Abstract
Gamma-aminobutyric acid (GABA) metabolism is implicated in posttraumatic stress disorder (PTSD) and may be altered in prefrontal-limbic brain regions involved in arousal regulation. This study used proton magnetic resonance spectroscopy (MRS) to test the hypothesis that PTSD and trauma-exposed non-PTSD comparison (TENC) adults have significantly different GABA than healthy comparison (HC) subjects in two brain areas implicated in arousal (medial prefrontal cortex, insula) but not in a control brain area (posterior temporal cortex). We also examined whether GABA alterations correlated with hyperarousal and dissociation symptoms. One hundred and fourteen participants (39 PTSD, 34 TENC, 41 HC) underwent 3T MRS of the medial prefrontal, right insular, and right posterior temporal cortices, and the GABA plus macromolecule signal (GABA+) was normalized to creatine (Cr). The Clinician Administered PTSD Scale measured hyperarousal symptoms, including sleep disruption. The Dissociative Experiences Scale assessed dissociation symptoms. PTSD and TENC participants had significantly lower mPFC GABA+/Cr than HC participants, and this deficit was significantly correlated with greater dissociation. Compared with HC, PTSD patients but not TENC had significantly lower insula GABA+/Cr. Total hyperarousal symptoms and sleep disruption were not significantly associated with GABA+/Cr alterations in either region. Our findings point to lower GABA in cortical areas implicated in arousal regulation in PTSD and suggest that GABA alterations are associated with symptoms of trauma-related psychopathology but not always a biomarker of diagnosis. These findings also add to evidence that dissociation has distinct neural correlates within PTSD, including high excitability of medial prefrontal cortex.
Similar content being viewed by others
Introduction
Gamma-aminobutyric (GABA) metabolism is implicated in behaviors and physiological processes that are associated with posttraumatic stress disorder (PTSD; [1,2,3,4]). Preclinical studies have shown that GABA agonists inhibit hyperarousal states, including the startle response induced by predator stress [5]. Fear learning is associated with morphological and functional adaptations of inhibitory GABA neurons within the medial prefrontal cortex (mPFC) and amygdala, and these changes modulate arousal level, fear learning, and threat detection sensitivity [6, 7]. Medications that potentiate GABA — including gabapentin [8], tiagebin [9], pregabalin, and baclofen [10, 11] — have shown some efficacy for PTSD either as standalone or adjunctive therapies [11, 12]. Consistent with evidence that these GABA agonists attenuate arousal in rodents, they improve hyperarousal symptoms of PTSD, including insomnia [8, 10,11,12]. Altogether, these lines of research suggest that GABAergic alterations in mPFC-limbic regions are associated with PTSD and may be relevant to alterations in arousal.
Proton magnetic resonance spectroscopy (MRS) allows detection of brain GABA in vivo and can therefore probe GABA involvement in behaviors and diagnosed conditions. Measurement of GABA has historically been challenging because of its low concentration in the brain and its overlap with more prominent metabolite peaks in the proton spectrum. However, advances in spectral acquisition methods, such as the widely used MEGAPRESS (MEGA-Point REsolved Spectroscopy Sequence), have greatly improved reliable estimation of brain GABA levels [13]. MEGAPRESS is an imaging sequence that selectively isolates or “edits” the GABA signal within the MRS spectrum [14]. Our research group and others have implemented MRS spectral editing methods to measure regional brain GABA in medial prefrontal-limbic brain areas associated with psychiatric illness (e.g. [15,16,17,18,19]).
A handful of studies have examined GABA levels in PTSD, and their findings vary across brain regions. In an early investigation, our laboratory reported that GABA in the right anterior insula, but not dorsal anterior cingulate cortex (ACC), was significantly lower in 13 patients with civilian-based PTSD than in 13 age- and sex-matched, non-traumatized healthy participants [20]. A subsequent investigation of dorsal ACC GABA found that a group of 27 veterans with PTSD and a group of 18 veterans without PTSD both had significantly lower dorsal ACC GABA than 28 non-traumatized controls [21], suggesting that combat exposure but not PTSD diagnosis is associated with low ACC GABA. Another research group conducted two MRS investigations of GABA in the medial temporal cortex of PTSD patients relative to trauma-exposed non-PTSD (TENC) subjects, and found lower GABA associated with PTSD in one study [22] but not in the other [23]. Thus far, only one prior study has reported elevated cortical GABA in PTSD [24] namely, higher GABA in the rostral ACC and left dorsolateral prefrontal cortex of 12 PTSD patients compared with 17 TENC. Altogether, this evidence suggests that brain GABA is altered in PTSD, and that there may be regional differences in the presence and nature of these alterations.
