Abstract
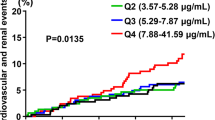
We aimed to evaluate the relationship of the albumin-to-creatinine ratio (ACR) with the risk of first stroke and examine possible effect modifiers in hypertensive patients. A total of 11,632 hypertensive participants with urinary ACR measurements and without a history of stroke from the China Stroke Primary Prevention Trial (CSPPT) were included in this analysis. The primary outcome was first stroke. Over a median follow-up of 4.4 years, 728 first strokes were identified, of which 633 were ischemic, 89 were hemorrhagic, and 6 were uncertain types. Overall, there was a significant positive association between natural log-transformed ACR and the risk of first stroke (HR, 1.11; 95% CI: 1.03–1.20) and first ischemic stroke (HR, 1.12; 95% CI: 1.03–1.22). Consistently, participants with ACR ≥ 10 mg/g had a significantly higher risk of first stroke (HR, 1.26; 95% CI: 1.06–1.50) and first ischemic stroke (HR, 1.33; 95% CI: 1.10–1.59) than those with ACR < 10 mg/g. Moreover, the association of ACR with first stroke was significantly stronger in participants with higher total homocysteine (tHcy) levels (<10 versus ≥ 10 μmol/L; P for interaction = 0.044). However, there was no significant association between ACR and first hemorrhagic stroke (per natural log [ACR] increment: HR, 1.02; 95% CI: 0.82–1.27). In summary, hypertensive patients with ACR ≥ 10 mg/g had a significantly increased risk of first stroke or first ischemic stroke. This positive association was more pronounced among participants with higher tHcy levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data described in the manuscript, code book, and analytic code will be made available from the corresponding authors on request after the request is submitted and formally reviewed and approved by the Ethics Committee of the Institute of Biomedicine, Anhui Medical University, Hefei, China.
References
GBD 2016 Lifetime Risk of Stroke Collaborators. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl J Med. 2018;379:2429–37.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–58.
Li Y, Liang M, Jiang C, Wang G, Li J, Zhang Y, et al. Impact of achieved blood pressure on renal function decline and first stroke in hypertensive patients with chronic kidney disease. Nephrol Dial Transpl. 2018;33:409–17.
Li Y, Zhou H, Liu M, Liang M, Wang G, Wang B, et al. Association of visit-to-visit variability in blood pressure and first stroke risk in hypertensive patients with chronic kidney disease. J Hypertens. 2020;38:610–7.
Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313:837–46.
Ärnlöv J, Evans JC, Meigs JB, Wang TJ, Fox CS, Levy D, et al. Low-Grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–75.
Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet. 2010;375:2073–81.
Mahmoodi BK, Yatsuya H, Matsushita K, Sang Y, Gottesman RF, Astor BC, et al. Association of kidney disease measures with ischemic versus hemorrhagic strokes. Stroke. 2014;45:1925–31.
Yuyun MF, Khaw KT, Luben R, Welch A, Bingham S, Day NE, et al. Microalbuminuria and stroke in a British population: The European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) population study. J Intern Med. 2004;255:247–56.
Solbu MD, Kronborg J, Jenssen TG, Njølstad I, Løchen M, Mathiesen EB, et al. Albuminuria, metabolic syndrome and the risk of mortality and cardiovascular events. Atherosclerosis. 2009;204:503–8.
Aguilar MI, O’Meara ES, Seliger S, Longstreth WJ, Hart RG, Pergola PE, et al. Albuminuria and the risk of incident stroke and stroke types in older adults. Neurology. 2010;75:1343–50.
Bouchi R, Babazono T, Yoshida N, Nyumura I, Toya K, Hayashi T, et al. Association of albuminuria and reduced estimated glomerular filtration rate with incident stroke and coronary artery disease in patients with type 2 diabetes. Hypertens Res. 2010;33:1298–304.
Hitman GA, Colhoun H, Newman C, Szarek M, Betteridge DJ, Durrington PN, et al. Stroke prediction and stroke prevention with atorvastatin in the Collaborative Atorvastatin Diabetes Study (CARDS). Diabet Med. 2007;24:1313–21.
