Addressing Vaccine Hesitancy Among Health Care Workers
Although there is no one-size-fits-all approach to promoting vaccine confidence, a conversation is a great starting point.
Oftentimes, when we think of vaccine hesitancy, we think about our patients. However, some health care workers express vaccine hesitancy, too. With several health care systems mandating COVID-19 vaccines, headlines include “New York Hospital to ‘Pause’ Delivering Babies After Staffers Quit Rather Than Get Vaccinated.”1 Yet, headlines don’t tell the whole story, and the issue of vaccine hesitancy certainly did not begin with the COVID-19 vaccine. How prevalent is vaccine hesitancy among health care workers? What are common reasons for hesitancy? How can we promote vaccine confidence among health care workers? Those are all questions worth answering, as research has found that health care workers who are vaccinated and have positive attitudes about vaccines are more likely to recommend vaccination to their patients and have higher patient rates of vaccination.2
VACCINE HESITANCY AMONG HEALTH CARE WORKERS
The rates of vaccine hesitancy vary by country, vaccine, and the type of health care worker. For example, the results of a systematic review and meta-analysis of international literature found that influenza vaccination rates reported in the literature vary greatly among health care providers: from approximately 33.1% in Turkey to less than 30% in Europe and nearly 98% in Australia.3,4 The United States often has higher rates of vaccination, including substantially higher influenza vaccination rates than Europe.3 Similar to influenza vaccination, there is quite a spread of COVID-19 vaccine acceptance in health care workers worldwide, ranging from 27.7% in Congo to 77.3% in the United States.4 In France, physicians and pharmacists had the highest intentions to receive a COVID-19 vaccine (92.1% and 88.8%, respectively), while nurses had lower intentions to receive the same vaccine (64.7%).5 Not surprisingly, most physicians and pharmacists have already been vaccinated against COVID-19 in both France and the United States. Approximately 96% of physicians and 88% of pharmacists in the United States have been reported as fully vaccinated.6,7 However, other US health care workers have much lower rates, ranging from 55% of nursing home staff, less than 50% to 56.7% of nurses, and 26% to 45.6% of home health aides are estimated to have received the COVID-19 vaccine.6,8 Rates of COVID-19 vaccination are highest in those working in hospitals or outpatient clinics (66% and 64%, respectively), with lower rates in medical offices (52%), nursing homes (50%), and in-home care (26%).9 Study results have shown that those who provide direct medical care are more likely to be accepting of the COVID-19 vaccine (ie, willing to be vaccinated themselves) than administrative staff and those who are not involved in direct patient care.10
So what can we glean from understanding the prevalence of vaccine hesitancy? Although we certainly do not understand the extent of vaccine hesitancy toward all vaccines, there remains a great deal of hesitancy among health care workers, particularly related to both the influenza and COVID-19 vaccines.
REASONS FOR VACCINE HESITANCY