There is also growing evidence of different PTSD symptom correlates of GABA alterations depending on the brain region, consistent with involvement of GABA metabolism in multiple physiological processes and behaviors relevant to PTSD. One study found that insomnia was associated with significantly lower GABA in the parieto-occipital cortex of patients with PTSD, but not with GABA in the medial temporal cortex [22]. Similarly, Sheth and colleagues [21] found that greater sleep impairment correlated with lower dorsal ACC GABA levels in PTSD patients. Comorbidities including substance use disorders and depression may also contribute to variability in GABA within PTSD. Pennington and colleagues [23] found that PTSD patients with comorbid alcohol use disorder had similar GABA levels in parieto-occipital and temporal cortices as healthy participants, whereas PTSD patients without alcohol use disorder showed significantly lower GABA levels than healthy controls in both regions. These findings converge with other evidence that excessive use of drugs, including alcohol and nicotine, can affect GABA activity [25,26,27]. Regarding depression, a meta-analysis of MRS GABA studies concluded that cortical GABA is lower in current (but not remitted) major depressive disorder [28].
The evidence reviewed above points to the importance of identifying regional brain GABA alterations in PTSD, and of determining their potential relevance to alterations in arousal, while accounting for effects of comorbidity. In this study, we compared GABA levels between adults with PTSD, TENC subjects, and non-traumatized healthy comparison (HC) subjects. We focused on two prefrontal-limbic brain areas that have been implicated in PTSD and modulation of arousal (mPFC, right insula), and on one control brain area (right posterior temporal cortex) that has not been centrally implicated in either PTSD or arousal. Relative to HC, the PTSD and TENC groups were predicted to show significant differences in mPFC and insula GABA but not in temporal cortex GABA. To examine the specificity of GABA differences, we also compared the groups on N-acetyl aspartate (NAA), an index of neuronal integrity. Finally, we hypothesized that GABA alterations detected in insula and mPFC would correlate with symptoms of excessive arousal (hyperarousal, including disrupted sleep) or attenuated arousal (dissociation).
Materials and methods
Participants
We recruited 126 participants (ages 18–50) via advertisements in the local community. All subjects provided written informed consent after receiving a full explanation of study procedures and were compensated for participating. Study procedures were approved by the Partners Human Research Committee. Our analyzed sample was 114 participants consisting of 39 adults with DSM-IV PTSD, 34 TENC adults with subthreshold symptoms, and 41 HC subjects with no history of DSM-IV Axis I disorder or Criterion A trauma exposure. This sample was defined after excluding: three participants for clinical neuroradiologic abnormalities; two for excessive head movement; two for claustrophobia; one for missing MRS data; one for inconsistent reporting precluding group assignment; two for left-handedness; one for current cannabis abuse. Selection criteria are detailed in the Supplement.
Doctoral-level psychologists administered the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) to all participants, and the Clinician Administered PTSD Scale for DSM-IV (CAPS) to PTSD and TENC participants. Based on the CAPS, 23 PTSD participants met criteria for current PTSD and 16 for lifetime PTSD with currently subthreshold symptoms. TENC participants endorsed a history of DSM-IV Criterion A trauma exposure and had never met criteria for more than one PTSD symptom cluster.
Depressive disorders were the most common comorbid conditions in the PTSD group (MDD, 12; dysthymic disorder, two; Depression not otherwise specified ((NOS), one), and in the TENC group (MDD, one; dysthymic disorder, one; depression NOS, one). One PTSD participant was taking a selective serotonin reuptake inhibitor (stable dose for ≥8 weeks). No other participants were taking psychotropic medication. Information on Axis I psychiatric comorbidities and index traumas is in the Supplement.
Interview and self-report measures
Life Experiences Checklist (LEC; [29])
All participants completed the LEC, a self-report questionnaire of exposure to 16 potentially traumatic life events. LEC score was derived as a measure of lifetime trauma load (number of traumas directly experienced plus number directly witnessed). Participants who checked one or more LEC items were asked follow-up questions by a clinician to determine whether any corresponded to a Criterion A trauma.
CAPS [30]
Participants with one or more LEC items meeting Criterion A (A1 and A2) for PTSD were administered the CAPS to determine assignment to PTSD and TENC groups. The CAPS also was used to calculate PTSD total symptom and subscale scores (Table 1). Sleep disruption scores were the sum of CAPS item B2 (distressing dreams) and CAPS item D1 (difficulty falling or staying asleep). CAPS “hyperarousal–” scores were the sum of all D cluster items, except for D1.
Beck Depression Inventory, Version 1a (BDI; [31])
BDI total score was used as a measure of depression symptom severity.
Dissociative Experiences Scale, 2nd version (DES; [32])
DES total score was derived as a measure of dissociation symptom severity.
Assessment of alcohol and nicotine use
Participants were asked to refrain from alcohol use for at least 24 h prior to their study visit and were queried about their most recent consumption of alcohol during their visit. Because chronic use or dependence on alcohol or nicotine affects GABA, participants were excluded for alcohol abuse in the past year or dependence in the past five years, as assessed with the SCID. To assess nicotine use disorder [25], we administered the Fagerström Test for Nicotine Dependence (FTND) to participants who endorsed regular nicotine use [33]. Five PTSD and two TENC participants were nicotine dependent (PTSD: two very dependent, three moderately dependent; TENC: one very dependent, one moderately dependent; Χ2 (df = 2) = 2.27, p = 0.32).