Yang X, Ko GT, So WY, Ma RC, Kong AP, Lam CW, et al. Additive interaction of hyperglycemia and albuminuria on risk of ischemic stroke in type 2 diabetes: Hong Kong Diabetes Registry. Diabetes Care. 2008;31:2294–2300.
Wachtell K, Ibsen H, Olsen MH, Borch-Johnsen K, Lindholm LH, Mogensen CE, et al. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: The LIFE study. Ann Intern Med. 2003;139:901–6.
Zhang C, Wang X, He M, Qin X, Tang G, Xu X, et al. Proteinuria is an independent risk factor for first incident stroke in adults under treatment for hypertension in China. J Am Heart Assoc. 2015;4:e002639.
Kistorp C, Raymond I, Pedersen F, Gustafsson F, Faber J, Hildebrandt P. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA. 2005;293:1609–16.
Gutiérrez OM, Judd SE, Muntner P, Rizk DV, McClellan WM, Safford MM, et al. Racial differences in albuminuria, kidney function, and risk of stroke. Neurology. 2012;79:1686–92.
Scirica BM, Mosenzon O, Bhatt DL, Udell JA, Steg PG, McGuire DK, et al. Cardiovascular outcomes according to urinary albumin and kidney disease in patients with type 2 diabetes at high cardiovascular risk: observations from the SAVOR-TIMI 53 trial. JAMA Cardiol. 2018;3:155–63.
Leitão L, Soares-dos-Reis R, Neves JS, Baptista RB, Bigotte Vieira M, Mc, et al. Intensive blood pressure treatment reduced stroke risk in patients with albuminuria in the SPRINT trial. Stroke. 2019;50:3639–42.
Masson P, Webster AC, Hong M, Turner R, Lindley RI, Craig JC. Chronic kidney disease and the risk of stroke: A systematic review and meta-analysis. Nephrol Dial Transpl. 2015;30:1162–9.
Huo Y, Li J, Qin X, Huang Y, Wang X, Gottesman RF, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China. JAMA. 2015;313:1325–35.
Qin X, Li J, Zhang Y, Chen D, Wang B, He M, et al. Effect of folic acid supplementation on risk of new-onset diabetes in adults with hypertension in China: Findings from the China Stroke Primary Prevention Trial (CSPPT). J Diabetes. 2016;8:286–94.
Kong X, Huang X, Zhao M, Xu B, Xu R, Song Y, et al. Platelet Count Affects Efficacy of Folic Acid in Preventing First Stroke. J Am Coll Cardiol. 2018;71:2136–46.
Qin X, Li Y, He M, Tang G, Yin D, Liang M, et al. Folic acid therapy reduces serum uric acid in hypertensive patients: a substudy of the China Stroke Primary Prevention Trial (CSPPT). Am J Clin Nutr. 2017;105:882–9.
Sun P, Liu L, Liu C, Zhang Y, Yang Y, Qin X, et al. Carotid Intima-Media thickness and the risk of first stroke in patients with hypertension. Stroke. 2020;51:379–86.
Ganyu Health Bureau. Notice on the work of monitoring the cardiovascular and cerebrovascular diseases. Ganyu government official website. http://xxgk.ganyu.gov.cn/XXGK/ArticleDetail/55633. Name of issuing department or agency: Health Bureau. 2012-03-14. Publication number: (2012)22.
Lianyungang health planning committee. Notice on accelerating the construction of the comprehensive prevention and control demonstration zone for chronic diseases in the city. Lianyungang Municipal People’s Government. http://xxgk.lyg.gov.cn/lygbcms/front/s20/c537/20180516/i58378.html. Lianyungang health planning committee. 2018-05-09. Publication number: 14252735/2018-00110.
Zhao M, Wu G, Li Y, Wang X, Hou FF, Xu X, et al. Meta-analysis of folic acid efficacy trials in stroke prevention: Insight into effect modifiers. Neurology. 2017;88:1830–8.
Spence JD, Barnett PA, Hegele RA, Marian AJ, Freeman D, Malinow MR. Plasma Homocyst(e)ine, but not MTHFR genotype, is associated with variation in carotid plaque area. Stroke. 1999;30:969–73.
