The latest studies of health needs in Fort Bend County identify barriers preventing many residents from accessing quality physical and mental health care, and local providers are expanding to meet the demand.
Various Fort Bend County entities conducted a series of community health studies and surveyed 800 individuals throughout 2022 to form the county’s 2022 Community Health Assessment report.
The CHA report released April 21 found that access to health care needed to be improved for many residents in the county; survey respondents said the two primary barriers to accessing health care were an inability to pay for care out of pocket and a lack of health insurance.
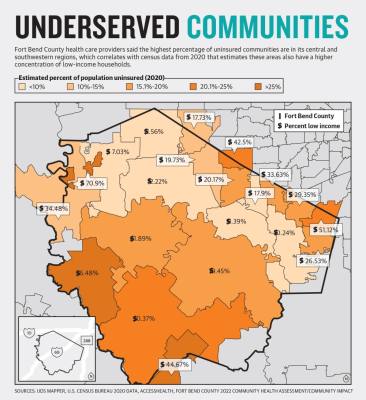
Areas north of Richmond, parts of Houston and the more rural areas in the county see uninsured population rates higher than 20%, said Kaila Williams, Fort Bend County’s director of health communications, equity and engagement.
Overall, 17% of adults and 11% of children were uninsured in the county in 2022, with the percentage of uninsured people reaching over 16% in the 77498 and 77489 Sugar Land and Missouri City ZIP Code Tabulation Areas in 2020. These ZCTAs—which are generalized representations of United States Postal Service ZIP code service areas—are located in the northeast part of the county near the city of Houston.
“Twenty-two percent of [CHA] respondents, they or a family member needed medical care in the past year but was unable to receive it,” she said. “The top reason was because they did not have health insurance.”
Williams also indicated 45% of respondents said free or low-cost medical services were the top missing services in their community. However, some local health clinics that provide low-cost services are undergoing expansions in areas with larger uninsured and low-income populations.
Identifying needs
Survey data and anecdotal accounts from health care officials that indicate household income and pandemic-era health trends point providers in the direction of the people who are most in need of support.
Fort Bend County overall has a lower percentage of uninsured people in its population than in the state, which has the highest population and percentage of uninsured residents in the nation, according to the Texas comptroller’s website. The ratio of providers to patients has improved over time in the county, but statewide trends—such as many essential labor employers not providing health care to workers—are also present in Fort Bend County.
In the CHA report, 25 “key informants” were consulted to represent different sectors and populations, such as primary health care providers, elected officials and hospitals.
These informants were asked to assess the health status of Fort Bend County residents. According to the report, the assessed individuals generally identified people with insurance and higher socioeconomic status as being relatively healthy, while people without insurance or with a low annual household income—or making less than $40,000—tended to have unmet health needs.
The observations made by informants were supported in the county’s health report. Only 29% of people with a low annual household income reported having “very good” health versus 41%-53% of people with middle and high annual household incomes.
Local nonprofit health care providers that cater to low income and uninsured populations, such as San Jose Clinic and AccessHealth, are expanding to better serve high-demand areas in the county.
San Jose Clinic aims to provide quality care and education to people with constraints keeping them from accessing health care. Kimberlyn Clarkson, chief advancement officer for San Jose Clinic, said chronic conditions were exacerbated over the course of the COVID-19 pandemic among patients. She said managing chronic conditions, such as diabetes and hypertension, is the current focus for the majority of San Jose Clinic patients.
“When a patient or person goes without consistent health care for a number of years, things like diabetes arise,” Clarkson said. “Chronic conditions often lead to other chronic conditions. So I start off with diabetes, then end up with some pancreatic and liver issues, maybe even heart issues.”
Meanwhile, AccessHealth, which has been based in Fort Bend and Waller counties for almost 50 years, serves its communities by not turning anyone away for a lack of ability to pay or a lack of insurance.
Data from AccessHealth showed an increase in the number of mental health or substance abuse visits since the onset of the COVID-19 pandemic in 2020. According to the data, there were 8,681 of these visits in 2022, reflecting a 45.68% jump from 5,959 visits in 2020.
“These figures indicate an elevated demand for mental health services, potentially influenced by the ongoing effects of the pandemic and the current global landscape,” an emailed statement from AccessHealth reads.
The CHA’s section relating to mental health needs in the county states there is one mental health provider for every 1,050 Fort Bend County residents, compared to one provider per 690 residents in the state overall.
“We’ve seen an increase in suicide ideation at our Fort Bend clinic since the start of the pandemic,” Clarkson said in regards to San Jose Clinic patients. “We think that isolation could play a factor in that.”
Barriers to care
The CHA report identified a variety of social barriers preventing residents from accessing quality care. Outside of being uninsured or underinsured, factors such as a lack of transportation and a lack of bilingual providers were key contributors, according to the CHA. An underinsured person is someone with insurance that may not sufficiently cover their medical needs.
“One of the No. 1 barriers for people dealing with health care is transportation,” Clarkson said. “In our area, where a county can span 100 miles like Harris County, having reliable transportation to get to and from the doctor is quite a challenge for underserved and under-resourced people.”
Clarkson said often people seeking care without reliable transportation would need to have a family member take them to a clinic. In these cases, both could be missing out on work hours with no paid time off benefits, she said.
AccessHealth Chief Population Health Officer Palak Jalan referred to the factors preventing people from accessing care as “social determinants of health.” She also indicated a lack of adequate transportation as one of these factors, while highlighting an inability to access healthy food, pay utility bills or generally find employment.
A lack of employment opportunities and low wages can cause many residents to deprioritize health care over housing and food, according to observations made in the CHA.
“[People] want to work, they want to take care of their families, they want to contribute to society—but they work in jobs that are not required to offer them benefits,” Clarkson said.
Meeting demand
Clarkson said San Jose is working to “bridge the trust gap” in areas around the Rosenberg community that they serve, especially people in more rural areas and people from marginalized communities.San Jose Clinic is planning to open a pharmacy in Rosenberg over the summer. The pharmacy will help provide services to places in the county with the highest demand, Clarkson said. It will be located at 117 Lane Dr. in the Quadrangle Square.
“We’re always thinking about growth in the Fort Bend area,” Clarkson said. “We’re looking at ... finding a funder that can help us secure our own land and our own space.”
Jalan said AccessHealth has plans to expand its presence in Missouri City and is also considering future expansions into west areas of the county and the Katy area, where Jalan said there is high demand. A timeline for the projects was not provided.
Jalan said being medically underserved is a multidimensional problem affecting Fort Bend County communities. She said systems-based changes or changes to governing policy outside of clinics tend to be overlooked methods for taking on the challenge.
“Access to green spaces, sidewalks, ... things that we would [usually] associate with civic infrastructure, have a big impact on health and well-being,” Jalan said.