Menstrual and birth control questionnaire
Female participants provided information on their menstrual cycle, days since last menstruation, and use of hormonal contraceptives (Supplement).
Magnetic resonance imaging and spectroscopy
Acquisition
Imaging was conducted at McLean Hospital on a 3 T Siemens Tim TRIO, whole-body, MR scanner using a 32-channel phased-array design radiofrequency head coil operating at 123 MHz. Participants were positioned inside the coil with lateral padding to minimize head movement. A three-plane series of scout images confirmed optimal head positioning. High-resolution T1 anatomic images then were acquired using the following parameters: 128 slices, 256 × 256 matrix, echo time = 3.31 ms; repetition time = 2530 ms; inversion time = 1100 ms; flip = 7°, slice thickness = 1.33 mm). These structural images were used to position the MRS voxels.
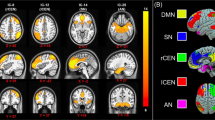
MRS voxel positioning
The same investigator (JEJ) positioned all voxels for all participants using internal anatomical landmarks. A 2.5 × 2.5 × 3 cm3 mPFC voxel was centered on the midline in the axial plane and on the tip of the corpus callosum in the sagittal plane (Fig. 1). The posterior edge of the mPFC voxel abutted but did not include corpus callosum. This voxel contains mostly gray matter of rostral anterior cingulate gyrus (Brodman area (BA) 32 and 24). A similar voxel has been labeled in prior studies as anterior cingulate cortex [15], medial prefrontal [34], or ventromedial prefrontal cortex [17, 35].
(A) medial prefrontal cortex (MPFC), (B) right anterior insula, and (C) right temporal cortex (TEMP). In each panel, sample raw MEGAPRESS “On” (difference-edited) and “Off” (1D-68ms) spectra are shown in black, along with their LCModel fits in red. Residuals above each spectrum depict the accuracy of the data fit. Cho choline, Cr creatine, GABA γ-aminobutyric acid, mI myoinositol.
A 2 × 2 × 3 cm3 right insula voxel was obliqued in the sagittal and axial planes along the axis of the insular cortex as we previously described [20]. This voxel was placed with its anterior edge at the anterior limit of the insula and the medial border was positioned to maximize insula gray matter and exclude other subcortical nuclei. This voxel includes the anterior and middle insular gyri.
A 2 × 2 × 3 cm3 right temporal cortex voxel was obliqued in the sagittal plane along the horizontal portion of the posterior superior temporal sulcus and centered on the Jensen sulcus in the sagittal and coronal planes. This voxel contains portions of posterior middle and superior temporal gyri.
Spectral acquisition
Shimming of the voxel was conducted using a machine automated routine, followed by manual shimming (JEJ). Following automated water-suppression, carrier-frequency, tip angles and coil tuning, a MEGAPRESS sequence [14]) acquired single voxel spectra at 68 ms in pairs collected in interleaved fashion, with the GABA-edited pulse applied on every second transient. Pairs (256) of “ON” and “OFF” spectra were acquired at a TR = 2 s and a spectral bandwidth of 1.2 kHz, with a scan duration = 8.5 min.
MRS data processing
All spectra were visually inspected for artifacts and fitting errors (JEJ). Spectra were excluded from the analyses for a full-width half maximum (FWHM) > 12, signal-to-noise ratio (SNR) < 6, a Cramer Rao Lower Bounds ≥ 20% for GABA and 10% for NAA. Based on these criteria, quality metabolite data were available for n = 110 (38 PTSD, 34 TENC, 38 HC) from mPFC, for n = 107 (37 PTSD, 33 TENC, 37 HC) from right insula, and for n = 106 (37 PTSD, 34 TENC, 35 HC) from temporal cortex.
Spectral data were processed using a Linux workstation with in-house reconstruction software and LCModel software [36], blind to subject information and group assignment. For quantification of GABA, difference-edited spectra were fitted in LCModel with basis sets using identical spectral sequences used to acquire in vivo spectra at 3T. Individual “ON” and “OFF” averages were frequency- and phase-corrected using the residual water resonances as a navigator. All “ON” and “OFF” spectra were averaged separately to produce single 68 ms “ON” and “OFF” spectra, which subsequently were subtracted to produce an optimized, difference-edited GABA spectrum. The processing pipeline yielded unscaled values for creatine and GABA. Because acquired GABA spectra contain contributions from co-edited macromolecules at the 3.00 ppm resonance, GABA is denoted as GABA+ as done previously (e.g. [37,38,39]). The difference-edited GABA resonance at 3.00 ppm and co-edited Glu and Gln peaks at 3.75 ppm and ~2.3 ppm were normalized to the fitted creatine (Cr) resonance (GABA+/Cr) from the 68 ms sub-spectrum [40, 41], after verifying that the groups did not differ on the ratio of Cr to the total 68 ms proton spectrum (mPFC: F(2,107) = 0.273, p = 0.762; insula: F(2,104) = 0.303, p = 0.739; temporal cortex: F(2,103) = 1.457, p = 0.238). Figure 1 shows sample raw MEGAPRESS “ON” (difference-edited) and “OFF” (1D-68ms) spectra (black) and associated fits (red). Tissue composition of each voxel was determined by segmenting T1 images into gray matter, white matter and cerebrospinal (CSF) using FSL 4.1 (FMRIB Software Library Analysis Group, FMRIB; Oxford, UK). In a separately recruited sample, test-retest assessments of insula GABA+/Cr in six healthy adults (scanned twice within 30 min) yielded a coefficient of variation of 11.76% ± 9.67 (mean ± SD), which is within the range of repeatability results obtained by others [13, 39, 42].
