Abstract
Praziquantel pharmacokinetics studies in schistosomiasis infected children are scarce partly due to the challenges/complexity of intensive blood sampling in the target population. This study was aimed to investigate the optimal single sampling time-point for monitoring praziquantel exposure. This was intensive pharmacokinetic study conducted among 32 Schistosoma mansoni infected children treated with an oral standard single-dose 40 mg/kg praziquantel. Plasma samples were collected at 0, 1, 2, 4, 6 and 8 h post-praziquantel administration. Quantification of praziquantel and its enantiomers (R- and S-praziquantel) concentrations was done by Liquid chromatography-tandem mass spectrometer (LC–MS/MS). The correlation between area under the plasma concentration–time curve from 0 to 8 h (AUC8) and plasma concentrations at each specific sampling time-point was determined by Pearson’s correlation coefficient (r2). The median age (range) of the study population was 12.5 years (10–17). The study participants were 17 males and 15 females. Both total praziquantel and its enantiomers (R- and S-praziquantel) displayed a wide inter-individual pharmacokinetic variability. Regression analysis indicated that, plasma concentrations collected at 4 h post-dose had a significantly highest correlation with the AUC8 for both total praziquantel (r2 = 0.81, p < 0.001) and S-praziquantel (r2 = 0.84, p < 0.001) than any other sampling time-point; while for R-praziquantel, plasma concentrations collected at 6 h sampling time-point had a significantly highest correlation with the AUC8 (r2 = 0.79, p < 0.001) than any other sampling time-point. Four hours sampling time-point post-praziquantel administration is ideal optimal single sampling time-point for therapeutic monitoring of total praziquantel exposure while 6 h sampling time-point is suitable for monitoring of a pharmacologically active R-praziquantel enantiomer.
Similar content being viewed by others
Introduction
Schistosomiasis is still a public health challenge in Sub-Saharan Africa (SSA). The disease causes significant morbidity and mortality especially among children in endemic countries1. Over 250 million people are infected with schistosomiasis worldwide and children are the most affected2. Preventive chemotherapy by mass praziquantel administration targeting school children is the core control strategy implemented in endemic countries and > 90% of those requiring treatment for schistosomiasis live in SSA3. Despite the repeated rounds of mass praziquantel administration, schistosomiasis remain a public health problem in SSA including Tanzania4,5.
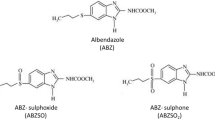
Praziquantel is a pyrazino-isoquinoline derivative, which has a rapid and complete absorption (> 80%) following its administration. Its systemic bioavailability is usually low and varies between individuals6. Praziquantel is distributed throughout the body and is highly bound to plasma protein (about 80%), mostly to albumin6. It undergoes an extensive enantioselective first pass metabolism in the liver by cytochrome P450 (CYP450) enzymes including CY3A4/5, CYP2C19, CYP2C9 and CYP1A2 to form several hydroxylated metabolites6,7. The major metabolite in humans is trans-4-hydroxylated praziquantel, which possess antischistosomal activity8. The fact that praziquantel metabolism is entirely via CYP450, its pharmacokinetics is susceptible to variability due to inter-individual pharmacogenetics differences and also risk of drug–drug interactions6.
Praziquantel treatment has been associated with varying cure rates, incidence, and profile of adverse events9,10,11. This is partly due to the fact that praziquantel displays a wide inter-individual variability in its pharmacokinetic parameters in the population12. The reported adverse events following praziquantel treatment have been linked to an increased risk of treatment non-compliance in the target population and hence low treatment coverage13. High incidence of adverse events and variability in praziquantel plasma concentration necessitate the need for assessing praziquantel exposure following treatment11. Additionally, praziquantel displays limited efficacy against juvenile worms14 and a threat of drug resistance has been reported in previous studies9. Therefore, the need for an alternative treatment regimen for the treatment and control of schistosomiasis is imminent. Recently, a combination of praziquantel and dihydroartemisinin-piperaquine produced superior efficacy than praziquantel alone for the treatment of schistosomiasis15. Furthermore, the combination of praziquantel and dihydroartemisinin-piperaquine produced an increased systemic praziquantel exposure without affecting the overall safety in the target population16. On the other hand, low praziquantel plasma levels have been reported in healthy volunteers who received co-administration of anti-tuberculous drugs and praziquantel17, and therefore, this drug–drug interaction may result into poor treatment efficacy in patients. Drug–drug interactions can affect systemic praziquantel levels and hence cure rate, incidence, and profile of adverse events11. Drug–drug interactions resulting from both the use of combination chemotherapy and concomitant drugs administration further warrants the need for monitoring of praziquantel exposure, particularly in children18.
