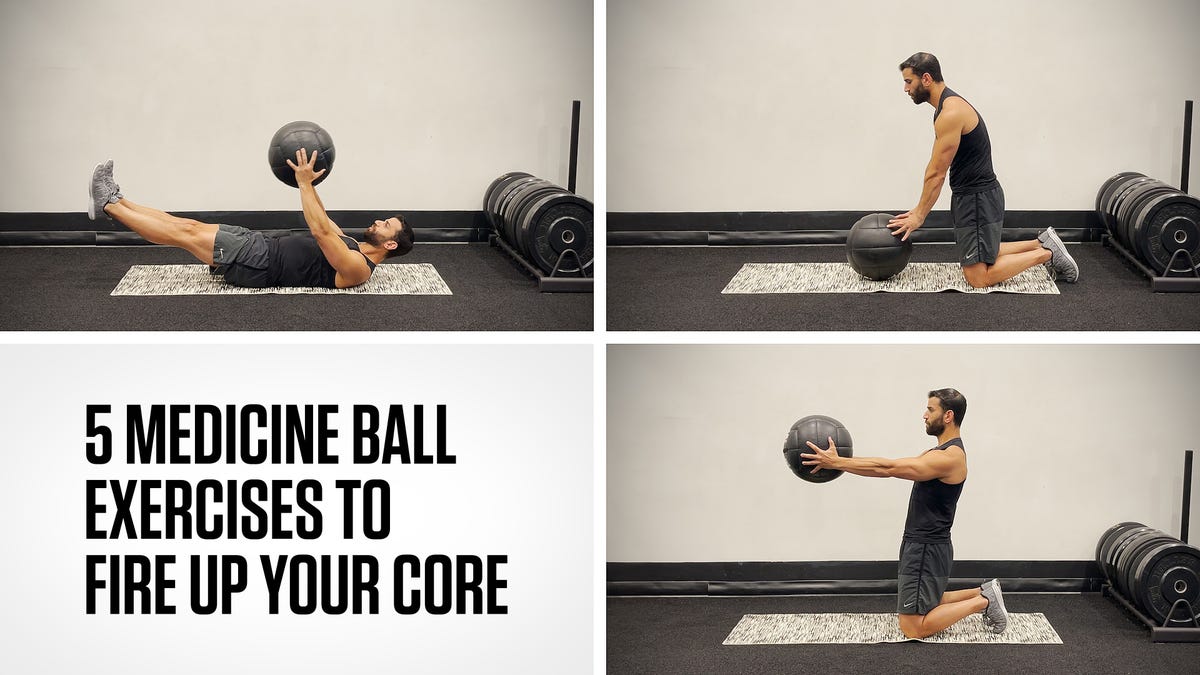
Regular exercise, whether that’s running, cycling, swimming, or walking, is one of the best things people with PCOS can do to help manage their symptoms.
“Exercise approaches PCOS in two specific ways,” Morosky says. “It decreases body fat and affects your metabolism.”
Excess body fat is a component of hormone imbalances seen with PCOS, he explains. “Body fat takes testosterone and turns it into weak estrogen, and that weak estrogen causes feedback to the brain, which can lead to not ovulating, a symptom of PCOS, for example.”
As for metabolism? People with PCOS often experience insulin resistance, which means they’re not burning glucose efficiently, and it then turns to fat. When you exercise, Morosky says, your body can start to use the energy from fat cells.
“Eventually, exercise will improve the metabolic problem with PCOS,” he says.
That said, some people with PCOS may exercise regularly, lose 10 pounds, and still not see symptom improvement, like the return of ovulation, says Meggie Smith, M.D., a reproductive endocrinology and infertility specialist at the Nashville Fertility Center.
“I don’t want anyone to think that it’s something they did wrong. Some people might not respond,” she says.
It’s worth noting that while running is one of the best things you can do to help manage PCOS, it’s important to keep your healthcare provider in the loop of your training, says Amanda Ulrich, M.D., assistant professor of obstetrics and gynecology at the University of Connecticut Health Center and associate program director of the Minimally Invasive Gynecologic Surgery Fellowship. That’s because PCOS causes enlarged ovaries—which is due to an excess number of follicles—and women can run the risk of an ovarian torsion—or the twisting of an ovary or fallopian tube—if they develop an ovarian cyst. During the time that the cyst is present and the ovary is enlarged, running may exacerbate the risk of the ovary twisting, Ulrich, a runner, explains.
Ultrasound imaging can help doctors and people with PCOS better evaluate the risk of ovarian torsion with exercise like running, Ulrich says. If you have PCOS and are experiencing symptoms such as nausea, vomiting, intense pelvic pain, or the inability to walk, you should go to the hospital right away, as you may have an ovarian torsion.
Is One Type of Exercise Better Than Another for Managing PCOS?
Yes and no.
“I tell my patients that the best exercise is the one you enjoy and do forever, whatever that looks like,” Morosky says.
Smith agrees: “I tell my patients to find something they enjoy. If they like it, the more likely they are to keep doing it.”
But scientifically speaking, exercise that can change a person’s body composition might bring the most benefit in terms of managing PCOS symptoms, she says, for example weight lifting or resistance training. Smith also recommends all women, regardless of whether they have PCOS, strength train and resistance train regularly to help improve bone health.
A study published in September in the Turkish Journal of Obstetrics and Gynecology looked at women with PCOS who were of “normal” body weight (as in, not overweight or obese) and found that they had lower aerobic capacity and muscle endurance than women who did not have PCOS.
The authors wrote that “the adverse metabolic profile of [PCOS] can limit physical function.”
Morosky calls the paper “interesting” but says more research is needed to determine what comes next.
“[PCOS] may affect how you work out, how your body uses oxygen, how your muscles are able to use energy when you’re working out,” he says. “But [the researchers] don’t go into much about what to do about this.”
The Bottom Line
While diagnosing PCOS can be tricky, it’s imperative that women who have symptoms work with a healthcare professional to diagnose the condition as early as possible. Smith points out that if a woman goes too long without ovulating—a symptom of PCOS—it could lead to endometrial cancer.
She also reiterates the importance of regular exercise—whether that’s running or something else—for women with PCOS, even if they’re not considered overweight or obese.
Morosky agrees: “Diet and exercise are the best tools against things associated with PCOS, like heart disease and difficulty getting pregnant.”
Heather is the former food and nutrition editor for Runner's World, the author of The Runner's World Vegetarian Cookbook, and a seven-time marathoner with a best of 3:31—but she is most proud of her 1:32 half, 19:40 5K, and 5:33 mile.