Qin X, Huo Y. H-Type hypertension, stroke and diabetes in China: Opportunities for primary prevention. J Diabetes. 2016;8:38–40.
Huang X, Li Y, Li P, Li J, Bao H, Zhang Y, et al. Association between percent decline in serum total homocysteine and risk of first stroke. Neurology. 2017;89:2101–7.
Spence JD, Yi Q, Hankey GJ. B vitamins in stroke prevention: time to reconsider. Lancet Neurol. 2017;16:750–60.
Stehouwer CD, Smulders YM. Microalbuminuria and risk for cardiovascular disease: Analysis of potential mechanisms. J Am Soc Nephrol. 2006;17:2106–11.
Schutte R, Schmieder RE, Huisman HW, Smith W, van Rooyen JM, Fourie CM, et al. Urinary albumin excretion from spot urine samples predict all-cause and stroke mortality in Africans. Am J Hypertens. 2014;27:811–8.
Wada M, Nagasawa H, Kurita K, Koyama S, Arawaka S, Kawanami T, et al. Microalbuminuria is a risk factor for cerebral small vessel disease in community-based elderly subjects. J Neurol Sci. 2007;255:27–34.
Bansal N, Zelnick LR, Alonso A, Benjamin EJ, de Boer IH, Deo R, et al. eGFR and Albuminuria in Relation to Risk of Incident Atrial Fibrillation: A Meta-Analysis of the Jackson Heart Study, the Multi-Ethnic Study of Atherosclerosis, and the Cardiovascular Health Study. Clin J Am Soc Nephrol. 2017;12:1386–98.
Yang X, Ko GT, So WY, Ma RC, Kong AP, Lam CW, et al. Additive interaction of hyperglycemia and albuminuria on risk of ischemic stroke in type 2 diabetes: Hong Kong Diabetes Registry. Diabetes Care. 2018;31:2294–2300.
Funding
The study was supported by the National Key Research and Development Program [2016YFE0205400, 2018ZX09739010, 2018ZX09301034003]; the Department of Science and Technology of Guangdong Province [2020B121202010]; the Science and Technology Planning Project of Guangzhou, China [201707020010]; the Science, Technology and Innovation Committee of Shenzhen [GJHS20170314114526143, JSGG20180703155802047]; the Economic, Trade and Information Commission of Shenzhen Municipality [20170505161556110, 20170505160926390, 201705051617070]; the Key Clinical Research Program of Southern Medical University [LC2019ZD005]; the High-level Matching Funds of Nanfang Hospital [2014070]; the Major New Drug Creation Technology Major Project [2020zx09201017]; the President Foundation of Nanfang Hospital, Southern Medical University [2017C007]; the President Foundation of Nanfang Hospital, Southern Medical University [2018Z009]; Outstanding Youth Development Scheme of Nanfang Hospital, Southern Medical University [2019J004]; and the National Natural Science Foundation of China [82000691, 81973133, 81730019].
Author information
Authors and Affiliations
Contributions
Min Liang, XX, and XQ designed the research; Min Liang, PH, HL, Yuanyuan Zhang, YY, Mengyi Liu, CZ, ZZ, ZL, JT, and MY contributed to data collection; PH and Yuanyuan Zhang analyzed data; Min Liang, PH, and XQ wrote the paper; All authors reviewed/edited the manuscript for important intellectual content; All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
He, P., Yang, Y., Tian, J. et al. Urinary albumin-to-creatinine ratio and the risk of first stroke in Chinese hypertensive patients treated with angiotensin-converting enzyme inhibitors. Hypertens Res 45, 116–124 (2022). https://doi.org/10.1038/s41440-021-00780-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00780-5
Keywords
This article is cited by
-
Risk factors for stroke among anthropometric indices and lipid profiles in the Korean population: a large-scale cross-sectional study
Scientific Reports (2023)
-
Elevated albumin-to-creatinine ratio as a risk factor for stroke and homocysteine as an effect modifier in hypertensive Asian individuals
Hypertension Research (2022)