What might prompt a health care worker, who interacts with those who have illness on a regular basis, to be vaccine hesitant? Much like our patients, there are multiple factors that may influence vaccine confidence among health care workers. Common reasons for vaccine hesitancy include:
- Lack of knowledge, misinformation, and doubts regarding vaccine efficacy and safety2,11,12
- Lack of support from colleagues and other social groups regarding vaccine efficacy and safety2
- Perceived benefits and risks of vaccination11,12
Although there may be a general understanding that vaccines are effective and safe among the medical community, not all health care workers have the same level of understanding regarding how a specific vaccine works, whether or not it is effective, and if it can be used safely.2 Lower knowledge of vaccine science is associated with lower vaccine confidence.2 Depending on the training of the health care worker regarding vaccines as well as the recency of the training, health care workers may not feel as confident with newer vaccines or understand how they have been formulated.2 For example, there are multiple components of vaccines (ie, antigens, stabilizers, adjuvants, preservatives), different adjuvants and preservatives utilized than in the past, and new mechanisms to promote immunity (ie, messenger RNA [mRNA] technology).13 A lack of familiarity and comfort with discussing these elements can contribute to a lack of confidence regarding vaccine efficacy and safety and leave health care workers feeling unprepared to engage in conversations with their patients.2
Health care workers also can have misperceptions or misinformation on how vaccines work. A systematic review found that 24% to 29% of those surveyed across several studies had incorrect knowledge regarding the influenza vaccine and the pertussis vaccine.11 Many also had doubts about the efficacy of the vaccines (2.5%-16%) and concerns about adverse effects (6%-25%).11 An incomplete understanding of the new mechanism introduced in the mRNA COVID-19 vaccines and the speed of its development can further contribute to concerns about efficacy and safety.9 Misperceptions such as these are a major contributor to low vaccination rates in nursing home staff.14
Furthermore, socialization can impact health care workers’ perceptions of vaccines. When friends and colleagues are hesitant about vaccine efficacy and safety, it can affirm the health care worker’s own hesitance or create dissonance with their own beliefs.2,12,15 These could be due to a variety of underlying beliefs, including the interplay of health, religion, politics, and government.15 Efforts to mandate vaccination may only result in further entrenchment within social groups,1,15 as evidenced by groups of health care workers quitting over recent COVID-19 vaccine mandates1 and a recent survey indicating 1 in 3 nurses would choose to quit if a vaccine were mandated.16 It is important to note that Black, indigenous, and people of color (BIPOC) groups have experienced many challenges, inequity, and misinformation from the health care system. Thus, some communities may have higher rates of distrust and negative perceptions of vaccines accordingly.14,17