To study the performance and safety of praziquantel in individual patients and during mass drug administration (MDA), its systemic exposure or bioavailability needs to be examined. Area under the concentration–time curve (AUC) is a pharmacokinetic parameter used to reflect the systemic bioavailability or exposure of the drug. Currently, intensive blood sampling at different time-points post-praziquantel administration is common practice used in pharmacokinetic studies and in clinical trials to determine the AUC and maximum plasma concentration achieved (Cmax) as markers of systemic drug exposure12,17,19,20. However, intensive blood sampling is challenging not only to researchers but also to study participants who are mostly children21,22. Furthermore, the amount of blood needed to be withdrawn during entire sampling period partly accounts for the most stress and anxiety experienced by the children.
In other infectious diseases such as malaria, single time-point plasma sample collected at day 7 has been well established to predict the long-acting antimalarial drug exposure and cure at 28 days follow-up23,24,25. Similarly, single blood sample collected at 2 h post-drug administration, better reflects the systemic exposure of an immunosuppressive cyclosporine and better predicts clinical outcomes of the patients in organ transplant26.
The antischistosomal activity of praziquantel is correlated to its systemic exposure (i.e., AUC) rather than Cmax achieved6,12. To calculate AUC, multiple blood sampling following drug administration is required to estimate the full concentration–time curve. However intensive sampling at a given time interval from all children at the same time present ethical and practical barriers. Therefore, plasma concentration collected at a single sampling time-point which better correlates with the AUC can serve as a surrogate marker for praziquantel systemic bioavailability and can predict schistosomiasis treatment outcomes. The optimal single sampling time-point will also mitigate the challenges of intensive blood sampling and hence increases praziquantel exposure monitoring following treatment, particularly among children27. To our knowledge, no study has investigated an optimal single sampling time-point as a surrogate marker to accurately predict systemic praziquantel exposure in children infected with trematodes or cestodes infections for which praziquantel is a treatment of choice. The present study examined the optimal single sampling time-point as a surrogate marker of praziquantel bioavailability monitoring in children.
Results
Patient’s and baseline characteristics
A total of 32 Schistosoma mansoni infected children were treated with an oral standard single dose praziquantel (40 mg/kg) and completed this study. The study participants were 17 males and 15 females. The median age (range) of the study population was 12.5 years (10–17). The median weight and height of the study participants were 32.5 kg and 140.9 cm, respectively. Most of the children had moderate to heavy Schistosoma mansoni infection (Table 1).
Pharmacokinetics of praziquantel and its enantiomers in the study population
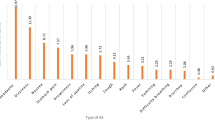
Changes in total praziquantel and its enantiomers plasma concentrations was monitored at 0, 1, 2, 4, 6 and 8 h after drug administration. The pharmacokinetics parameters of total praziquantel, R-praziquantel and S-praziquantel are presented in Table 2. The Cmax in ng/mL for both total praziquantel and enantiomers were achieved at 3.5 h post-dose. The AUC8 for total praziquantel was 1254.4 ng h/mL. The AUC8 for S-praziquantel was higher than that for R-praziquantel (Table 2). There was a wide inter-individual variability in pharmacokinetic parameters of both total praziquantel and its enantiomers as presented in Table 2 and Fig. 1.
