Novel Antibody Combinations Expand Treatment Options in Multiple Myeloma
Single-agent belantamab demonstrated anti-myeloma activity and a manageable safety profile in the DREAMM-2 phase 2 study.
Saad Z. Usmani, MD

Investigators continue to look to novel antibody combinations that include antibody-drug conjugates (ADCs), as well as bispecific and trispecific antibodies in preclinical and clinical trials, for patients with multiple myeloma (MM).
“Multiple myeloma is a prime example of a heterogeneous disease that must be treated with multiple mechanisms of action,” said Saad Z. Usmani, MD. Usmani who presented virtually during the multiple myeloma session at the Society of Hematologic Oncology (SOHO) 2021 Annual Meeting.1 His presentation, “Novel BCMA Targeted ADCs, Bispecific and Trispecific Antibodies,” emphasized that these agents will be part of the armamentarium of the future but that investigators should be aware of their efficacy and safety profiles. That is especially true for belantamab mafodotin-blmf (Blenrep), a first-in-class ADC that targets the B-cell maturation antigen (BCMA).
Single-agent belantamab demonstrated anti-myeloma activity and a manageable safety profile in the DREAMM-2 phase 2 study (NCT03525678).2 In the study, 293 patients were screened, and 196 patients were included in the intention-to-treat population. Patients were randomized to receive 2.5 mg/kg or 3.4 mg/kg belantamab via intravenous infusion every 3 weeks on day 1 of each cycle until disease progression or unacceptable toxicity. The intention-to-treat population comprised all randomized patients, regardless of treatment administration. At data cutoff, 30 of 97 (31%) patients in the 2.5-mg arm had an overall response (97.5% CI, 20.8%-42.6%) and 34 of 99 (34%) patients in the 3.4-mg arm had an overall response (97.5% CI, 23.9%-46.0%).
Regarding safety, the most common grade 3-4 adverse events (AEs) observed in the 2.5-mg arm (n = 95) was keratopathy (27%), thrombocytopenia (20%), and anemia (20%). In the 3.4-mg arm (n = 99), most common AEs were keratopathy (21%), thrombocytopenia (33%), and anemia (25%).
“I think there’s a natural learning curve associated with every new product and technology in cancer medicine,” Usmani said in an interview with Targeted Therapies in Oncology™ before the conference. He recommended that community oncologists who treat patients with belantamab should partner with an ophthalmologist because keratopathy is considered an AE of special interest, as observed in clinical trials. He noted that it’s common to refer patients with cancer to other specialists in subspecialties to help meet patient needs.
Turning to bispecific and trispecific antibodies, Usmani noted that patients who are penta-refractory have notably poor outcomes, but that the horizon looks bright.
Bispecific antibodies have shown high response in early clinical trials. This type of antibody is engineered so that one end binds to the multiple myeloma cells and the other binds to the T cell. By targeting BCMA, CD38, GPRC5D, and FDRH5, these agents mobilize cytotoxic T cells to attack tumor cells through CD3. Additional research involving bispecific antibodies use natural killer (NK) cells through CD16 to carry out attacks on tumor cells, but this is in preclinical development.2
In order for this mode of treatment to be effective, the patient’s T cells have to be healthy and viable, and the bone marrow microenvironment has to be conducive, Usmani said. AEs are similar to chimeric antibody receptor (CAR) T-cell therapies, which also uses T cells. These AEs include cytokine release syndrome and neurotoxicities, but “the proportion of patients who experience these AEs is lower and the grading is lower compared with CAR T-cell therapy,” Usmani said.
Another caveat when considering using CAR T-cell therapy in patients is the length of time it takes to prepare the treatment. “Right now, the challenge with CAR T-cell therapy is the time it takes to collect the T cells and the wait for the product to come back,” Usmani said. “Many patients may have progressive disease requiring additional chemotherapy for disease control, or they may no longer be eligible for CAR T-cell therapy because of the disease burden and renal failure.”