Statistical analyses
Analyses of variance (ANOVA) examined group differences in GABA+/Cr with a Bonferroni-adjusted p-value of .017 adjusting for comparisons at three voxels, and post-hoc Dunnett’s tests comparing PTSD to HC and TENC to HC. These were followed by linear models that covaried for potentially confounding effects of age, sex, and CSF proportion of the voxel, consistent with prior literature [20, 43]. For linear regressions with significant effects of group, we ran follow-up Dunnett’s tests of least-squares means, adjusting for the covariates. Pearson correlations examined bivariate associations, including whether GABA+/Cr was significantly correlated with sleep disruption, hyperarousal–, and DES scores. To minimize the number of analyses, symptom correlations were run only for regions where the omnibus linear model had identified a significant association of group with GABA+/Cr. Correlations were exploratory and not corrected for multiple comparisons. All statistical analyses were conducted using JMP 14.0 (SAS Institute Inc, USA).
Results
Table 1 shows demographic and clinical characteristics of the participants.
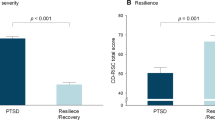
Group differences in GABA and NAA
Insula
Table 2 shows metabolite levels across groups. There was a significant group difference in insula GABA+/Cr (F(2,107) = 3.142, p = 0.047), corresponding to lower GABA+/Cr in PTSD than HC participants (Cohen’s d = −0.581, p = 0.043) and a nonsignificant difference between TENC and HC participants (d = −0.441, p = 0.090). The linear model predicting insula GABA+/Cr was statistically significant (F(5,99) = 3.593, p = 0.005), with a significant effect of group (F(2,99) = 3.240, p = 0.043), and nonsignificant effects of age, sex, and %CSF. Least-squares means Dunnett’s showed significantly lower insula GABA+/Cr in PTSD than HC (p = 0.044), not in TENC relative to HC (p = 0.080). There was no significant group difference in insula NAA/Cr (Supplement).
mPFC
ANOVA identified a significant group difference in mPFC GABA+/Cr (F(2,107) = 6.173, p = 0.003), corresponding to lower GABA+/Cr in PTSD than HC (d = −0.798, p = .003), and lower GABA+/Cr in TENC than HC (d = −0.625, p = 0.013) (Table 2). The linear model predicting mPFC GABA+/Cr was statistically significant (F(5,103) = 2.573, p = 0.031), with a significant effect of group (F(2,103) = 5.453, p = 0.006), and no significant contributions of age, sex, or %CSF. Least-squares means Dunnett’s found significantly lower mPFC GABA+/Cr in PTSD than HC (p = 0.006), and in TENC compared with HC (p = 0.024). There was no group difference in mPFC NAA/Cr (Supplement).
Temporal cortex
ANOVA identified no significant group difference in right temporal cortex GABA+/Cr (F(2,106) = 0.422, p < 0.657). The linear model predicting temporal GABA+/Cr was nonsignificant (F(5,100) = 0.894, p = 0.488), with no significant effect of group (F(2,100) = 0.640, p = 0.640) or any covariate. There was no group difference in temporal cortex NAA/Cr (Supplement).
Correlations with PTSD symptoms
Insula
Within PTSD participants (who differed significantly from HCs on insula GABA+/Cr), there was a nonsignificant negative correlation of insula GABA+/Cr with sleep disruption (r(37) = −0.277, p = 0.097; Fig. 2). Insula GABA+/Cr was not significantly correlated with hyperarousal– scores (r(37) = −0.145, p = 0.390) or DES scores (r(37) = −0.016, p = 0.927) in PTSD patients.
mPFC
Within the combined PTSD and TENC groups (who differed significantly from HCs on mPFC GABA+/Cr), there was a significant negative correlation of mPFC GABA+/Cr with DES scores (r(72) = −0.275, p = 0.019; Fig. 3). mPFC GABA+/Cr was not significantly associated with hyperarousalscores (r(70) = −0.176, p = 0.145) or sleep disruption (r(70) = −0.054, p = 0.657).