Correlation between plasma concentrations at different sampling time-points and AUC8
The r2 values were calculated for the correlation between plasma concentrations collected at each specific time-point (ng/mL) and AUC8 (ng h/mL) (Fig. 2). According to the regression analysis, the r2 values varied significantly across the plasma concentrations collected at different sampling time-points for both total praziquantel and its enantiomers (Figs. 2, 3). The r2 values of the plasma concentrations collected at 4 h sampling time-point for total praziquantel (r2 = 0.81, p < 0.001) and S-praziquantel (r2 = 0.84, p < 0.001) were significantly higher than the rest of the sampling time-points. For R-praziquantel, the r2 value of the plasma concentration collected at 6 h sampling time-point were significantly higher than the rest of the sampling time-points (r2 = 0.79, p < 0.001) (Figs. 2, 3).
Discussion
We investigated the optimal single sampling time-point for monitoring of praziquantel exposure among schistosomiasis infected children who were treated with single dose praziquantel. Intensive blood sampling over several hours is a common practice in pharmacokinetics studies and clinical trials for the assessment of praziquantel exposure12,19,20. Lack of single optimal blood sampling time-point for monitoring of the praziquantel exposure partly contributes to the scarcity of pharmacokinetic data among treated children. The antischistosomal activity of praziquantel depends on the drug exposure i.e. AUC6; therefore, sampling time point whose plasma concentrations better correlate with AUC would serve as a pharmacokinetic marker for monitoring praziquantel bioavailability. In malaria treatment using artemisinin-based combination therapy (ACTs), plasma concentrations collected at day 7 for piperaquine or lumefantrine is a marker of antimalarial drug exposure and a predictor of malaria cure25. In this study, intensive blood samples were collected at 0, 1, 2, 4, 6 and 8-h post-drug administration, and the AUC8 was calculated.
The key findings from the present study include (1) both total praziquantel and its enantiomers display a wide inter-individual variability in pharmacokinetic parameters and (2) plasma concentrations collected at 4 h post-praziquantel administration had a significantly highest correlation (r2 value) with AUC8 than any other time-points for total praziquantel while plasma concentrations collected at 6 h post-praziquantel had a significantly highest correlation (r2 value) with AUC8 for a pharmacologically active R-praziquantel. To the best of our knowledge, this is the first study to examine the optimal single sampling time-point for monitoring of praziquantel and its enantiomers exposure in children.
In this study, both total praziquantel and its enantiomers exhibited a wide pharmacokinetic variability (Fig. 1) similar to reports from previous studies12,19. Based on the literature, most of the praziquantel pharmacokinetics variability is unexplained12. However, factors such as differences in age and weights of the study participants (mostly children), food effect, intestinal diseases, and a wide spectrum of CYP450 metabolizing enzymes involved in biotransformation of praziquantel (extensive first pass effect), including CYP3A, CYP1A2, CYP2C9 and CYP2C19 have been speculated12,19. CYP enzymes relevant for praziquantel metabolism display wide between-individual and population variation in enzyme activities partly due to pharmacogenetics variations28,29,30 and also display an enantioselective catalytic activity7. The difference in CYP enzymes catalytic activity towards praziquantel enantiomers may also account for the observed pharmacokinetics variability. Therefore, there is a need for pharmacogenetics studies of praziquantel and its relevance on plasma concentrations among treated children11.
Our study show that plasma concentrations collected at 4 h post-dose is the best single sampling time-point for therapeutic drug monitoring of total praziquantel exposure among treated children. The Pearson’s correlation coefficient (r2 value) between plasma concentrations collected at 4 h post-dose and AUC8 was significantly higher than any other sampling time-point (r2 = 0.81) (Figs. 2, 3). The 4-h post dose sampling point also corresponds well to the T-max for total, R- and S-praziquantel. Therefore, based on these findings, the 4 h sampling time-point following praziquantel administration can be used as a marker of systemic drug exposure or bioavailability among treated children (Fig. 1). The use of this single sampling time-point will mitigate the challenges of intensive blood sampling for assessment of praziquantel exposure especially in children21,22.
On the other hand, for R-praziquantel, plasma concentrations collected at 6 h post-dose had significantly higher correlation with AUC8 than any other sampling time-point (r2 = 0.79) (Figs. 2, 3). Therefore, for studies targeting R-praziquantel, plasma samples collected at 6 h post-dose gives the best correlation with AUC and would be a suitable single sampling time-point for monitoring of its exposure following praziquantel administration. R-praziquantel is the pharmacologically active enantiomer and contributes to the antischistosomal activity of praziquantel11,19. Recently, there has been a move to produce a monoenantiomeric R-praziquantel formulation for the treatment and control of schistosomiasis in children11. R-praziquantel formulation will reduce the tablet size and also the bitter taste of the drug that were contributed by the S-praziquantel31 and hence better treatment compliance among children. Once the R-praziquantel formulation is approved for use, a 6-h post-dose sampling time-point is ideal for assessing its systemic exposure following administration.
Future praziquantel pharmacokinetic studies should focus on calculating the cut-off point for the plasma concentrations at 4 h sampling time-point for total praziquantel and 6 h sampling time-point for R-praziquantel in order to predict the clinical outcome of schistosomiasis treatment (i.e. cure rate) at 14–21 days follow-up according to the WHO guidelines32 and other parasitic infections of which praziquantel is a treatment of choice. In malaria treatment using ACTs, a cut off ≥ 200 ng/mL of day 7 lumefantrine concentration is associated with malaria cure at 28 days follow-up25.
PZQ is co-administered with albendazole for the control and treatment of intestinal schistosomiases and soil transmitted helminths (STH) respectively in MDA campaign to all school-age children without prior screening in endemic areas. In our study, participants were screened for intestinal schistosomiases as having Schistosoma mansoni infection was the inclusion criteria. Participants were not screened for STH, and this may be considered as study limitation. Although our study finding reflect the practical situation in sub-Saharan Africa where STH and schistosomiasis are co-endemic, STH co-infection may possibly influence PZQ metabolism. As the study participants had heavy-to-moderate Schistosoma mansoni infection intensity, any impact of STH co-infection on hepatic PZQ metabolism may be insignificant but cannot be ruled out. Therefore, the impact of STH coinfection on PZQ pharmacokinetics in co-infected children remains to be explored in controlled large sample size studies.
In conclusion, since monoenantiomeric R-praziquantel formulation is not yet approved for clinical use, plasma concentrations collected at 4 h post-dose is the ideal optimal single sampling time-point for monitoring of praziquantel bioavailability in children infected with cestodes and trematodes including schistosomiasis, where praziquantel is a treatment of choice.
Materials and methods
Study design and population
This was a single-arm pharmacokinetic study aimed at examining the optimal single sampling time-point suitable for monitoring of praziquantel bioavailability during treatment of schistosomiasis in children. A total of 32 Schistosoma mansoni infected children (aged 10–17 years) were recruited in this study between May 2017 and January 2018. The enrolled participants were randomly selected from a parallel study assessing the efficacy and safety of single dose praziquantel (40 mg/kg body weight) for the treatment of intestinal schistosomiasis33. Hemoglobin concentration (Hb conc) was determined from finger prick blood sample using a HemoCue Hb 201+ machine (HemoCue AB Angelholm, Sweden) to exclude participants with severe anemia (defined as Hb conc < 8 g/dL). As intensive pharmacokinetic study requires multiple blood sampling, laboratory tests that required additional blood sampling such us liver and kidney function test and complete blood count were not done for ethical reasons (to reduce the number and volume of blood samples collected from children, a vulnerable population). However, clinical and physical examinations (i.e. jaundice, edema, pallor etc.) were done before treatment to ensure that the participants had no liver or kidney problems or any other chronic diseases.
Ethical approval for this study was obtained from the National Institute for Medical Research, Dar es Salaam, Tanzania (Ref. No. NIMR/HQ/R.8a/Vol.IX/2343), Muhimbili University of Health and Allied Sciences Institutional Review Board (Ref. No.2016-5-25/AEC/Vol.X/03) and Stockholm Ethics Committee (Ref. No. 2020-00845). This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from parents/guardians and assent from eligible children.