Usmani highlighted findings from a phase 1 first-in-human study (NCT03145181) evaluating teclistamab, a bispecific antibody, in patients with relapsed/refractory multiple myeloma.3 The primary objectives were to identify the recommended phase 2 dose in part 1 of the study and determine the agent’s safety and tolerability at the recommended phase 2 dose, which was part 2 of the study.
There were 219 patients screened for inclusion and 157 patients were enrolled and received at least 1 dose of the agent (intravenous administration, n = 84; subcutaneous administration, n = 73). A total of 40 patients were given the recommended phase 2 dose.
Investigators reported no dose-limiting toxicities at the recommended phase 2 dose in the first part of the study. In the 40 patients treated at the recommended phase 2 dose, the most common treatment-emergent AEs were cytokine release syndrome in 28 (70%; all grade 1 or 2 events) and neutropenia in 26 (65%) patients (grade 3 or 4 in 16 [40%]).
Responses were encouraging, with the overall response rate in patients treated at the recommended phase 2 dose at 65% (95% CI, 48%-79%). Investigators reported a very good partial response or better for 58% of patients. Median duration of response was not reached for the recommended phase 2 dose and 85% of responders were alive and continuing treatment after 7.1 months’ median follow-up (interquartile range, 5.1-9.1).
Another area of preclinical development involves trispecific antibodies. These antibodies may provide a T-cell costimulatory signal such as CD28, or alternatively, dual MM antigens to increase specificity of NK or T-cell targeting.4
“Trispecific antibodies can stimulate T or NK cells, but the other 2 [binding domains] will have 2 separate recognition patterns for 2 different kinds of surface markers,” Usmani said. “These antibodies haven’t reached the clinical trial setting yet, but the concept is intriguing. So their development is similar to the development of bispecific antibodies.”
