Multiple Trials Examined for RET-Targeted Therapies in MTC
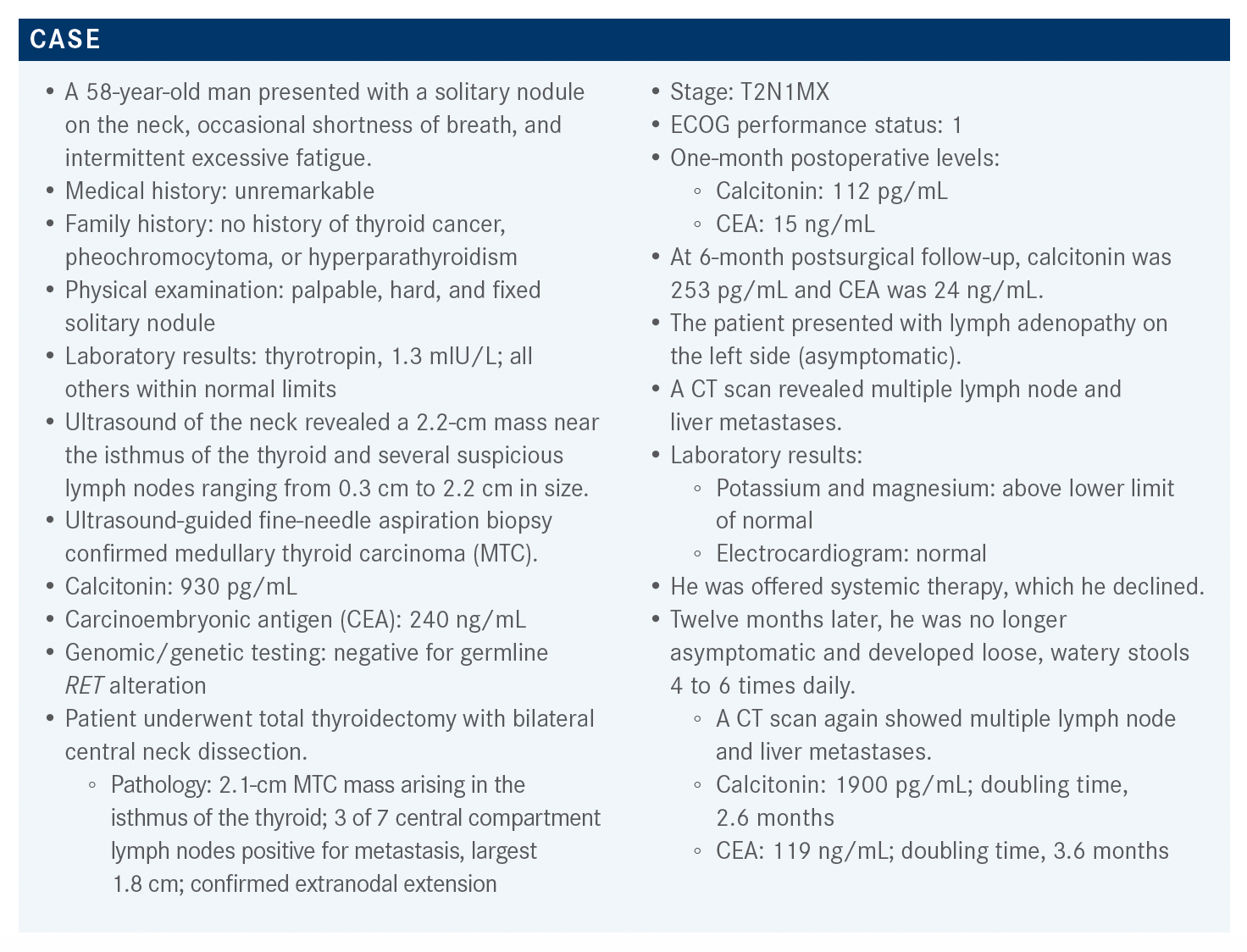
A 58-year-old man presented with a solitary nodule on the neck, occasional shortness of breath, and intermittent excessive fatigue. Twelve months after being treated with systemic therapy, symptoms occurred leading the oncologist to discover metastatic disease.