Stool samples examination
Two fresh stool samples were collected and analyzed by Kato-Katz technique for screening of Schistosoma mansoni infection both at pre- and post-treatment as reported previously4,33. Infection intensity was categorized as light infection (epg 1–99), moderate infection (epg 100–399) and heavy infections (epg ≥ 400)4.
Therapeutic procedures and blood sampling
Following a pre-treatment meal, study participants were treated with an oral single dose 40 mg/kg body weight of praziquantel (Praziquantel 600 mg/tablet, Batch BZ6043, S Kant Health Care Ltd, India) as a direct observed treatment (DOT)33. Food has been shown to increase the bioavailability of praziquantel6. After drug administration, serial blood samples (2 mL) were collected at 0, 1, 2, 4, 6 and 8 h from each participant using an indwelling sterile catheter inserted and maintained in the forearm vein. The withdrawn blood samples in heparinized tubes were immediately centrifuged at 1000 rpm for 10 min to obtain plasma, and aliquots were kept at − 80 °C freezer until analyzed.
Chemicals and reagents
Racemic (rac) praziquantel was obtained from Merck (Darmstadt, Germany). An 11-fold rac-deuterated-praziquantel (rac-praziquantel-d11) as an internal standard, R-praziquantel and S-praziquantel were purchased from Toronto Research Chemicals (Toronto, Ontario, Canada). Chemicals such as acetone, acetonitrile, ammonium acetate, isopropanol, methanol, and acetic acid of mass spectrometry (MS) grade were acquired from Merck (Darmstadt, Germany). Ultrapure MilliQ water was prepared using a Milli-Q water purification system (Merck Millipore, MA, USA). Blank human plasma was supplied by the local blood bank of the Karolinska University Hospital Huddinge (Stockholm, Sweden).
Quantification of R- and S-praziquantel
Quantification of plasma concentrations of R- praziquantel, and S-praziquantel was done using LC/MS/MS as described previously16. Briefly, plasma calibration samples were freshly prepared by spiking blank plasma samples with rac-praziquantel and were included in each analytical run. Quality control (QC) samples were also prepared by spiking plasma blanks with known concentrations to obtain low (QCL), medium (QCM), and high (QCH) samples for both R-praziquantel and S-praziquantel. The quantification range of the method was 1–1500 ng/mL for both R-praziquantel and S-praziquantel.
For extraction of analytes of interest, 100 µL of plasma samples went through protein precipitation with 200 µL of internal standard solution (50 ng/mL of rac-praziquantel-d11 in methanol) and then vortexed for 10 s followed by centrifugation for 5 min at 2100×g. Thereafter, 150 µL of the supernatant was diluted with 75 µL MilliQ water and 5 µL was injected into the LC–MS/MS system. The chromatographic system was using a Chiralpak AGP 2.0 × 100 mm, 5 µm, column (Chiral Technologies Europe, Illkirch, France) with 10 mM ammonium acetate: isopropanol 98:2 (v/v) pH 8 as mobile phase with a flow rate of 0.3 mL/min. The chromatographic run was 22 min, and with use of the parallel two channel capacity, injection to injection time was 11 min. R-Praziquantel eluted first followed by S-praziquantel with a difference of 1.9 min. Total praziquantel concentrations were obtained by adding R-praziquantel and S-praziquantel final concentrations. The analytical method was validated according to the European Medicines Agency Guideline on bioanalytical method validation34.
Pharmacokinetic analysis
Noncompartmental analysis (NCA) with linear trapezoidal rule was used to calculate pharmacokinetics parameters using R statistical software version 4.0.235. The primary and secondary pharmacokinetic parameters for R-praziquantel, S-praziquantel and total praziquantel were calculated including maximum plasma concentration (Cmax) in ng/mL, time needed to reach Cmax (Tmax) in hours, area under the concentration–time curve from 0 h to infinity (AUC∞, ng × h/mL), area under the concentration–time curve from 0 to 8 h post-dose (AUC8, ng × h/mL) and terminal half-life (t1/2) in hours. Cmax, Tmax, t1/2, AUC8, and AUC∞ were directly calculated from the pharmacokinetics raw data using the PKNCA package version 0.9.4 implemented in R36.