Potential comorbidity confounds
Depression
BDI scores were not significantly correlated with insula GABA+/Cr in PTSD participants (r(37) = −0.027, p = 0.872), or with mPFC GABA+/Cr in trauma-exposed participants (r(72) = 0.031, p = 0.794).
Alcohol and nicotine use
All participants reported abstaining from alcohol for at least 24 h prior to their study visit. Within the seven nicotine-dependent participants, the correlation between FTND score and mPFC GABA+/Cr was a very small effect (r(6) = −0.067, p = 0.900). Similarly, the correlation between FTND scores and insula GABA+/Cr was a small effect size (r(6) = −0.137, p = 0.796).
Discussion
In this study, we used single voxel MEGAPRESS to test the hypothesis that PTSD and trauma-exposed non-PTSD adults would show regionally-specific alterations in GABA within medial prefrontal and insular cortices, but not in the posterior temporal cortex, compared with non-traumatized healthy adults. Our secondary hypotheses examined whether differences in GABA were associated with symptoms of altered arousal. We found significantly lower mPFC GABA in both PTSD and TENC compared with HC participants, and mPFC GABA levels were significantly negatively correlated with dissociation severity within trauma-exposed participants. We also found significantly lower right insula GABA in PTSD compared with HC, but not in TENC compared with HC. As predicted, neither the PTSD nor the TENC group had significantly different GABA levels in the right posterior temporal cortex compared with HC. Finally, there were no significant group differences in NAA in any of the three voxels, indicating that the GABA differences in mPFC and insula are likely not due to differences in neuronal density.
To our knowledge, this is the first report of lower mPFC GABA in trauma-exposed adults with and without PTSD. In this study, the mPFC voxel contained mostly rostral ACC (BA 32), in contrast to the more dorsal ACC location in our prior investigation [20]. Our results differ from those of an earlier report of higher GABA in PTSD patients compared with healthy adults in a similar mPFC location [24]. This could relate to differences in how PTSD was operationalized and in the size of the voxel between the two studies. Michels et al. [24] defined PTSD using a CAPS cut-off score, not as a DSM diagnosis that requires endorsement of certain combinations of symptoms. In addition, the mPFC voxel of Michels et al. [24] extended anteriorly through the medial frontopolar cortex (BA10). Thus, differences in rostral ACC and frontal pole GABA may have contributed to the different findings across studies. Rostral ACC GABA has been shown to correlate with negative BOLD responses during emotion regulation tasks [44], and lower GABA levels in PTSD may reflect more limited capacity of prefrontal GABAergic interneurons to modulate local information-processing functions [45]. One role of mPFC GABA interneurons is to integrate afferent inputs that mediate acquisition of conditioned fear responses, such that activation of mPFC GABA neurons during fear learning may “signal” for conditioned fear stimuli during fear learning [7]. In addition, mPFC GABA interneurons regulate efferent signaling of mPFC principal neurons, ultimately modulating downstream recruitment of the larger brain network that mediates fear expression and defensive behavior [45]. Thus, our finding of lower GABA may be consistent with other neuroimaging evidence of rostral ACC dysfunction in trauma and PTSD, including prior reports of relatively decreased rostral ACC activation during emotion regulation and fear inhibition tasks [46,47,48].
A finding of lower GABA in the right insula in PTSD compared with HC participants replicates a previous finding from our laboratory, which was conducted in a different sample and using a 4 Tesla scanner [20]. We also extend those findings by showing that this GABA deficit was smaller in magnitude and not statistically significant in TENC compared with HC subjects. Because PTSD and TENC participants did not differ on lifetime trauma exposure, lower GABA in the insular cortex may be an illness marker of PTSD, rather than a marker of trauma exposure or subclinical symptom presentation. The anterior insula is involved in anticipating aversive events and monitoring emotional responses [49, 50], and it exhibits lateralized functioning whereby the right insula appears particularly important for sympathetic arousal [51]. In functional imaging studies of PTSD, anterior insula hyperactivity is consistently observed during processing of negatively-valenced stimuli including trauma reminders [52, 53]. It is possible that lower insula GABA in people with clinically-significant PTSD is related to functional over-reactivity during aversive processing.
Our findings add to evidence relating dissociation and arousal to mPFC neurobiology. We found that higher trait dissociation, reflecting a tendency towards emotional detachment and hypoarousal responses to stress, was associated with lower GABA levels in the mPFC among the trauma-exposed participants. Dissociation involves a blunting of internal physiological sensations and emotions, along with cognitive detachment from one’s immediate external surroundings. The neurobiology of dissociation involves greater mPFC top-down modulation of limbic regions such as the amygdala and insula, leading to suppression of their activity and autonomic blunting [54,55,56]. Regarding potential correlates of lower insula GABA in PTSD, there were no significant associations with dissociation, hyperarousal, or sleep disruption symptoms. We propose that the latter could be further studied using more sensitive indexes of sleep quality. Indeed, there is a growing literature supporting a relationship between GABA and sleep, including studies showing that patients with primary insomnia, compared with healthy sleepers, have significantly lower levels of cortical GABA [57,58,59]. The insula contributes to sleep via its connections with cortical and brainstem regions that control sleep-wake cycling [60, 61]. Altogether, this motivates larger investigations of insula GABA and sleep disruption in PTSD.