During a Targeted Oncology Case-Based Roundtable event, Erminia Massarelli, MD, PhD, MS, codirector, Lung Cancer and Thoracic Oncology Program, and associate clinical professor in the Department of Medical Oncology & Therapeutics Research at the City of Hope Comprehensive Cancer Center, discussed the case of a 58-year-old patients with RET-mutant medullary thyroid cancer.
Targeted OncologyTM: What is the frequency of RET mutations and fusions in patients with MTC and papillary thyroid cancer [PTC] and treatment options?
MASSARELLI: The frequency of RET mutations and fusions in MTC is as high as 90%. But don’t forget, MTC is a rare cancer. PTC occurs more frequently; however, the RET mutations and fusions are found in [only] 10% to 20% of patients with PTC.1
According to the National Comprehensive Cancer Network [NCCN] guidelines, the preferred regimens for asymptomatic, RET mutation–positive MTC are selpercatinib [Retevmo] and pralsetinib [Gavreto]. For MTC without RET mutation, the NCCN recommends vandetanib [Caprelsa] and cabozantinib [Cometriq].2 It’s very important to check the RET status because not every instance of MTC has [a RET] mutation.
What data support the use of vandetanib for advanced or metastatic MTC?
The ZETA trial [NCT00410761] was a phase 3 trial that compared vandetanib [300 mg/d] vs placebo for advanced or metastatic MTC among 331 randomized patients. There was a statistically significant advantage for treatment with vandetanib; the objective response rate [ORR] was 45% [odds ratio (OR), 5.48; 95% CI, 2.99-10.79; P < .001] and the disease control rate was 87% [OR, 2.64; 95% CI, 1.48- 4.69; P = .001]. The biochemical response [rates were also] significant, with reduction in both calcitonin, among 69% of patients [OR, 72.9; 95% CI, 26.2-303.2; P < .001] and CEA, among 52% of patients [OR, 52.0; 95% CI, 16.0-320.3; P < .001]. The best outcome [with respect to progression-free survival (PFS)] was among RET mutation–positive patients; we know that [vandetanib is not only] a VEGF inhibitor but also a RET inhibitor. The overall survival [OS] data were immature at data cutoff.3
Among the observed adverse events [AEs] of any grade, diarrhea occurred in 56% of the vandetanib group vs 26% of the placebo group, and hypertension occurred in 32% vs 5% of the respective groups. Among AEs of grade 3 or higher, QT prolongation occurred in 8% vs 1%; fatigue, in 6% vs 1% of the respective groups.3
What data support the use of cabozantinib for metastatic MTC?
The EXAM trial [NCT00704730] was a phase 3 trial of cabozantinib vs placebo among 330 randomized patients. There was an ORR of 28% with cabozantinib and 0% with placebo [P < .001].⁴ The ORR was 34% among patients whose tumors tested positive for the RET M918T mutation and 20% among the M918T-negative subgroup. So [cabozantinib] is still a good option for patients who cannot go on RET-specific inhibitors. [Additional analyses showed that] the M918T-positive subgroup exhibited significant benefit with respect to median PFS [13.9 months with cabozantinib vs 4.0 months with placebo; HR, 0.15; 95% CI, 0.08-0.28; P < .0001] and median OS [44.3 months with cabozantinib vs 18.9 months with placebo; HR, 0.60; 95% CI, 0.38-0.94; P = .03]. The M918T-negative subgroup did not exhibit significant benefit with respect to either PFS or OS.5 So you see that cabozantinib also has a RET-inhibitory activity.