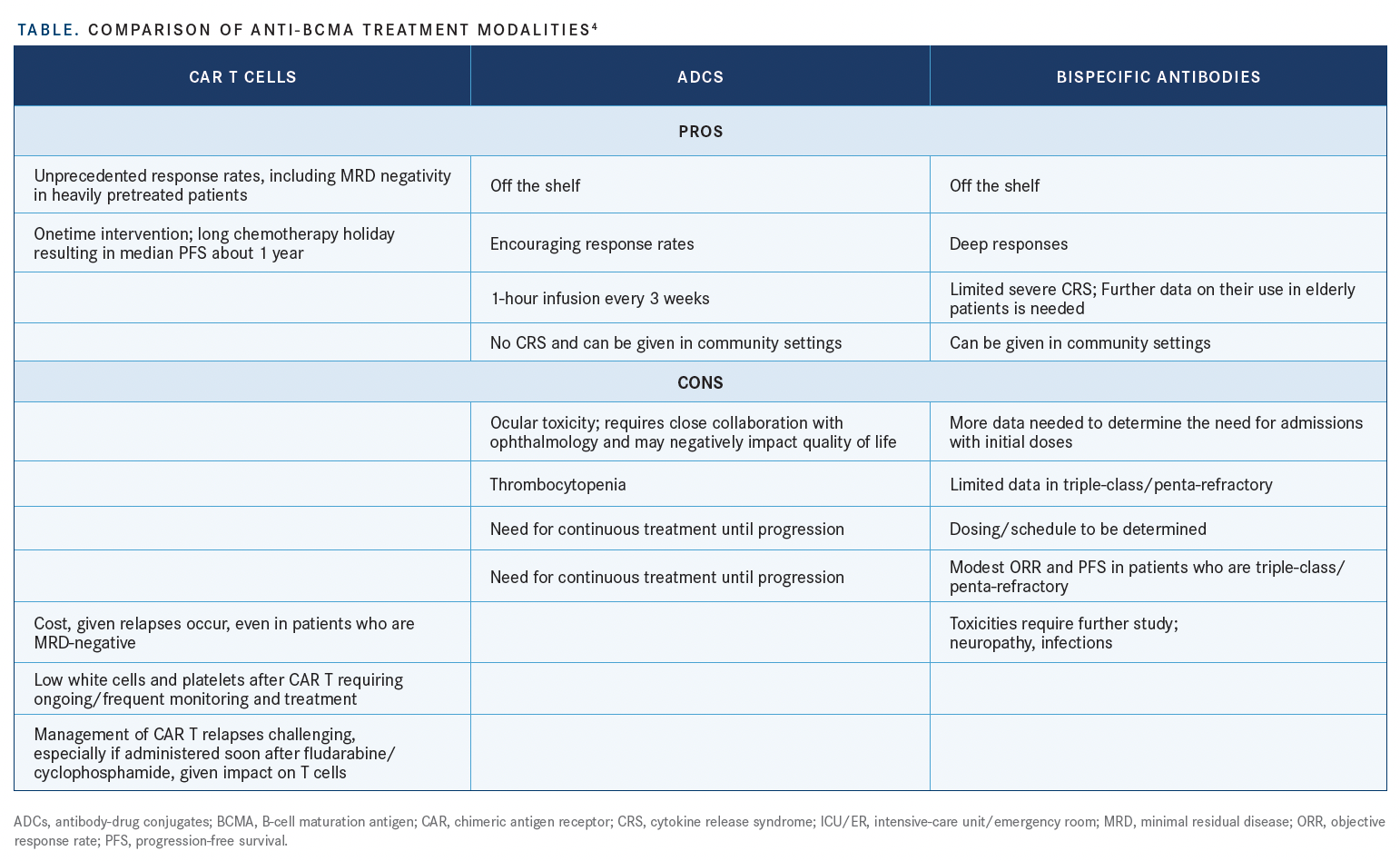
A comparison of anti-BCMA modalities is shown in the TABLE.4
Usmani concluded by emphasizing the importance of using combination therapies because it “has made the most impact in terms of improving survival outcomes, especially in the relapsed/refractory setting.” With the emergence of these novel antibodies, a similar approach will be required. “That will be a key message in my presentation. These immunotherapies are promising, but just targeting BCMA is not going to [be curative.] This approach could be part of the strategy,” he said
References:
1. Usmani S. Novel BCMA targeted ADCs, bispecific and trispecific antibodies. Presented at: 2021 Society of Hematologic Oncology Annual Meeting. September 8-11, 2021; virtual.
2. Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21(2):207- 221. doi:10.1016/S1470-2045(19)30788-0
3. Usmani SZ, Garfall AL, van de Donk NWCJ, et al. Teclistamab, a B-cell maturation antigen × CD3 bispecific antibody, in patients with relapsed or refractory multiple myeloma (MajesTEC-1): a multicentre, open-label, single-arm, phase 1 study. Lancet. Published online August 10, 2021. doi:10.1016/S0140-6736(21)01338-6
4. Lancman G, Richter J, Chari A. Bispecifics, trispecifics, and other novel immune treatments in myeloma. Hematology Am Soc Hematol Educ Program. 2020;2020(1):264-271. doi:10.1182/hematology.2020000110

Powell Reviews Updated IO/TKI Data and AE Management in Endometrial Cancer
April 18th 2024During a Case-Based Roundtable® event, Matthew A. Powell, MD, discussed the case of a patient with advanced endometrial cancer treated with lenvatinib plus pembrolizumab who experienced grade 2 treatment-related hypertension.
Read More
Savona Discusses First-Line JAK Inhibition for Patients With Myelofibrosis at Risk of Anemia
April 17th 2024During a Case-Based Roundtable® event, Michael Savona, MD, and participants discussed the case of a patient with myelofibrosis and moderate anemia receiving JAK inhibitor therapy.
Read More