Another reason for vaccine hesitancy could relate to perceived risks and benefits of vaccination. For example, health care workers, whether in community or hospital settings, can believe that they are already protected by the frequent exposure they receive to a multitude of viruses, particularly influenza.11 However, this can be thought of more broadly in terms of the health belief model, where the health care workers weigh out the perceived risks and benefits of vaccination.15 When health care workers believe that vaccinating themselves protects others (protects public health), see themselves as susceptible to the illness, or view vaccination as a necessity to avoid the severity of the disease, they are more likely to be vaccinated.11,15 (Similar factors impact health care workers’ recommendations to patients.12) If a virus or illness is perceived as low risk and/or a vaccination is perceived as a low benefit (eg, low efficacy),11,15 then health care workers are less likely to become vaccinated (eg, influenza).15
PROMOTING VACCINE CONFIDENCE
So how do we promote vaccine confidence among health care workers, particularly given the recent government mandate regarding COVID-19 vaccination among health care workers at most Medicare-and Medicaid-participating health care settings?18 The Figure outlines some key approaches to promote confidence.15,17,19,20
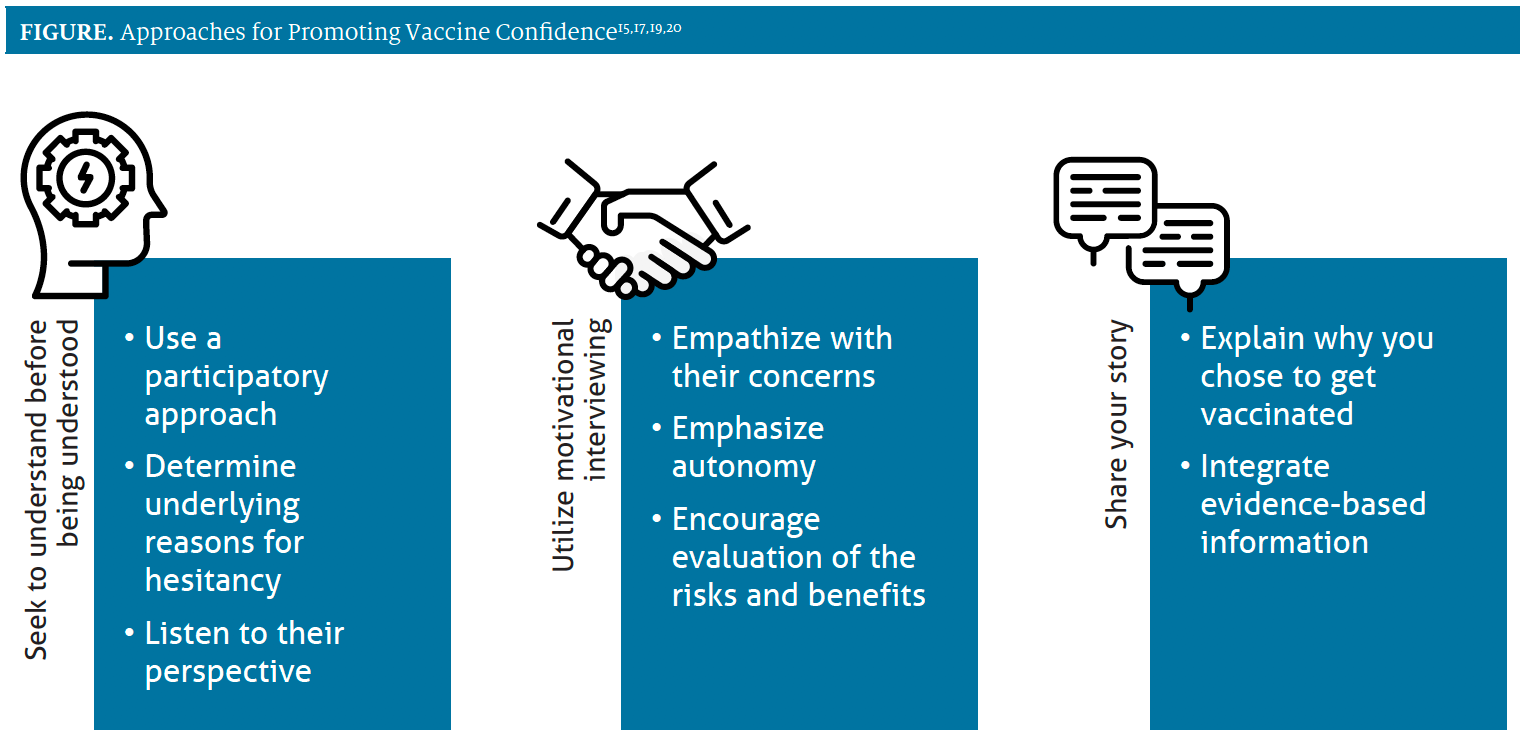
Although our initial response may be to provide education to address knowledge gaps, it’s important to first understand the health care worker’s perspective. Using open-ended questions with a participatory approach (eg, asking their thoughts on vaccination vs assuming they want to get vaccinated) are a starting point for the conversation. This is particularly important if we want to develop trust with other professionals who are from BIPOC communities.17 We should listen to their responses and identify any underlying reasons for hesitancy as well as any health beliefs. Once those are understood, we can utilize motivational interviewing, which is a patient-centered approach to communication that promotes trust.20 With this approach, we can empathize with our colleagues’ concerns about a vaccine, support their ability to make their own choices (autonomy), and encourage them to evaluate the risks and benefits of vaccination.20 Through the process of evaluating the risks and benefits of vaccination together, we can provide evidence-based information to address any misconceptions or misinformation and share our own stories of why we chose to receive a vaccine.20 In many cases, seeing someone else who is a health care worker who took the time to think through the evidence can promote confidence in a vaccine.14
Although there is no one-size-fits-all approach to promoting vaccine confidence, a conversation is a great starting point. Prepare yourself well for those conversations and spend some time ensuring that you know the evidence behind vaccine efficacy and safety.
Aleda M. H. Chen, PharmD, PhD, FAPhA, is the associate dean and an associate professor at the Cedarville University School of Pharmacy in Ohio.
Justin W. Cole, PharmD, BCPS, is the chair of pharmacy practice and an associate professor at the Cedarville University School of Pharmacy in Ohio.
REFERENCES
- Madani D. New York hospital to ‘pause’ delivering babies after staffers quit rather than get vaccine. NBC News. September 12, 2021. Accessed September 12, 2021. https://www.nbcnews.com/ news/us-news/new-york-hospital-pause-delivering-babies-after-staffers-quit-rather-n1279001
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700-6706. doi:10.1016/j.vaccine.2016.10.042
- Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. Hum Vaccin Immunother. 2018;14(3):772-789. doi:10.1080/21645515.2017.1348442
- Li M, Luo Y, Watson R, et al. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. Published online June 30, 2021. doi:10.1136/postgradmedj-2021-140195
- Gagneux-Brunon A, Detoc M, Bruel S, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168-173. doi:10.1016/j.jhin.2020.11.020
- Ezekiel J, Skorton DJ. Mandating COVID-19 vaccination for health care workers. Ann Intern Med. 2021;174(9):1308-1310. doi:10.7326/M21-3150
- Vast majority of pharmacists surveyed are fully vaccinated against COVID-19. American Pharmacists Association. May 24, 2021. Accessed September 12, 2021. https://www.pharmacist. com/APhA-Press-Releases/vast-majority-of-pharmacists-surveyed-are-fully-vaccinated-against-covid-19.
- Lee JT, Althomsons SP, Wu H, et al. Disparities in COVID-19 vaccination coverage among health care personnel working in long-term care facilities, by job category, National Healthcare Safety Network - United States, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(30):1036-1039. doi:10.15585/mmwr.mm7030a2
- KFF/The Washington Post frontline health care workers: The Washington Post/KFF survey project. Kaiser Family Foundation. March 2021. Accessed September 12, 2021. https://files.kff.org/attachment/ Frontline%20Health%20Care%20Workers_Full%20Report_FINAL.pdf
- Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel). 2021;9(2):119. doi:10.3390/vaccines9020119
- Collange F, Verger P, Launay O, Pulcini C. Knowledge, attitudes, beliefs and behaviors of general practitioners/family physicians toward their own vaccination: a systematic review. Hum Vaccin Immunother. 2016;12(5):1282-1292. doi:10.1080/21645515.2015.1138024
- Lin C, Mullen J, Smith D, Kotarba M, Kaplan SJ, Tu P. Healthcare providers’ vaccine perceptions, hesitancy, and recommendation to patients: a systematic review. Vaccines (Basel). 2021;9(7):713. doi:10.3390/vaccines9070713
- What’s in vaccines? CDC. August 5, 2019. Accessed September 12, 2021. https://www.cdc.gov/vaccines/vac-gen/additives.htm
- Harrison J, Berry S, Mor V, Gifford D. “Somebody like me”: understanding COVID-19 vaccine hesitancy among staff in skilled nursing facilities. J Am Med Dir Assoc. 2021;22(6):1133- 1137. doi:10.1016/j.jamda.2021.03.012
- To KW, Lai A, Lee KC, Koh D, Lee SS. Increasing the coverage of influenza vaccination in healthcare workers: review of challenges and solutions. J Hosp Infect. 2016;94(2):133-142. doi:10.1016/j.jhin.2016.07.003
- Mitchell H. 30% of nurses would quit over vaccine mandate, Ohio union says. Becker’s Hospital Review. September 2, 2021. Accessed September 12, 2021. https://www.beckershospital review.com/workforce/30-of-nurses-would-quit-over-vaccine-mandate-ohio-union-says.html
- Quinn SC, Andrasik MP. Addressing vaccine hesitancy in BIPOC communities - toward trustworthiness, partnership, and reciprocity. New Engl J Med. 2021;385(2):97. doi:10.1056/NEJMp2103104
- Path out of the pandemic: President Biden’s COVID-19 action plan. The White House. Accessed September 12, 2021. https://www.whitehouse.gov/covidplan/
- COVID-19 vaccine confidence project executive summary. Reagan-Udall Foundation for the FDA. December 15, 2020. Accessed September 22, 2021. https://reaganudall.org/sites/ default/files/2020-12/Vaccine%20Confidence%20Project%20 Findings%20for%20Public%20Distribution%20121820.pdf
- Talking with patients about COVID-19 vaccination: an introduction to motivational interviewing for healthcare professionals. CDC. Accessed September 19, 2021. https://www.cdc.gov/ vaccines/covid-19/hcp/engaging-patients.html