Lonsurf/Bevacizumab Does Not Prolong PFS Over Capecitabine/Bevacizumab in mCRC
The primary end point of the phase 3 SOLSTICE study of trifluridine and tipiracil plus bevicizumab versus capecitabine and bevacizumab in patients with unresectable metastatic colorectal cancer was not met.
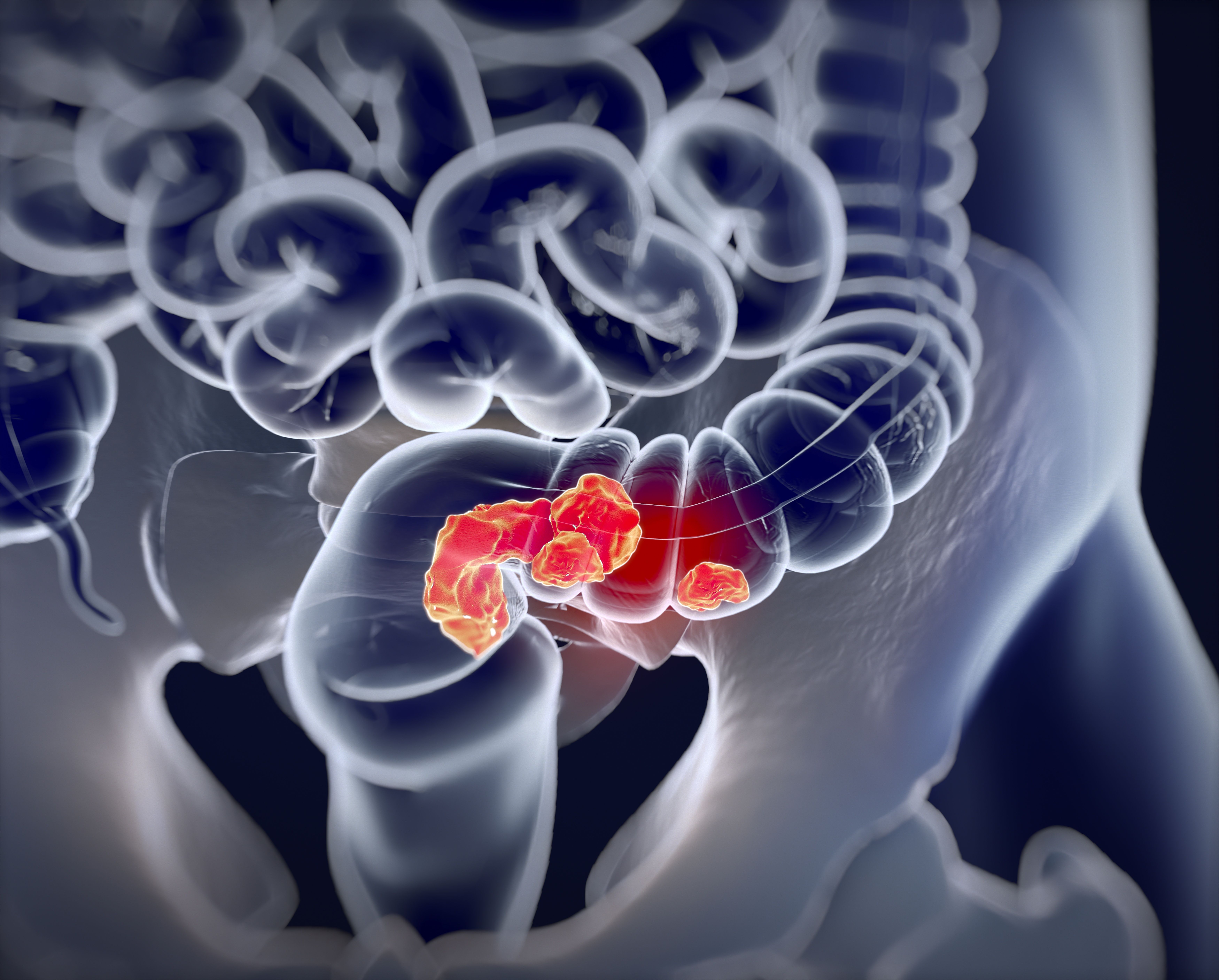
The frontline combination of trifluridine and tipiracil (Lonsurf) with bevacizumab (Avastin) did not demonstrate improvement in progression-free survival (PFS) compared with frontline capecitabine and bevacizumab in patients with unresectable metastatic colorectal cancer (mCRC) ineligible for intensive therapy, according to a press release issued by Servier.1
The primary end point of the study was not met but considering that no serious safety concerns have been observed in either treatment arm, the study will continue as planned.
Primary analysis data will also be presented at an upcoming medical meeting.
"Metastatic colorectal cancer patients who are not well enough to undergo intensive chemotherapy have limited options, and quality of life is a priority," said Thierry André, MD, a professor at Saint Antoine Hospital, in Paris, France, and the lead investigator for the SOLSTICE study, in the press release. "We are continuously searching for new ways to give these patients efficient treatment with low toxicities."