There are methodological strengths and limitations to consider when interpreting our findings. Because this was a cross-sectional study, we cannot assess whether lower GABA was a precursor versus consequence of trauma and PTSD; however, our findings of larger effect sizes in PTSD compared with TENC, along with symptom correlations, suggest that GABA deficits scale with aspects of illness severity. Moreover, these neurochemical differences cannot be attributed to psychotropic medication effects, since all but one participant was unmedicated. The neurochemical changes also showed some specificity to GABA, as there were no group differences in NAA in any voxel. Importantly, our study design excluded the possibility that GABA findings were related to excessive or recent use of alcohol. However, given the anxiolytic and GABAergic effects of alcohol, one avenue for future research will be to examine whether subclinical alcohol contributes to GABA deficits in some PTSD patients. Because MRS measurement captures both the pre- and post-synaptic pools of GABA, we cannot conclude that lower GABA reflects less neurotransmission or inhibition. Finally, our study did not include a dedicated assessment of sleep; rather, power to detect individual differences in sleep was limited by use of a two-item score from a general PTSD symptom measure.
In summary, our findings suggest that lower GABA differs in its presence and clinical significance across cortical regions in PTSD. Lower mPFC GABA was seen in trauma-exposed participants irrespective of PTSD diagnosis, and it may be a marker of trait-related processes such as a tendency towards dissociation. In contrast, lower right insula GABA may be an illness marker of PTSD, reflecting severity of disease processes.
References
Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry. 2004;161:195–216.
Asede D, Bosch D, Lüthi A, Ferraguti F, Ehrlich I. Sensory inputs to intercalated cells provide fear-learning modulated inhibition to the basolateral amygdala. Neuron. 2015;86:541–54.
Millan MJ. The neurobiology and control of anxious states. Prog Neurobiol. 2003;70:83–244.
Steckler T, Risbrough V. Pharmacological treatment of PTSD - established and new approaches. Neuropharmacology. 2012;62:617–27.
Adamec R, Strasser K, Blundell J, Burton P, McKay DW. Protein synthesis and the mechanisms of lasting change in anxiety induced by severe stress. Behav Brain Res. 2006;167:270–86.
Kasugai Y, Vogel E, Hörtnagl H, Schönherr S, Paradiso E, Hauschild M, et al. Structural and functional remodeling of amygdala GABAergic synapses in associative fear learning. Neuron. 2019;104:781–794.e4.
Cummings KA, Clem RL. Prefrontal somatostatin interneurons encode fear memory. Nat Neurosci. 2019;23:61–74.
Hamner MB, Brodrick PS, Labbate LA. Gabapentin in PTSD: a retrospective, clinical series of adjunctive therapy. Ann Clin Psychiatry. 2001;13:141–6.
Connor KM, Davidson JRT, Weisler RH, Zhang W, Abraham K. Tiagabine for posttraumatic stress disorder: effects of open-label and double-blind discontinuation treatment. Psychopharmacology. 2006;184:21–5.
Drake RG, Davis LL, Cates ME, Jewell ME, Ambrose SM, Lowe JS. Baclofen treatment for chronic posttraumatic stress disorder. Ann Pharmacother. 2003;37:1177–81.
Manteghi AA, Hebrani P, Mortezania M, Haghighi MB, Javanbakht A. Baclofen add-on to citalopram in treatment of posttraumatic stress disorder. J Clin Psychopharmacol. 2014;34:240–3.
Pollack MH, Hoge EA, Worthington JJ, Moshier SJ, Wechsler RS, Brandes M, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72:892–7.
Duda JM, Moser AD, Zuo CS, Du F, Chen X, Perlo S, et al. Repeatability and reliability of GABA measurements with magnetic resonance spectroscopy in healthy young adults. Magn Reson Med. 2021;85:2359–69.
Mescher M, Merkle H, Kirsch J, Garwood M, Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed. 1998;11:266–72.
Gabbay V, Mao X, Klein RG, Ely BA, Babb JS, Panzer AM, et al. Anterior cingulate cortex γ-aminobutyric acid in depressed adolescents: relationship to anhedonia. Arch Gen Psychiatry. 2012;69:139–49.
Hasler G, Neumeister A, van der Veen JW, Tumonis T, Bain EE, Shen J, et al. Normal prefrontal gamma-aminobutyric acid levels in remitted depressed subjects determined by proton magnetic resonance spectroscopy. Biol Psychiatry. 2005;58:969–73.
Hasler G, van der Veen JW, Tumonis T. Glutamate/glutamine and GABA levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64:193–200.
Öngür D, Prescot AP, McCarthy J, Cohen BM, Renshaw PF. Elevated gamma-aminobutyric acid levels in chronic schizophrenia. Biol Psychiatry. 2010;68:667–70.