Statistical data analysis
Statistical data analysis was performed by R software. Results were summarized as mean ± standard deviations (SD) or median (interquartile range—IQR) for continuous variables and proportions for categorical variables. The log-transformed plasma concentrations and calculated AUC8 were dose-normalized by dividing the values with dose received by each participant. Pearson’s correlation coefficient (r2) was used to determine the correlation between praziquantel and its enantiomers plasma concentrations at each specific sampling time-point and AUC8. Sampling time-point with significantly highest r2 value than any other time-point was considered as an optimal single sampling time-point for monitoring of praziquantel bioavailability in children.
Ethical approval
The study was reviewed and approved by the National Institute for Medical Research, Dar es Salaam, Tanzania (Ref. No. NIMR/HQ/R.8a/Vol.IX/2343), Muhimbili University of Health and Allied Sciences Institutional Review Board (Ref. No. 2016-5-25/AEC/Vol.X/03) and Stockholm Ethics Committee (Ref. No. 2020-00845). All participants received comprehensive information about the study and provided written informed consent (parents/guardians) and assent (eligible children) for participating in the study.
Data availability
All relevant data presented in this work are contained within the manuscript.
References
Hotez, P. J. et al. The global burden of disease study 2010: Interpretation and implications for the neglected tropical diseases. PLoS Negl. Trop. Dis. 8, e2865. https://doi.org/10.1371/journal.pntd.0002865 (2014).
Mazigo, H. D. Participatory integrated control strategies and elimination of schistosomiasis in sub-Saharan Africa. Lancet Glob. Health 7, e998–e999. https://doi.org/10.1016/s2214-109x(19)30271-2 (2019).
World Health Organization, Geneva (2013). Schistosomiasis: Progress report 2001–2011, strategic plan 2012–2020. https://www.who.int/schistosomiasis/resources/9789241503174/en/. Accessed 6 Nov 2019.
Mnkugwe, R. H., Minzi, O. S., Kinung’hi, S. M., Kamuhabwa, A. A. & Aklillu, E. Prevalence and correlates of intestinal schistosomiasis infection among school-aged children in North-Western Tanzania. PLoS One 15, e0228770. https://doi.org/10.1371/journal.pone.0228770 (2020).
Gebreyesus, T. D. et al. Prevalence, intensity, and correlates of schistosomiasis and soil-transmitted helminth infections after five rounds of preventive chemotherapy among school children in Southern Ethiopia. Pathogens (Basel, Switzerland) https://doi.org/10.3390/pathogens9110920 (2020).
Olliaro, P., Delgado-Romero, P. & Keiser, J. The little we know about the pharmacokinetics and pharmacodynamics of praziquantel (racemate and R-enantiomer). J. Antimicrob. Chemother. 69, 863–870. https://doi.org/10.1093/jac/dkt491 (2014).
Wang, H. et al. Metabolic profiling of praziquantel enantiomers. Biochem. Pharmacol. 90, 166–178. https://doi.org/10.1016/j.bcp.2014.05.001 (2014).
Kovač, J., Vargas, M. & Keiser, J. In vitro and in vivo activity of R- and S-praziquantel enantiomers and the main human metabolite trans-4-hydroxy-praziquantel against Schistosoma haematobium. Parasit. Vectors 10, 365. https://doi.org/10.1186/s13071-017-2293-3 (2017).
Gryseels, B. et al. Are poor responses to praziquantel for the treatment of Schistosoma mansoni infections in Senegal due to resistance? An overview of the evidence. Trop. Med. Int. Health 6, 864–873. https://doi.org/10.1046/j.1365-3156.2001.00811.x (2001).
Coulibaly, J. T. et al. Efficacy and safety of praziquantel in preschool-aged and school-aged children infected with Schistosoma mansoni: A randomised controlled, parallel-group, dose-ranging, phase 2 trial. Lancet Glob. Health 5, e688–e698. https://doi.org/10.1016/s2214-109x(17)30187-0 (2017).