The toxicity profile was similar to that of vandetanib. In the experimental arm vs the control arm, AEs of any grade included diarrhea [in 70.1% vs 35.8% of the respective groups], decreased weight [57.9% vs 11.0%], decreased appetite [49.1% vs 15.6%], nausea [46.7% vs 21.1%], and fatigue [42.5% vs 30.3%]. Liver toxicity and rash also occurred; however, [the majority of these were grade 2 or lower].⁵ There was palmar-plantar erythrodysesthesia, which occurred in 52.8% of patients treated with cabozantinib and in 1.8% of patients who received placebo. This is a syndrome in which the hands and feet become red and [develop] hyperkeratotic lesions. Some of my patients could not even walk anymore because of this problem, especially at a higher dose.
The patients in the experimental arm of this trial started treatment at 140 mg per day; 82% had 1 dose reduction and 46% underwent a second dose reduction. [In my experience], 40 mg per day [is a tolerable dosage] for cabozantinib.
in RET-mutant MTC and RET fusion–positive thyroid cancer?
The LIBRETTO-001 trial [NCT03157128] analyzed selpercatinib in RET-mutant MTC and RET fusion–positive thyroid cancer. [The primary analysis set consisted of] 55 patients with RET-mutant MTC and prior treatment with cabozantinib, vandetanib, or both; 35% were female and 65% were male. The majority had an ECOG performance status of 0 or 1; only 5% of patients had a status of 2. Regarding prior treatment, 44% of these patients were treated with both cabozantinib and vandetanib, 24% had received only cabozantinib, and 33% had received only vandetanib. Fifty-three percent of patients had previously received 2 or more multikinase inhibitors and 31% had received prior nonmultikinase systemic therapy. Only 7% of the patients had brain metastases; MTC and PTC don’t have high incidences of brain metastasis. Measurable disease was present in 96% of patients. The most common RET mutation was the M918T mutation, present in 60% of patients. The second most common mutation was the extracellular cysteine mutation [13%], [followed by] the V804M/L mutation [9%].6
The ORR in the 55 previously treated MTC patients was 69% [95% CI, 55%-81%]; of these, 60% had partial responses, which was really amazing. The median duration of response [DOR] was not estimable [NE; 95% CI, 19.1- NE]; [likewise], the median PFS was NE [95% CI, 24.4-NE]. Among 88 patients with RET-mutant MTC not previously treated [with cabozantinib or vandetanib], 73% [95% CI, 62%-82%] had an objective response; of these, 61% had a partial response. The median DOR was 22.0 months [95% CI, NE-NE] and the median PFS was 23.6 months [95% CI, NE-NE]. Among 19 patients with previously treated RET fusion–positive thyroid cancer, 79% [95% CI, 54%-94%] had an objective response. The median DOR was 18.4 months [95% CI, 7.6-NE] and the median PFS, 20.1 months [95% CI, 9.4-NE]. [Finally], all 8 patients with RET fusion– positive thyroid cancer that was not previously treated had a response; the median DOR was NE.7 The waterfall plots of maximum change in tumor size [show similar trends] among patients with previously treated and previously untreated RET-mutant MTC and among patients with previously treated RET fusion–positive thyroid cancer. [In all groups], the majority responded.6
There were AEs, of course; treatment-related AEs of any grade were experienced by 94% of patients and AEs of grade 3, by 28%.6 However, the toxicity profile of sel-percatinib, when compared with that of cabozantinib or vandetanib, was significantly better. For example, because selpercatinib is a RET-specific inhibitor, patients didn’t have as much diarrhea of any grade, [which occurred in 17% of treated patients]. [Also], their skin rash was better, [occurring in 8% of treated patients]. There was also nausea [in 15% of patients] and vomiting [in 7%], but [neither was] grade 3 or 4. There was liver toxicity of grade 3 in 7% to 10% of patients. [Regarding the diarrhea, in my experience], patients who start with high calcitonin have this diarrhea, which is related to the decreasing calcitonin. Then once the calcitonin goes really low, the diarrhea disappears. These patients might have grade 2 or grade 3 diarrhea at the beginning, but then after a few months on selpercatinib, the diarrhea resolves. That happened for 2 of my patients, and it’s now been almost 2 years.
What data support the use of pralsetinib for RET-mutant MTC?