Streeter CC, Gerbarg PL, Brown RP, Scott TM, Nielsen GH, Owen L, et al. Thalamic gamma aminobutyric acid level changes in major depressive disorder after a 12-week Iyengar yoga and coherent breathing intervention. J Alter Complement Med. 2020;26:190–7.
Rosso IM, Weiner MR, Crowley DJ, Silveri MM, Rauch SL, Jensen JE. Insula and anterior cingulate GABA levels in posttraumatic stress disorder: preliminary findings using magnetic resonance spectroscopy. Depress Anxiety. 2014;31:115–23.
Sheth C, Prescot AP, Legarreta M, Renshaw PF, McGlade E, Yurgelun-Todd D. Reduced gamma-amino butyric acid (GABA) and glutamine in the anterior cingulate cortex (ACC) of veterans exposed to trauma. J Affect Disord. 2019;248:166–74.
Meyerhoff DJ, Mon A, Metzler T, Neylan TC. Cortical gamma-aminobutyric acid and glutamate in posttraumatic stress disorder and their relationships to self-reported sleep quality. Sleep. 2014;37:893–900.
Pennington DL, Abé C, Batki SL, Meyerhoff DJ. A preliminary examination of cortical neurotransmitter levels associated with heavy drinking in posttraumatic stress disorder. Psychiatry Res. 2014;224:281–7.
Michels L, Schulte-Vels T, Schick M, O’Gorman RL, Zeffiro T, Hasler G, et al. Prefrontal GABA and glutathione imbalance in posttraumatic stress disorder: preliminary findings. Psychiatry Res. 2014;224:288–95.
Cosgrove KP, Esterlis I, Mason GF, Bois F, O’Malley SS, Krystal JH. Neuroimaging insights into the role of cortical GABA systems and the influence of nicotine on the recovery from alcohol dependence. Neuropharmacology. 2011;60:1318–25.
Krystal JH, Staley J, Mason G, Petrakis IL, Kaufman J, Adron Harris R, et al. γ-Aminobutyric acid type A receptors and alcoholism: intoxication, dependence, vulnerability, and treatment. Arch Gen Psychiatry. 2006;63:957–68.
Mason GF, Petrakis IL, de Graaf RA, Gueorguieva R, Guidone E, Coric V, et al. Cortical gamma-aminobutyric acid levels and the recovery from ethanol dependence: preliminary evidence of modification by cigarette smoking. Biol Psychiatry. 2006;59:85–93.
Schür RR, Draisma LWR, Wijnen JP, Boks MP, Koevoets MGJC, Joëls M, et al. Brain GABA levels across psychiatric disorders: a systematic literature review and meta-analysis of (1) H-MRS studies. Hum Brain Mapp. 2016;37:3337–52.
Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–41.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90.
Beck AT, Steer RA. Manual for the Beck Depression Inventory, 1993 edition. The Psychological Corporation, San Antonio, TX. 1993.
Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation: Prog Dissociative Disord. 1993;6:16–27.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom K-O. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Addiction. 1991;86:1119–27.
Kegeles LS, Mao X, Stanford AD, Girgis R, Ojeil N, Xu X, et al. Elevated prefrontal cortex γ-aminobutyric acid and glutamate-glutamine levels in schizophrenia measured in vivo with proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2012;69:449–59.
Hasler G, van der Veen JW, Geraci M, Shen J, Pine D, Drevets WC. Prefrontal cortical gamma-aminobutyric acid levels in panic disorder determined by proton magnetic resonance spectroscopy. Biol Psychiatry. 2009;65:273–5.
Provencher SW. Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med. 1993;30:672–9.
Costigan AG, Umla-Runge K, Evans CJ, Hodgetts CJ, Lawrence AD, Graham KS. Neurochemical correlates of scene processing in the precuneus/posterior cingulate cortex: a multimodal fMRI and 1 H-MRS study. Hum Brain Mapp. 2019;40:2884–98.
Gaetz W, Bloy L, Wang DJ, Port RG, Blaskey L, Levy SE, et al. GABA estimation in the brains of children on the autism spectrum: measurement precision and regional cortical variation. Neuroimage. 2014;86:1–9.
Mikkelsen M, Singh KD, Sumner P, Evans CJ. Comparison of the repeatability of GABA-edited magnetic resonance spectroscopy with and without macromolecule suppression. Magn Reson Med. 2016;75:946–53.
Mullins PG, McGonigle DJ, O’Gorman RL, Puts NAJ, Vidyasagar R, Evans CJ, Cardiff Symposium on MRS of GABA, Edden RAE. Current practice in the use of MEGA-PRESS spectroscopy for the detection of GABA. Neuroimage. 2014;86:43–52.
Weis J, Persson J, Frick A, Åhs F, Versluis M, Alamidi D. GABA quantification in human anterior cingulate cortex. PLoS One. 2021;16:e0240641.
Baeshen A, Wyss PO, Henning A, O’Gorman RL, Piccirelli M, Kollias S, et al. Test-retest reliability of the brain metabolites GABA and Glx with JPRESS, PRESS, and MEGA-PRESS MRS sequences in vivo at 3T. J Magn Reson Imaging. 2020;51:1181–91.
Harasym D, Nelson AJ, Noseworthy M. Sources of variability and improvements in the measure of GABA using MEGA-PRESS at 3T. CRB. https://doi.org/10.1615/CritRevBiomedEng.2020030321. 2019.
Northoff G, Walter M, Schulte RF, Beck J, Dydak U, Henning A, et al. GABA concentrations in the human anterior cingulate cortex predict negative BOLD responses in fMRI. Nat Neurosci. 2007;10:1515–7.
Prévot T, Sibille E. Altered GABA-mediated information processing and cognitive dysfunctions in depression and other brain disorders. Mol Psychiatry. 2021;26:151–67.
New AS, Fan J, Murrough JW, Liu X, Liebman RE, Guise KG, et al. A functional magnetic resonance imaging study of deliberate emotion regulation in resilience and posttraumatic stress disorder. Biol Psychiatry. 2009;66:656–64.
Stevens JS, Ely TD, Sawamura T, Guzman D, Bradley B, Ressler KJ, et al. Childhood maltreatment predicts reduced inhibition-related activity in the rostral anterior cingulate in PTSD, but not trauma-exposed controls. Depress Anxiety. 2016;33:614–22.
Rougemont-Bücking A, Linnman C, Zeffiro TA, Zeidan MA, Lebron-Milad K, Rodriguez-Romaguera J, et al. Altered processing of contextual information during fear extinction in PTSD: an fMRI study. CNS Neurosci Therapeutics. 2011;17:227–36.
Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3:655–66.
Craig AD. Significance of the insula for the evolution of human awareness of feelings from the body. Ann N.Y. Acad Sci. 2011;1225:72–82.
Holtmann O, Franz M, Moenig C, Tenberge J-G, Schloßmacher I, Ivanova I, et al. Lateralized deficits in arousal processing after insula lesions: behavioral and autonomic evidence. bioRxiv 2021.03.24.436828.
Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164:1476–88.
Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60:383–7.
Nicholson AA, Friston KJ, Zeidman P, Harricharan S, McKinnon MC, Densmore M, et al. Dynamic causal modeling in PTSD and its dissociative subtype: bottom-up versus top-down processing within fear and emotion regulation circuitry. Hum Brain Mapp. 2017;38:5551–61.
Hopper JW, Frewen PA, van der Kolk BA, Lanius RA. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. J Trauma Stress. 2007;20:713–25.
Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. 2010;167:640–7.
Plante DT, Jensen JE, Schoerning L, Winkelman JW. Reduced γ-aminobutyric acid in occipital and anterior cingulate cortices in primary insomnia: a link to major depressive disorder? Neuropsychopharmacology. 2012;37:1548–57.
Winkelman JW, Buxton OM, Jensen JE, Benson KL, O’Connor SP, Wang W, et al. Reduced brain GABA in primary insomnia: preliminary data from 4T proton magnetic resonance spectroscopy (1H-MRS). Sleep. 2008;31:1499–506.
Morgan PT, Pace-Schott EF, Mason GF, Forselius E, Fasula M, Valentine GW, et al. Cortical GABA levels in primary insomnia. Sleep. 2012;35:807–14.
Chen MC, Chang C, Glover GH, Gotlib IH. Increased insula coactivation with salience networks in insomnia. Biol Psychol. 2014;97:1–8.
Chen MC, Chiang W-Y, Yugay T, Patxot M, Özçivit İB, Hu K, et al. Anterior insula regulates multiscale temporal organization of sleep and wake activity. J Biol Rhythms. 2016;31:182–93.
Acknowledgements
We thank all participants of this research study, and the technologists and staff of the McLean Imaging Center. A preliminary report of these data was presented as a poster presentation at the 2018 annual meeting of the American College for Neuropsychopharmacology (ACNP). No portion of these data has been previously published.
Funding
This research was supported by the National Institute of Mental Health (R01MH096987; IMR). IMR was also partially supported by R01MH120400 and P50MH115874. EAO was partially supported by K23MH112873. The authors have no conflicts of interest in relation to this work.
Author information
Authors and Affiliations
Contributions
IMR conceived the study and obtained funding. IMR, MMS, JEJ designed the study and protocol. IMR, MMS, EAO, JEJ contributed to data collection and processing, and BR assisted with statistical analysis and review. IMR wrote the initial draft of the manuscript. All authors provided critical input to the manuscript, contributed to revised drafts, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rosso, I.M., Silveri, M.M., Olson, E.A. et al. Regional specificity and clinical correlates of cortical GABA alterations in posttraumatic stress disorder. Neuropsychopharmacol. 47, 1055–1062 (2022). https://doi.org/10.1038/s41386-021-01197-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01197-x