Zdesenko, G. & Mutapi, F. Drug metabolism and pharmacokinetics of praziquantel: A review of variable drug exposure during schistosomiasis treatment in human hosts and experimental models. PLoS Negl. Trop. Dis. 14, e0008649. https://doi.org/10.1371/journal.pntd.0008649 (2020).
Bustinduy, A. L. et al. Population pharmacokinetics and pharmacodynamics of praziquantel in Ugandan children with intestinal schistosomiasis: Higher dosages are required for maximal efficacy. MBio https://doi.org/10.1128/mBio.00227-16 (2016).
Bergquist, R. & Gray, D. J. Schistosomiasis elimination: Beginning of the end or a continued march on a trodden path. Trop. Med. Infect. Dis. https://doi.org/10.3390/tropicalmed4020076 (2019).
Inobaya, M. T., Olveda, R. M., Chau, T. N., Olveda, D. U. & Ross, A. G. Prevention and control of schistosomiasis: A current perspective. Res. Rep. Trop. Med. 65–75, 2014. https://doi.org/10.2147/rrtm.S44274 (2014).
Mnkugwe, R. H., Minzi, O., Kinung’hi, S., Kamuhabwa, A. & Aklillu, E. Efficacy and safety of praziquantel and dihydroartemisinin piperaquine combination for treatment and control of intestinal schistosomiasis: A randomized, non-inferiority clinical trial. PLoS Negl. Trop. Dis. 14, e0008619. https://doi.org/10.1371/journal.pntd.0008619 (2020).
Minzi, O. M. et al. Effect of dihydroartemisinin-piperaquine on the pharmacokinetics of praziquantel for treatment of Schistosoma mansoni infection. Pharmaceuticals 14, 400. https://doi.org/10.3390/ph14050400 (2021).
Ridtitid, W., Wongnawa, M., Mahatthanatrakul, W., Punyo, J. & Sunbhanich, M. Rifampin markedly decreases plasma concentrations of praziquantel in healthy volunteers. Clin. Pharmacol. Ther. 72, 505–513. https://doi.org/10.1067/mcp.2002.129319 (2002).
Utzinger, J., Keiser, J., Shuhua, X., Tanner, M. & Singer, B. H. Combination chemotherapy of schistosomiasis in laboratory studies and clinical trials. Antimicrob. Agents Chemother. 47, 1487–1495. https://doi.org/10.1128/aac.47.5.1487-1495.2003 (2003).
Kovač, J. et al. Pharmacokinetics of praziquantel in Schistosoma mansoni- and Schistosoma haematobium-infected school- and preschool-aged children. Antimicrob. Agents Chemother. https://doi.org/10.1128/aac.02253-17 (2018).
Meister, I. et al. Pharmacokinetic study of praziquantel enantiomers and its main metabolite R-trans-4-OH-PZQ in plasma, blood and dried blood spots in opisthorchis viverrini-infected patients. PLoS Negl. Trop. Dis. 10, e0004700. https://doi.org/10.1371/journal.pntd.0004700 (2016).
Barker, C. I. S. et al. Pharmacokinetic studies in children: Recommendations for practice and research. Arch. Dis. Child. 103, 695–702. https://doi.org/10.1136/archdischild-2017-314506 (2018).
Howie, S. R. Blood sample volumes in child health research: Review of safe limits. Bull. World Health Organ. 89, 46–53. https://doi.org/10.2471/blt.10.080010 (2011).
World Health Organization. Methods and techniques for assessing exposure to antimalarial drugs in clinical field studies. Geneva, 2011. http://www.who.int/malaria/publications/atoz/9789241502061/en/. Accessed 09 Mar 2021.
White, N. J., van Vugt, M. & Ezzet, F. Clinical pharmacokinetics and pharmacodynamics and pharmacodynamics of artemether-lumefantrine. Clin. Pharmacokinet. 37, 105–125. https://doi.org/10.2165/00003088-199937020-00002 (1999).
Kilonzi, M. et al. Usefulness of day 7 lumefantrine plasma concentration as a predictor of malaria treatment outcome in under-fives children treated with artemether-lumefantrine in Tanzania. Malar. J. 19, 66. https://doi.org/10.1186/s12936-020-3150-y (2020).
Jia, Y. et al. Optimal sampling time-point for cyclosporin A concentration monitoring in heart transplant recipients. Exp. Ther. Med. 16, 4265–4270. https://doi.org/10.3892/etm.2018.6711 (2018).
Reed, M. D. Optimal sampling theory: An overview of its application to pharmacokinetic studies in infants and children. Pediatrics 104, 627–632 (1999).
Mutagonda, R. F. et al. Effect of pharmacogenetics on plasma lumefantrine pharmacokinetics and malaria treatment outcome in pregnant women. Malar. J. 16, 267. https://doi.org/10.1186/s12936-017-1914-9 (2017).
Mugusi, S. et al. Impact of population and pharmacogenetics variations on Efavirenz pharmacokinetics and immunologic outcomes during anti-tuberculosis co-therapy: A parallel prospective cohort study in two Sub-Sahara African populations. Front. Pharmacol. 11, 26. https://doi.org/10.3389/fphar.2020.00026 (2020).
Ahmed, J. H. et al. Population pharmacokinetic, pharmacogenetic, and pharmacodynamic analysis of cyclophosphamide in Ethiopian breast cancer patients. Front. Pharmacol. 11, 406. https://doi.org/10.3389/fphar.2020.00406 (2020).
Meyer, T. et al. Taste, a new incentive to switch to (R)-praziquantel in schistosomiasis treatment. PLoS Negl. Trop. Dis. 3, e357. https://doi.org/10.1371/journal.pntd.0000357 (2009).
World Health Organization, Geneva (2013). Assessing the efficacy of anthelminthic drugs against schistosomiasis and soil-transmitted helminthiases. https://apps.who.int/iris/handle/10665/79019. Accessed 6 Nov 2019.
Mnkugwe, R. H., Minzi, O. S., Kinung’hi, S. M., Kamuhabwa, A. A. & Aklillu, E. Efficacy and Safety of praziquantel for treatment of Schistosoma mansoni infection among school children in Tanzania. Pathogens (Basel, Switzerland) https://doi.org/10.3390/pathogens9010028 (2019).
European Medicine Agency. Guideline on bioanalytical method validation EMEA/CHMP/EWP/192217/2009 Rev. 1 Corr. 2. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-bioanalytical-method-validation_en.pdf. Accessed 10 Mar 2021.
R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, V., Austria. https://www.R-project.org/
Denney, W. D. S. & Buckeridge, C. Simple, automatic noncompartmental analysis: The PKNCA R package. J. Pharmacokinet. Pharmacodyn. 42(1), 11–107. https://doi.org/10.1007/s10928-015-9432-2 (2015).
Acknowledgements
We convey our sincere thanks to the National Institute for Medical Research, Mwanza Research Centre staff for their support on sample collection, processing, and storage. We thank the study participants (parents/guardians and children) who participated in this study.
Funding
Open access funding provided by Karolinska Institute. The study received financial support from the Swedish International Development Cooperation Agency (Sida) for capacity building at Muhimbili University of Health and Allied Sciences (MUHAS) as a part of bilateral collaboration between Sweden and Tanzania, and European and Developing Countries Clinical Trials Partnership (EDCTP) 2 program, supported by the European Union (Grant number CSA2016S-1618).
Author information
Authors and Affiliations
Contributions
Protocol development and project design: R.H.M., O.M.S., S.M.K., A.A.K., and E.A.: data collection: R.H.M., O.M.S., S.M.K., A.A.K., and E.A.: data analysis: R.H.M., O.M.S., E.N., S.M.K., A.A.K., and E.A.: project supervision: O.M.S., S.M.K., A.A.K., and E.A.: writing first draft manuscript: R.H.M.: review and editing of the manuscript: O.M.S., E.N., S.M.K., A.A.K., and E.A.: finally, all authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mnkugwe, R.H., Ngaimisi Kitabi, E., Kinung’hi, S. et al. Optimal single sampling time-point for monitoring of praziquantel exposure in children. Sci Rep 11, 17955 (2021). https://doi.org/10.1038/s41598-021-97409-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-97409-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.