SOLSTICE (NCT03869892) is an open-label, randomized phase 3 study of approximately 856 patients with unresectable mCRC who are not candidates for intensive therapy. Patients were enrolled at 200 sites across 35 countries. The study was conducted based on phase 2 research showing promising anti-tumor activity was demonstrated with trifluridine and tipiracil plus bevacizumab in patients who were ineligible for treatment with oxaliplatin or irinotecan-based chemotherapy.2
In SOLSTICE, the secondary end points were overall survival (OS), objective response rate, disease control rate, duration of response, safety/tolerability, and quality of life (QOL). As an exploratory end point, the efficacy of trifluridine and tipiracil plus bevacizumab versus capecitabine and bevacizumab was investigated in patients with RAS, BRAF 600E-positive tumors, as well as based on patients’ mismatch repair status.
In a 1:1 ratio, 427 patients were randomized to receive trifluridine plus tipiracil 35 mg/m2 twice daily. Trifluridine and tipiracil were administered on days 1 through 5 and days 8 through 13 for 4 weeks and combined with bevacizumab 5 mg/kg administered intravenously on days 1 and 15. In the control arm, the other 427 patients received capecitabine at 1250 or 1000 mg/m2 twice daily on days 1 through 14 every 3 weeks in combination with bevacizumab 7.5 mg/kg administered on day 1 every 3 weeks.
The starting dose of capecitabine in the control arm was at the investigators’ discretion. All treatment in the study continued until radiologic or clinical disease progression, unacceptable toxicity, conversion to resectable mCRC, or another reason.
To conduct analyses in the study, patients were stratified by ECOG performance score, tumor localization, and the reason they are ineligible for intensive therapy.2 Per the inclusion criteria patients were required to have a histologically confirmed adenocarcinoma of the colon or rectum, an ECOG performance score of ≤ 2, and adequate organ function. Patients could not have received prior systemic anticancer therapy for unresectable mCRC and could not be candidates for the full dose chemotherapy combination of irinotecan or oxaliplatin or curative resection. RAS status for any patient must have been available in order for the patient to enroll.3
Driven by the primary end point of investigator-assessed PFS, the study was 90% powered to detect an improvement with a hazard ratio (HR) of 0.77 using a log-rank test. Investigators also projected a 2.5 level significance according to a 2-look group sequential design at one-sided cumulative evaluation.
The expected median duration of PFS was 9.7 months with the experimental combination trifluridine and tipiracil with bevacizumab compared with 7.5 months with the combination oof capecitabine and bevacizumab.
SOLSTICE was also 80% powered to detect an improvement in OS was trifluridine and tipiracil with bevacizumab versus the control combination with an HR of 0.79. Further, the other study end points will be determined using Fisher’s exact test and Clopper–Pearson confidence intervals, or a Kaplan-Meier analysis. Descriptive statistics in each treatment arm will also be assessed to determine safety and QOL measures.
"We remain committed to improving outcomes in mCRC and we will continue to follow patients as planned in order to perform the main secondary end point analysis on overall survival in 2023," said Patrick Therasse, MD, PhD, head of Late Stage and Life Cycle Management, and deputy head Oncology and Immuno-Oncology Therapeutic Area, at Servier, in the press release.1 "The clinical value of Lonsurf in its current indications remains unchanged, and the ongoing phase 3 SUNLIGHT trial [Lonsurf plus bevacizumab versus Lonsurf in third-line mCRC] is proceeding as planned."
References:
1. Servier announces outcome from the primary analysis of the Phase III SOLSTICE trial assessing LONSURF® (trifluridine/tipiracil) + bevacizumab in a 1st line setting for patients with unresectable mCRC non-eligible for intensive therapy. News release. Servier. October 22, 2021. Accessed October 22, 2022. https://bwnews.pr/3GaDDBk
2. Andre T, Saunders M, Kanekisa A, et al. First-line trifluridine/tipiracil plus bevacizumab for unresectable metastatic colorectal cancer: SOLSTICE study design. Future Oncol. 2020;16(4);21-29. doi: 10.2217/fon-2019-0786.
3. Phase III study in first-line treatment of patients with metastatic colorectal cancer who are not candidate for intensive therapy. (SOLSTICE). Clinicaltrials.gov. Accessed October 22, 2021. https://bit.ly/3b0lGa2
Retrospective Data Demonstrates Efficacy of Regorafenib in mCRC
April 16th 2024During a Case-Based Roundtable® event, Madappa Kundranda, MD, PhD, discussed recent retrospective studies that compared outcomes between the available treatment options in patients with relapsed/refractory advanced colorectal cancer in the first article of a 2-part series.
Read More
Peritoneal RFS May Be a Stronger Predictor of OS in CRC Peritoneal Metastasis
March 27th 2024In an interview with Targeted Oncology, Muhammad Talha Waheed, MBBS, discussed research on the reliability of using recurrence-free survival as an efficacy end point for trials evaluating patients with colorectal cancer peritoneal metastasis.
Read More
Study Finds Susceptibility Gene Variations by Race/Ethnicity in Early-Onset CRC
February 20th 2024In an interview with Targeted Oncology, Andreana N. Holowatyj, PhD, MSCI, discussed data from a study which found racial and ethnic differences in susceptibility genes for early-onset colorectal cancer, suggesting current multigene panel tests may not be accurate for diverse populations.
Read More