The ARROW trial [NCT03037385] was a phase 1/2 trial of pralsetinib for RET-mutant MTC. The patients had advanced tumors [and they were subdivided into cohorts] as well. There was a 67-patient cohort with RET-mutant MTC previously treated with cabozantinib, vandetanib, or both; a 42-patient cohort with RET-mutant MTC without prior systematic treatment; and a 10-patient cohort with RET-mutant MTC and previous systemic treatment other than cabozantinib or vandetanib. Finally, there was a 319-patient cohort representing other [RET-altered tumors].8,9
The majority of patients in the RET-mutant cohorts were male and White [with an] ECOG performance status of 0 or 1.9 Central nervous system metastases were present in 7% of the group previously treated with cabozantinib, vandetanib, or both and in 14% of the cabozantinib- and vandetanib-naive group.8,9 The previously treated group had received a median of 2 prior lines of therapy, with a range of 1 to 7. Among the cabozantinib- and vandetanib-naive group, 28% had received up to 3 lines of prior therapy, 10% had received anti–PD-1 or PD-L1 inhibitors, 3.4% had received kinase inhibitors, and 10% had received radioactive iodine. These are most likely patients who were on prior clinical trials.
The ORR among patients with RET-mutant MTC previously treated with cabozantinib or vandetanib was 60% [95% CI, 46%-73%], and in the naive cohort it was 66% [95% CI, 46%-82%]. The complete response rate was 1.8% among the previously treated patients and 10% in the naive cohort. The respective partial response rates were 58% and 55%. Median DOR was not reached in either cohort, but a DOR of at least 6 months was achieved in 79% of the previously treated cohort and 84% of the naive cohort.10
[The AEs among 138 treated patients included] hypertension, of course; remember, this is still a RET inhibitor. Hypertension of any grade occurred in 40% of patients; 21% of patients experienced hypertension of grade 3 or grade 4. [Other AEs of grade 3 and 4 included] fatigue, in 6% of patients; diarrhea, in 5%; pyrexia, in 2.2%; and dyspnea, in 2.2%. This is similar to [what was observed with] selpercatinib.9
Pralsetinib was approved by the FDA for RET-altered thyroid cancer.10 The new label [includes mention of] tumor lysis syndrome.9
REFERENCES:
1. Subbiah V, Cote GJ. Advances in targeting RET-dependent cancers. Cancer Discov. 2020;10(4):498-505. doi:10.1158/2159-8290.CD-19-1116
2. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 1.2021. Accessed August 10, 2021. https://bit.ly/3j5gYN2
3. Wells SA Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134-141. doi:10.1200/JCO.2011.35.5040
4. Elisei R, Schlumberger MJ, Müller SP, et al. Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol. 2013;31(29):3639-3646. doi:10.1200/ JCO.2012.48.4659
5. Schlumberger M, Elisei R, Müller S, et al. Overall survival analysis of EXAM, a phase III trial of cabozantinib in patients with radiographically progressive medullary thyroid carcinoma. Ann Oncol. 2017;28(11):2813-2819. doi:10.1093/annonc/mdx479
6. Wirth LJ, Sherman E, Robinson B, et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med. 2020;383(9):825-835. doi:10.1056/ NEJMoa2005651
7. Retevmo. Prescribing information. Lilly USA, LLC; 2021. Accessed August 10, 2021. https://bit.ly/3CWorWK
8. Hu MI, Subbiah V, Wirth L, et al. Results from the registrational phase I/II ARROW trial of pralsetinib (BLU-667) in patients (pts) with advanced RET mutation–positive medullary thyroid cancer (RET + MTC). Ann Oncol. 2020;31(suppl 4):S1084. doi:10.1016/j.annonc.2020.08.1401
9. Gavreto. Prescribing information. Genentech USA, Inc and Blueprint Medicines Corporation; 2021. Accessed August 11, 2021. https://bit.ly/3gjDOin
10. FDA approves pralsetinib for RET-altered thyroid cancers. FDA. December 1, 2020. Accessed August 11, 2021. https://bit.ly/3kd9Uxk
Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen